Abstract
Objective:
To assess the difference in resource utilisation between lithium and valproate treatment groups from the VALID study.
Methods:
A modelled economic study was conducted as an appendage to the VALID study, an international, randomised, open-label, parallel-group, 12-week, equivalence study in patients with bipolar I disorder experiencing a manic/mixed episode, compared the efficacy and safety of valproate against that of lithium. The difference in health resource utilisation between the treatment groups was analysed based on information collected from a standardised questionnaire.
Results:
Efficacy and tolerability of valproate and lithium were shown to be comparable in the management of bipolar disorder in the VALID study. Cost analysis was based on information for 138 (35.5% male, mean age: 37.73 years) and 131 (45.8% male, mean age: 38.98 years) patients from lithium and valproate treatment groups, respectively. The groups differed in the number of hospital visits (503 vs. 421), outpatient visits (15 vs. 2), and number of work days lost (907 vs. 514.5) due to bipolar disorder. All differences were in favour of the valproate treatment group. In the modelled analysis and subsequent sensitivity analyses, the total cost saving was calculated to be US$199,322 (range: US$37,629–$226,903). This would translate into a cost saving of US$1444 per patient, or a cost saving of US$6278 per patient per year (range: US$1185–$7145 per patient per year).
Limitations:
The present study suffers from the limitations inherent in any economic evaluation that uses data from multicentre clinical trials with potential variations in treatment provision as well as the theoretical bias from an open-label study design. The study sample size had also limited statistical power to detect moderate differences in total medical costs, given the large variances often observed on cost variables.
Conclusions:
The use of valproate over lithium is likely to result in substantial cost savings to the healthcare system and reduce the financial burden to patients.
Introduction
Bipolar I disorder is a serious and persistent disorder characterised by unpredictable episodes of mania, hypomania, mixed mood, major depression, and euthymia. It is a relatively common psychiatric disorder with frequent relapses, and a lifetime prevalence of 1%Citation1.
In 1991, the economic burden of bipolar disorder in the United States (US) was estimated to be $7 billion in direct medical costs and $38 billion in indirect costsCitation2. The average lifetime treatment cost per patient is thought to range from $11,720 for patients with a single manic episode to $624,785 for patients with non-responsive/chronic episodesCitation3. It was reported that patients with bipolar disorder had annual medical costs that were four times those of patients without bipolar disorderCitation4.
Lithium and valproate are two rigorously studied pharmacologic treatments for acute mania in bipolar I disorderCitation5. Lithium was the first mood-stabilising medication approved by the US Food and Drug Administration in the 1970s for the treatment of mania, and is a recommended and established first-line therapy for the treatment of manic episodes in bipolar diseaseCitation6. Valproate is also recommended as an appropriate first-line treatment of acute mania in international practice guidelinesCitation6–9. Several studies have shown the comparable efficacy and safety of lithium and valproateCitation10,Citation11. The sustained antimanic activity of valproate in bipolar disorderCitation10–12 was further confirmed by the VALID study, which showed that valproate and lithium have comparable efficacy and tolerability in the treatment of acute mania over 12 weeksCitation13.
Although both valproate and lithium are very commonly prescribed, few pharmacoeconomic studies have compared their cost effectiveness for the treatment of bipolar disorder. Moreover, published studies to date have largely been limited to North American populationsCitation14–16. To extend these observations to other populations, the VALID study was performed in six Eastern European and South East Asian countries to compare the effectiveness of valproate and lithium treatment in bipolar disorderCitation13. The current study was designed as a pragmatic trial in order to determine medical costs in conditions which closely resembled standard clinical practice and would therefore be broadly generalisable.
Methods
Study design
The current study utilised cost data collected from the VALID Study. VALID was an international, multicentre, randomised, open-label, parallel-group, equivalence study of 12 weeks’ duration comparing sodium valproate with lithium in bipolar patients suffering from a manic episode. The study was conducted in 21 centres in six countries/regions (Bulgaria, Hong-Kong, Malaysia, Russia, Taiwan and Thailand) between January 2004 and February 2006Citation1Citation3. The study procedures, treatments administered and statistical analyses to compare the efficacy and tolerability of lithium and valproate are detailed in an earlier paperCitation13.
The analysis of the difference in health resource utilisation outcomes between the valproate and lithium treatment groups was based upon the information collected from the standardised questionnaire used in all the studied sites in the various countries and regions for the VALID study. As well as socio-demographic information, the questionnaire captured information relating to direct costs such as hospital visits, clinic visits and visits to other health professionals and information relating to indirect costs such as days of lost productivity.
Patient sample
The study included in- and out-patients aged from 18 to 75 years with a current diagnosis of bipolar I disorder according to the DSM IV TR criteriaCitation17 and currently experiencing a manic or mixed episode. Patients were required to have experienced at least one manic episode within the previous 3 years. For patients over 60 years of age at the screening visit, a previous manic episode before the age of 60 regardless of the inter-episode interval was acceptable. For patients under 30 years of age, newly diagnosed patients were also eligible.
A total score on the Young Mania Rating Scale (YMRS)Citation18, of 18 or higher was required at screening and baseline. Women of childbearing age were required to be using an effective method of contraception. Patients with antecedents of intolerance to valproate or lithium, comorbidities or treatments that might interfere with the implementation or interpretation of the study, or clinically relevant abnormalities in biochemical, haematological or electrocardiographic parameters were ineligible. Additionally, patients who had participated in a clinical trial within the previous 3 months, currently fulfilled DSM-IV diagnostic criteria for alcohol or substance dependence or substance abuse or who were judged by the investigator to be at serious risk of suicide were excluded from the study.
For this pharmacoeconomic study, 131 and 138 evaluable patients were included in the valproate and lithium groups, respectively.
Ethics approvals
The study was conducted according to the Declaration of Helsinki (Hong Kong Amendment)Citation19, Good Clinical Practices (European Guidelines)Citation20, and pertinent national legal and regulatory requirements. Written informed consent was obtained from each patient. Patients were free to withdraw from the study at any time for any reason, without effect on their medical care. The protocol was submitted to and approved by the appropriate local and national ethics committee in each country/region.
Modelling to estimate cost difference between the two treatments
The initial step taken for the analysis was to retrieve relevant information relating to resource consumption from the consolidated report. The next step involved assigning costs to both direct (e.g., hospital visits) and indirect (e.g., days of lost productivity) resource consumption identifying the major differences between the two treatment groups. The final step involved establishing a model that would estimate the cost difference between the valproate and lithium treatment groups in all the participating countries and regions in the VALID study.
In assigning cost to the quantity of healthcare utilisation and days lost at work, it was decided to adopt an approach that would allow data to be generalised across all the participating countries and regions in the VALID Study. That is, the cost difference was to be calculated for all the participating countries and regions first as a weighted average for the group and then applied to individual countries and regions. However, due to the unavailability of reliable scheduled fee information from, as well as due to, differences in the structure of the healthcare systems in all the participating countries and regions of the VALID study, in the modelling of the direct cost differences between the two groups, the analysis adopted an approach in estimation of resource consumption which was somewhat akin to the common comparator approach used in economic evaluation.
In the estimation of indirect cost difference between the two groups, it was necessary to obtain a ratio against a source where costs for healthcare services and average salary are readily available from an official source. The ratios used for the modelling study were the per capita gross domestic product (GDP) adjusted for purchasing power parity (PPP) from the CIA World Fact BookCitation21. Data from Australia were used for this purpose to make the comparison meaningful across all countries and regions. To calculate the weighted average for the whole group, equal weightage was assigned to each country and region as they had similar prevalence of bipolar disorder. The average per capita GDP for the group adjusted by PPP was US$18,633.
The next step was to find information for fees for hospital visits, admissions and specialist physician professional fees. The most robust data which are readily available are from the website of the Department of Health and Ageing, Commonwealth of Australia. The information was obtained from Medicare Benefits Schedule, November 2007 versionCitation22 and AR-DRG version 5.0Citation23. To increase the generalisability of the results, only those items that would likely to be applicable to all participating countries and regions of the VALID study were retrieved. The exchange rate used was as on November 13, 2007: US$ 1 = Aus$ 1.126Citation24.
For estimation of the indirect cost, average weekly earnings of Aus$852.30 (US$758.04) for Australian employees in 2006 were takenCitation25. Based on a 40-hour (5-day) working week, the daily earning would be Aus$170.46 (US$151.61).
There were three basic assumptions: first, a correction (multiplication by 138/131 = 1.05) was used to adjust for the difference in sample size between the two treatment groups in determining per patient hospital visits and in outpatient visits etc.; second, 55% of hospital visits would eventually be treated as inpatients (reflecting the study population – 54% and 59% of the valproate and lithium patients, respectively were treated as inpatients); and third, the salary of bipolar patients was the same as that of the general population.
Based on certain assumptions (made on the basis of observations from the information of the consolidated report of the VALID study), the potential cost savings for valproate over lithium were calculated and a series of sensitivity analyses were undertaken to test these assumptions.
Sensitivity analysis
One-way sensitivity analyses were performed by assuming the best-case and worst-case scenarios. To be realistic, the worst-case scenario in this analysis would assume that all cases involved in inpatient care incurred the highest costs and that 30% of episodes in outpatient care would be initial consultations. The indirect cost component would remain unchanged. For the best-case scenario, it would be assumed that all hospital episodes were outpatient follow-up episodes while the rest of the other components remained unchanged.
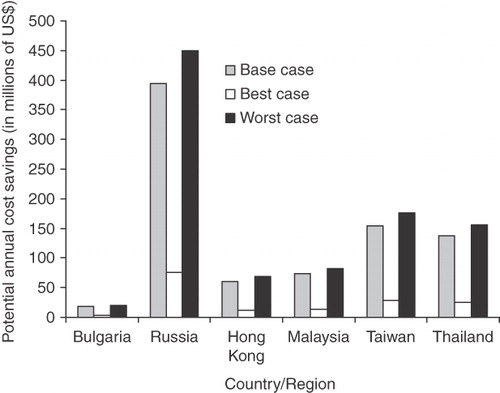
Estimation of total annual savings if lithium is totally replaced by valproate
For each country/region, the cost difference was multiplied by the prevalence rate of bipolar disorder and the total population of the country/region to provide an estimate of the cost savings from using valproate over lithium in the management of bipolar disorder. For the prevalence, a rate of 1–2% (using a mid-point value of 1.5%) was assumedCitation1. Another assumption was that only 20% of patients with bipolar disorder would be using lithium. Again, sensitivity analyses were conductedCitation26,Citation27.
Results
Baseline characteristics
From the consolidated report from the VALID study, information for 131 patients (45.8% male, mean age: 38.98 years) from the valproate treatment group and138 patients (35.5% male, mean age: 37.73 years) from the lithium treatment group was available for the economic analysis. Generally speaking, the subjects participating in the study were very similar in terms of employment status (51.2 vs. 50% unemployed or retired in the valproate and lithium treatment groups, respectively), proportion being treated as inpatients (53.4 vs. 58.7% in the valproate and lithium treatment groups, respectively), and number of patients reporting loss of productivity >50% due to bipolar disorder (10 vs. 11 in the valproate and lithium treatment groups, respectively).
Healthcare utilisation
The main differences in healthcare utilisation and financial burden between the two treatment groups were in the number of hospital visits, outpatient visits, and the number of work days lost due to bipolar disorder. The differences were all in favour of the valproate treatment group ().
Table 1. Difference in resource utilisation between valproate and lithium treatment groups of the VALID study.
After adjusting for the slight difference in the number of patients between the two groups, the differences in hospital visits, outpatient visits and work days lost due to bipolar disorders were 61 episodes, 12.9 episodes and 366.8 days, respectively. This means that on average, each patient treated in the lithium group would incur an extra 0.44 episodes of hospital visits, 0.09 episodes of outpatient visits and 2.64 work days lost due to bipolar disorders compared to patients treated in the valproate group (). As the final assessment day of the study was at day 84, the values would represent an extra 0.005 episodes of hospital stay per patient per day, 0.001 episodes of outpatient visits per patient per day and 0.03 extra work days lost per patient on lithium treatment when compared to valproate treatment ().
Cost savings and sensitivity analyses
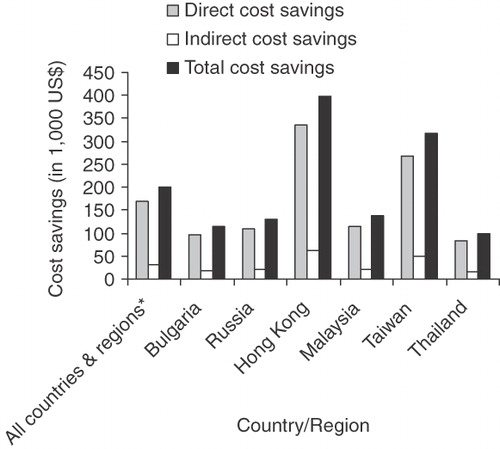
Based on the modelling assumptions, we obtained a difference in hospital visits of 33.55 episodes and a difference of 40.45 episodes of outpatient management between the two treatment groups, yielding a direct cost difference of US$300,321. Likewise, the indirect cost difference between the two treatment groups was valued as US$55,611. Hence, the total cost difference between the two treatment groups worked out to be US$355,932.
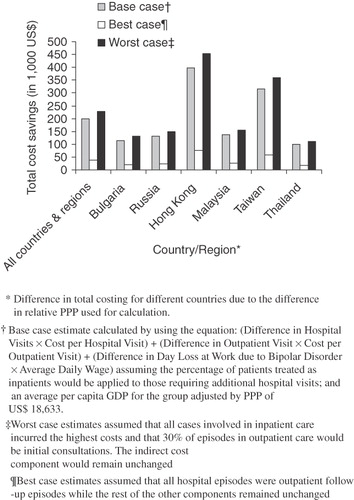
To convert this value for the countries and regions participating in the VALID study, this value was multiplied by a factor of 0.56 (18,633/33,000), calculated from the ratio of GDP per capita of the group as compared to Australia. Thus, in the base-case analysis, the total cost saving was calculated to be US$199,322 (). This would translate into a cost saving of US$1444 per patient, or a cost saving of US$6278 per patient per year as the final assessment day was at day 84.
Figure 1. Cost savings for participating countries or regions of the VALID study (adjusted by PPP). Weighted average value of all participating countries/regions (not the sum of all countries), hence the total cost of all countries may be lower than some individual countries or regions where the PPP are much higher, e.g. Hong Kong and Taiwan.
The results of the sensitivity analyses showed the total cost savings in the best- and worst-case scenarios were US$ 37,629 and US$226,903, respectively (). This would amount to a cost saving of US$1185 and US$7145 per patient per year in the best- and worst-case scenarios, respectively. The best- and worst-case scenarios of potential cost savings assuming that all patients suffering from bipolar disorder were on lithium and were to switch over to valproate are summarised in . Based on the results, it is evident that each country could make substantial savings if all bipolar disorder patients on lithium were switched to valproate.
Discussion
In this study, to estimate the difference in resource utilisation between the valproate and lithium treatment groups of the VALID study, we found that the key difference between the two groups was in the number of hospital visits (direct medical costs) and the number of work days lost due to bipolar disorders (indirect costs). The difference in number of hospital visits would directly impact on the healthcare system; however, to have a comprehensive estimation of the burden of the disease to the society for any disease management, especially for the case of psychiatric diseases, the indirect cost needs also to be considered as this could be substantial. In our study, for both the direct and indirect costs, the differences were all in favour of the valproate group.
There are two assumptions that could potentially affect the results of our study. These assumptions are: (1) that 55% of hospital visits would eventually be treated as inpatients, and (2) the salary of bipolar patients is the same as that of the general population. The assumption that of the hospital visits, 55% of the cases were eventually treated as inpatients and 45% as outpatients was based upon the proportion shown by the VALID studyCitation13. This was assumed to reflect the treatment pattern for all groups, and this assumption has been tested in the sensitivity analysis. Finally, the assumption that the salary of bipolar patients is the same as the general population resulted from a lack of information about the average salary of bipolar patients. Hence, based on the principle of non-discrimination, it was assumed that the use of the same average salary as that of the general population would reflect the concept of ‘opportunity cost’ loss. Nevertheless, as demonstrated by the results of the sensitivity analyses, both assumptions only affect the magnitude but not the direction of the cost difference between the two treatment groups.
In the 12-week study, valproate was associated with a cost saving of approximately US$1445 per patient with bipolar disorder. This is comparable to the savings of about US$1700 per patient with bipolar disorder in the divalproex-treated group compared to the lithium group in an earlier 1-year-long studyCitation28. The magnitude of savings in our study is likely significant for the healthcare system. For example, in a healthcare system with 5000 patients with bipolar disorder, treatment with valproate may be associated with about US$7.3 million in savings.
Medication adherence is associated with hospitalisation and medical costsCitation29. Differences between agents that lead to differences in compliance may have important implications on treatment outcomes. For example, differences in the side-effect profile of agents may affect patients’ ability to continue treatment. In the study by Revicki et al., fewer divalproex-treated patients discontinued medication due to lack of efficacy or side-effects than did lithium-treated patientsCitation28. In another clinical trial, there were also fewer treatment discontinuations due to intolerance or non-compliance in the divalproex-treated group compared with the lithium-treated groupCitation10. In the VALID study, however, there was no significant difference in the proportion of patients discontinuing treatment in the valproate and lithium treatment groups (6.2 vs. 5.8%)Citation13. Hence, it is noteworthy that even with a comparable side-effect profile, valproate was found to be more cost effective than lithium.
The present study suffers from the limitations inherent in any economic evaluation that uses data from multicentre clinical trials, such that variations in treatment provision can be difficult to map to treatment provision in any single country. The open-label design would theoretically introduce a number of possible biases. Nevertheless, randomisation should to some extent reduce the potential for inclusion bias, and indeed the two treatment groups were well-balanced with respect to the demographic and clinical variables evaluated at baseline. Finally, the study sample size had limited statistical power to detect moderate differences in total medical costs, given the large variances often observed on cost variables. Larger sample sizes (i.e., 300–500 subjects per group) are typically required to evaluate differences in medical costsCitation30. However, the consistency in the observed difference in both direct and indirect costs in favour of valproate treatment arm would support that this trend is unlikely to be an artefact due to chance.
From the analyses performed, the results of this pragmatic, randomised study suggest that the use of valproate over lithium in the management of bipolar disorder is likely to result in substantial cost savings to the healthcare system while also reducing the financial burden to patients.
Transparency
Declaration of funding
This study was supported financially by Sanofi-Aventis.
Declaration of financial/other relationships
Professor Li has worked as a consultant/advisor to the VALID study and Dr Aggarwal is an employee of Sanofi-Aventis.
Acknowledgements
The authors would also like to acknowledge the efforts and contributions of members of the VALID Study Group in various countries/regions for collection of the health resource utilisation data used in the current study. Special acknowledgment to Dr. Tini Nyugen for organising the data collection process.
References
- Merikangas KR, Akiskal HS, Angst J, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry 2007;64:543-52
- Wyatt RJ, Henter I. An economic evaluation of manic-depressive illness – 1991. Soc Psychiatry Psychiatr Epidemiol 1995;30:213-19
- Begley CE, Annegers JF, Swann AC, et al. The lifetime cost of bipolar disorder in the US: an estimate for new cases in 1998. Pharmacoeconomics 2001;19:483-95
- Bryan-Comstock L, Stender M, Devercelli G. Health care utilization and costs among privately insured patients with bipolar I disorder. Bipolar Disorder 2002;4:398-405
- Keck PE Jr, Nabulsi AA, Taylor JL, et al. A pharmacoeconomic model of divalproex vs. lithium in the acute and prophylactic treatment of bipolar I disorder. J Clin Psychiatry 1996;57:213-22
- American Psychiatric Association. Practice guideline for the treatment of patients with bipolar disorder (revision). Am J Psychiatry 2002;159(4):1-50
- Goodwin GM. Evidence-based guidelines for treating bipolar disorder: recommendations from the British Association for Psychopharmacology. J Psychopharmacol 2003;17,149-73
- Yatham LN, Kennedy SH, O'Donovan C, et al; Guidelines Group, CANMAT. Canadian Network for Mood and Anxiety Treatments (CANMAT) guidelines for the management of patients with bipolar disorder: update 2007. Bipolar Disord 2006;8:721-39
- Grunze H, Kasper S, Goodwin G, et al. The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders, Part II: Treatment of Mania. World J Biol Psychiatry 2003;4:5-13
- Bowden CL, Calabrese JR, McElroy SL, et al. A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry 2000;57:481-9
- Bowden C, Göğüş A, Grunze H, et al. A 12-week, open, randomized trial comparing sodium valproate to lithium in patients with bipolar I disorder suffering from a manic episode. Int Clin Psychopharmacol 2008;23:254-62
- Zajecka JM, Weisler R, Sachs G, et al. A comparison of the efficacy, safety, and tolerability of divalproex sodium and olanzapine in the treatment of bipolar disorder. J Clin Psychiatry 2002;63:1148-55
- Bowden CL, Mosolov S, Hranov L, et al. Efficacy of valproate versus lithium in mania or mixed mania: a randomized, open 12-week trial. Int Clin Psychopharmacol 2010;25:60-7
- Keck PE Jr, McElroy EL, Bennett JA. Health-economic implications of the onset of action of antimanic agents. J Clin Psychiatry 1996;57(13), 13-18
- Revicki DA, Matza LS, Flood E, et al. Bipolar disorder and health-related quality of life: review of burden of disease and clinical trials. Pharmacoeconomics 2005;23:583-94
- Dalkilic A, Diaz E, Baker CB, et al. Effects of divalproex versus lithium on length of hospital stay among patients with bipolar disorder. Psychiatr Serv 2000;51:1184-6
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, (4th edn) Text Revision. Washington DC: American Psychiatric Association, 2000
- Young RC, Biggs JT, Ziegler VE, et al. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 1978;133:429-35
- World Medical Association. Declaration of Helsinki, 3rd (Hong Kong) amendment, 1989
- European Medicines Agency. ICH Topic E 6 (R1) Guideline for Good Clinical Practice. CPMP/ICH/135/95, 2002
- Central Intelligence Agency. The World Factbook. Available at: https://www.cia.gov/library/publications/the-world-factbook/index.html. Accessed: December 5, 2009
- Australian Government Department of Health and Aging. MBS Online: Medicare Benefits Schedule. Available at: http://www.health.gov.au/internet/mbsonline/publishing.nsf/Content/Medicare-Benefits-Schedule-MBS-1 Accessed: December 5, 2009
- Australian Government Department of Health and Aging. Australian Refined Diagnosis Related Groups (AR-DRGs). Available at: http://www.health.gov.au/internet/main/publishing.nsf/Content/health-casemix-ardrg1.htm. Accessed: April 1, 2010
- Universal Currency Converter. Available at: http://www.xe.com/ucc/convert.cgi Accessed: November 13, 2007
- Australian Bureau of Statistics. Employee earnings and hours. 6306.0. Available at: http://www.ausstats.abs.gov.au/Ausstats/subscriber.nsf/0/284EA51F2E7BD8F9CA25728F000D10AC/$File/63060_May%202006.pdf Updated: March 8, 2007. Accessed December 5, 2009
- Müller-Oerlinghausen B, Berghöfer A, Bauer M. Bipolar disorders. Lancet 2002;359:241-6
- Fountoulakis KN, Vieta E, Sanchez-Moreno J, et al. Treatment guidelines for bipolar disorder: A critical review. J Affect Disord 86;2005:1-10
- Revicki DA, Hirschfield RMA, Ahearn EP, et al. Effectiveness and medical costs of divalproex versus lithium in the treatment of bipolar disorders: results of a naturalistic clinical trial. J Affect Disord 2005;86:183-93
- Svarstad BL, Shireman TI, Sweeny JK. Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatr Serv 2001;52:805-11
- Health Care Consultants of America, Inc. Physicians Fee and Coding Guide: A Comprehensive Fee and Coding Reference. Augusta, GA: MAG Mutual Group, 1997