Abstract
Objective:
Benefits of anti-coagulation for venous thromboembolism (VTE) prevention in total hip and knee arthroplasty (THA/TKA) may be offset by increased risk of bleeding. The aim was to assess in-hospital risk of VTE and bleeding after THA/TKA and quantify any increased costs.
Methods:
Healthcare claims from the Premier PerspectiveTM Comparative Hospital Database (January 2000–September 2008) were selected for subjects ≥18 years with ≥1 diagnosis code for THA/TKA. VTE was defined as ≥1 code for deep vein thrombosis or pulmonary embolism. Bleeding was classified as major/non-major. Incremental in-hospital costs associated with VTE and bleeding were calculated as cost differences between inpatients with VTE or bleeding matched 1:1 with inpatients without VTE or bleeding.
Results:
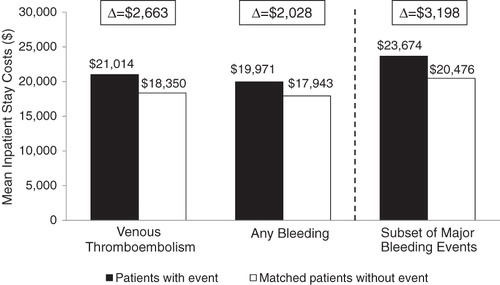
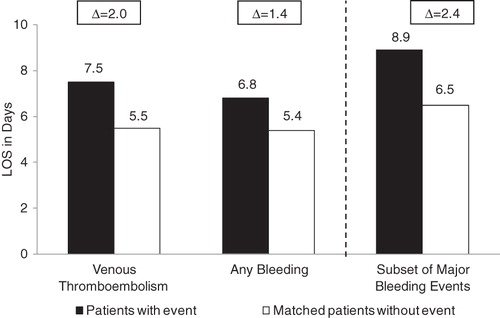
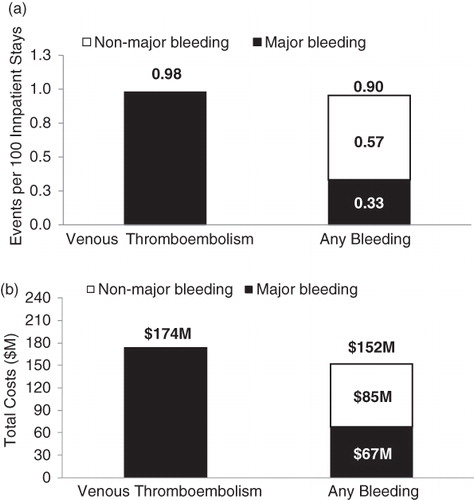
A total of 820,197 inpatient stays were identified: 8042 had a VTE event and 7401 a bleeding event (2740 major bleeding). The risks of VTE, any bleeding, and major bleeding were 0.98, 0.90, and 0.33/100 inpatient stays, respectively. Mean incremental in-hospital costs per inpatient were $2663 for VTE, $2028 for bleeding, and $3198 for major bleeding.
Limitations:
These included possible inaccuracies or omissions in procedures, diagnoses, or costs of claims data; no information on the amount of blood transfused or decreases in the hemoglobin level to evaluate bleeding event severity; and potential biases due to the observational design of the study.
Conclusions:
In-hospital risk and incremental all-cause costs with THA/TKA were higher for VTE than for bleeding. Despite higher costs, major bleeding occurred less frequently than VTE, suggesting a favorable benefit/risk profile for VTE prophylaxis in THA/TKA.
Introduction
Despite advances in prophylactic measures to prevent venous thromboembolism (VTE), its components—deep vein thrombosis (DVT) and pulmonary embolism (PE)—are associated with considerable mortality and morbidity in the US, where they result in ∼600,000 hospitalizations and 300,000 deaths per yearCitation1. VTE is the second most common medical complication, the second most common cause of excess hospital length of stay (LOS), and the third most common cause of excess mortality, while PE is the most common preventable cause of hospital deathCitation2. The prognosis for patients with VTE is characterized by the risk of recurrent events or post-thrombotic syndrome, and for patients with PE, by pulmonary hypertensionCitation3.
VTE is a frequent complication after total hip arthroplasty (THA) and total knee arthroplasty (TKA)Citation2, possibly due to direct trauma in the deep veinsCitation4. Approximately half of the patients who undergo TKA or THA surgery without prophylaxis develop DVT, and 1–2% develop PE, which in 25% of cases results in sudden deathCitation5,Citation6. The risk of DVT after THA has been reported to be 5–20% in patients receiving adequate thromboprophylaxisCitation7. In 2007, there were more than 1 million hospital discharges with a primary diagnosis of TKA or THA, with aggregate costs totaling over $15.6 billionCitation8. It is estimated that by 2030 the number of THAs could reach 572,000 and the number of TKAs could reach 3.48 million annuallyCitation9.
Consequently, VTE imposes a substantial financial burden on the healthcare system, and long-term costs associated with VTE complications after THA or TKA are significant. Several studies have attempted to quantify the cost of VTE complicationsCitation6,Citation10–12. Median annualized all-cause reimbursed costs for patients with DVT or PE were reported to be ∼$17,512 and $18,901, respectively, compared to $680 for control patients without DVT or PECitation13. The mean all-cause cost of recurrent VTE events requiring hospitalization was estimated at $12,326 (DVT: $11,419; PE: $11,014; DVT + PE: $19,237)Citation14.
The benefit of using anti-coagulation therapy for the prevention of VTE is counterbalanced by the potential increased risk of bleeding. Therefore, assessment of the risk and cost of VTE and its prevention must also take into consideration the risk of bleeding. When results from five large clinical trials were pooled, rates of major bleeding after THA were 3.3% in patients receiving vitamin K antagonists and 5.3% in patients receiving low molecular weight heparin (LMWH)Citation2. After TKA, major bleeding was found to occur in 2.7% of patients receiving vitamin K antagonists, compared to 4.5% in patients receiving LMWHCitation2. Estimates of costs of management of an episode of major bleeding have been reported to range from $113–$5355 per patientCitation15,Citation16.
The goals of this study were to assess the in-hospital risk of developing VTE and bleeding in patients after THA or TKA surgery and to quantify the costs associated with VTE and bleeding. The choice to focus solely on the in-hospital period following THA and TKA was motivated by the high risk of developing VTE and bleeding events before hospital dischargeCitation17.
Patients and methods
Data source
The Premier PerspectiveTM Comparative Hospital Database (PREMIER) was used to conduct the current study. Because the PREMIER database includes records collected directly from the hospitals’ cost accounting systems, as opposed to insurers’ billing systems, it offers one of the richest and most reliable sources of claims-based inpatient cost data. De-identified inpatient records were retrieved retrospectively from the PREMIER database between January 2000 and September 2008. This database provides detailed information for more than 25 million inpatient discharges from over 500 acute-care hospitals across all US regions. Data elements by setting include claim-level information, including primary and secondary diagnoses and procedures, and detailed billing information.
Study design
A retrospective cohort design was used to evaluate the in-hospital risk of developing VTE or bleeding, including the sub-set of major bleeding events, in patients undergoing THA or TKA, while a matched-cohort design was used to quantify increased costs associated with VTE or bleeding. To be included in the study sample, patients were required to meet the following criteria: (a) at least one claim with a primary or secondary procedure code for THA or TKA (International Classification of Disease, 9th Revision, Clinical Modification [ICD-9-CM] procedure codes: 00.70, 81.51, 00.80, 00.84, 81.54, 81.55; Current Procedural Terminology, Fourth Edition [CPT-4] codes: 01214, 01215, 27130, 27132, 27134, 01402, 27447, 27486, 27487), and (b) at least 18 years of age as of the date of the THA or TKA. For the purpose of this study, each inpatient stay (hospitalization) for THA or TKA was considered a unit for analysis, and the study observation period spanned from the date of hospital admission to the date of discharge. For all patients, baseline characteristics were evaluated based on records collected at admission, and VTE and bleeding events were assessed based on records collected during the study observation period.
Outcome measures
The main outcomes of the study included VTE and bleeding rates and total inpatient costs, regardless of anti-coagulation therapy to estimate the real-world rates of these events. VTE events were defined as ≥1 primary or secondary diagnosis code for DVT (ICD-9-CM codes: 451.1x, 451.2, 453.4x, 453.8, 453.9) or PE (ICD-9-CM code: 415.1x). Bleeding was defined as ≥1 primary or secondary diagnosis code for any bleeding (major bleeding + non-major bleeding: see Appendix for complete list of ICD-9-CM codes). Because diagnosis codes for bleeding are less specific than those for VTE, bleeding event rates could vary depending on the definition applied. In order to control for this lack of specificity, outcomes were also studied using a more stringent definition for bleeding events limited to major bleeding (Appendix). The rates of VTE and bleeding were also stratified according to the number of risk factors (0, 1, 2, 3 or more) observed during inpatient stays.
Statistical analyses
The rate of VTE and bleeding complications among patients undergoing THA or TKA was evaluated using absolute risk. The absolute risk of VTE, any bleeding (major and non-major), and the sub-set of major bleeding events associated with THA or TKA was calculated as the number of patients with an event divided by the total number of inpatients undergoing THA or TKA. The binomial distribution was used to construct 95% confidence intervals for absolute risk. The risk stratification analysis of the rate of VTE and bleeding was conducted using descriptive statistics.
To quantify the incremental cost associated with VTE and bleeding, patients with VTE or bleeding events were matched 1:1 with control THA or TKA patients without a diagnosis of VTE or bleeding, respectively, based on both (i) exact matching factors and (ii) propensity scores using a caliper of 5%. The exact matching factors included age (5-year intervals), gender, degree of severity based on the admitting diagnosis, risk factors for VTE (trauma, major surgery, and congestive heart failure), risk factors for bleeding (anemia, major surgery, and atrial fibrillation), and use of anti-coagulant. The propensity score was generated in a first step using probability estimates from a logistic regression model that was estimated using the full database, and in which VTE or bleeding assignment was the binary dependent variable and baseline covariates were used as predictors of VTE and bleeding.
Descriptive univariate analyses were conducted to determine the incremental all-cause inpatient costs associated with VTE relative to no-VTE, bleeding relative to no-bleeding, and major bleeding relative to non-major bleeding controls. Increased inpatient costs associated with VTE or bleeding were calculated as the average total inpatient stay costs of the VTE, bleeding, and major bleeding groups minus the average total inpatient stay costs of the matched control groups.
Results
A total of 820,197 inpatient stays (269,905 THA and 550,292 TKA) met the entry criteria and formed the study populations. describes baseline patient characteristics. The VTE and bleeding group mean ages were 68.7 and 70.4 years, respectively. The proportion of women was 62.9% and 42.3% in the VTE group and the bleeding group, respectively. The mean LOS for patients with VTE and bleeding was 7.8 and 7.1 days, respectively. A total of 8042 patients developed a VTE and 7401 patients developed a bleeding event, including 2740 major bleeding complications, during hospitalization. Of the VTE events, 5434 were DVT and 3148 were PE (). Gastrointestinal bleeding was the most frequent major bleeding event (0.22%) and hematuria the most frequent non-major bleeding event (0.44%; ).
Table 1. Characteristics of patients with THA/TKA and costs per inpatient stay.
Table 2. Distribution of VTE and bleeding events.
Risk of VTE or bleeding complications
For the overall THA or TKA inpatient population, the absolute risks (95% confidence interval) of VTE, any bleeding, and the sub-set of major bleeding were 0.98 (0.96–1.00), 0.90 (0.88–0.92), and 0.33 (0.32–0.35) events per 100 inpatient stays, respectively (). The corresponding cumulative inpatient costs associated with VTE and any bleeding inpatient stays were $174,081,000 for the 8042 inpatient stays of the VTE cohort and $151,874,000 for the 7401 inpatient stays of the bleeding cohort (). The corresponding cumulative inpatient cost for the sub-set of 2740 inpatient stays with major bleeding events (i.e., out of 7401 any bleeding events) was $67,173,000.
Figure 1. (a) Incidence of venous thromboembolism and bleeding during total hip arthroplasty/total knee arthroplasty inpatient stays. (b) Total costs associated with venous thromboembolism and bleeding during total hip arthroplasty/total knee arthroplasty inpatient stays.
For the stratified analysis by VTE/bleeding risk factors, the absolute risk of VTE for a patient with 0, 1, 2, or 3+ risk factors for VTE was 0.68, 1.21, 2.01, and 4.10 events per 100 inpatient stays. The absolute risk of any bleeding for patients with 0, 1, 2, or 3+ risk factors for bleeding was 0.46, 0.64, 1.14, and 2.55 events per 100 inpatient stays, while the corresponding risk for major bleeding was 0.13, 0.19, 0.44, and 1.20 events per 100 inpatient stays ().
Table 3. Descriptive statistics on the risk stratification of VTE and bleeding events.
Inpatient costs associated with VTE and bleeding relative to control patients
From the initial sample of 8042 and 7401 patients who developed VTE and any bleeding events, respectively, 7875 (97.9%) and 7226 (97.6%) were matched with THA or TKA control inpatients without VTE or bleeding events. Characteristics of the case-control cohorts for each event are presented in and .
Table 4. Characteristics of matched VTE and control cohorts.
Table 5. Characteristics of matched bleeding and control cohorts.
After matching the VTE and bleeding cohorts with comparable control patients, both the VTE and bleeding groups were associated with increased inpatient costs compared to the no-VTE and no-bleeding control groups (). The increased LOS associated with a VTE event was 2.0 days, and with any bleeding event was 1.4 days (). For the sub-set of patients with major bleeding events, the increased LOS was 2.4 days ().
Discussion
This large retrospective study based on health claims from the PREMIER hospital database was conducted to assess the risk and all-cause cost burden of VTE and bleeding in the inpatient hospital setting after THA or TKA. A total of 820,197 THA or TKA inpatient stays were analyzed. The real-world absolute risk of VTE was slightly higher than that of any bleeding, and substantially higher than major bleeding. Although specific cost data cannot be compared directly between the VTE and bleeding cohorts (i.e., different populations with different risk factors), the overall real-world healthcare costs for VTE did represent a larger cost burden to the healthcare system than the cost burden associated with bleeding in this analysis.
After matching the VTE and bleeding cohorts with comparable control patients, the increased inpatient cost associated with a VTE event was higher compared to that of a bleeding event, but lower than a major bleeding event. However, even if major bleeding events are more costly, the risk of major bleeding (0.33%) was one-third the risk of VTE events (0.98%) following THA or TKA. Consequently, from a population perspective, the greater incremental cost associated with major bleeding compared to VTE was offset by its lower incidence. The cumulative cost burden to the healthcare system associated with VTE and bleeding events during THA or TKA inpatient stays was substantial: $174 million for VTE and $152 million for any bleeding, including $67 million for the sub-set of major bleeding events.
The purpose of the current study was to evaluate the in-hospital risk and cost of VTE and bleeding. Anti-coagulation therapy is highly effective for VTE prophylaxis following THA/TKA; however, its benefits are counterbalanced by an increased risk of bleeding. It was beyond the scope of this study to assess whether thromboprophylaxis is cost saving (and beneficial) or leads to increased costs due to bleeding, or to evaluate the impact of dosage of thromboprophylactic agents on these outcomes. Therefore, our study was conducted on all orthopedic surgery hospitalization regardless of thromboprophylaxis, and not specifically on the comparison of orthopedic hospitalization treated with thromboprophylaxis vs no thromboprophylaxis. Further research is warranted to evaluate the potential cost benefit or cost saving associated with VTE prophylaxis in orthopedic surgery hospitalization.
A risk stratification analysis of the rates of VTE and bleeding showed a rising trend for patients with VTE and bleeding risk factors. The risk of VTE for patients with 0–3 or more risk factors for VTE ranged from 0.68–4.10 events per 100 inpatient stays. Similarly, the risk for any bleeding and major bleeding for patients with 0–3 or more risk factors for bleeding rose from 0.46 to 2.55 and from 0.13 to 1.20 events per 100 inpatient stays, respectively. The comorbidity profile of THA and TKA patients is an important aspect to consider when choosing the appropriate thromboprophylaxis. For example, recent literature and guidelines discussed the possibility of mechanical thromboprophylaxis in patients at high risk for bleedingCitation2,Citation18,Citation19.
The LOS associated with any bleeding, which included major bleeding, was 1.4 days longer than that observed in a matched cohort in the absence of bleeding. The LOS associated with a VTE event was 2 days longer than the LOS compared with a comparable cohort without VTE. Assuming a standardized cost of ∼$1500 per hospital day, these results indicate potentially avoidable inpatient costs of $3000 for a VTE event and $2100 for any bleeding, which demonstrate similar costs to those found in our study. Regarding the overall population of 820,197 THA or TKA inpatient stays, at 3.9 days the mean LOS was similar to that seen in a study by Anderson et al.Citation20 at 3.7 days.
In the current study, the in-hospital risk of VTE in patients undergoing THA or TKA was 0.98%. This finding is similar to the risk of VTE obtained in a study by Samama et al.Citation17, who reported that 1.2% of THA or TKA patients had a VTE before hospital discharge, although the hospital LOS reported in Samama et al.Citation17 was longer (10.6 days), compared to what we observed in the current study (7.8 days). Memtsoudis et al.Citation21 also studied patients who underwent primary or revision THA or TKA and found that the risk of in-hospital PE was 0.36%. This compares well with the PE risk of 0.38% found in the present study. In patients undergoing THA, Hitos and FletcherCitation22 found the in-hospital incidence of VTE was 2.5%. The discrepancy in the magnitude of the reported VTE risk between the Hitos study and the current one may be due to various factors, including a different study population and study design. More recently, a systematic review of studies reporting in-hospital VTE following total or partial hip arthroplasty (TPHA) or total or partial knee arthroplasty (TPKA) among patients receiving recommended prophylaxis found that the pooled rates of symptomatic post-operative VTE before hospital discharge were 0.53% (95% CI, 0.35–0.70%) for those undergoing TPHA and 1.09% (95% CI, 0.85–1.33%) for patients undergoing TPKACitation23. Regarding bleeding, the risk of any bleeding and the sub-set of major bleeding in the current study was 0.90% and 0.33%, respectively. These results encompass the level of bleeding risk found in the study by Samama et al.Citation17, in which 0.65% of THA or TKA patients had clinically significant bleeding before hospital discharge. With respect to inpatient costs, in a study of patients who underwent THA, TKA, or hip-fracture repair, Ollendorf et al.Citation6 estimated the mean inpatient care cost for patients with PE (with or without DVT) to be $18,521 compared with $9345 for patients without PE. These estimates are consistent with the mean cost per inpatient stay of $21,014 for VTE found in the present study.
This study is subject to several limitations. First, claims databases may contain inaccuracies or omissions in procedures, diagnoses or costs. Second, the observational design was susceptible to various biases, such as information or classification bias (e.g., identification of false positive VTE or bleeding events). It is also possible that VTE and bleeding events were under-coded (i.e., false negative). However, well-designed observational studies with appropriate statistical techniques adjusting for potential confounding factors, such as the use of a matched control population, provide valuable information with real-life scenarios. Third, in addition to the site of bleeding, the severity of a bleeding event is often determined by the amount of blood that needs to be transfused. However, the database used in the present study did not contain the information pertaining to the amount of blood transfused, and the identification of major bleeding events relied solely on diagnosis codes. Fourth, costs were reflected for the specific timeframe of the study and therefore may be higher if elevated to 2012 costs due to inflation. Finally, the current study included only inpatient data, thereby limiting the observation to only short-term or acute events occurring during the THA or TKA inpatient stay. Consequently, this study did not have information on patients with prior VTE or bleeding. Of note, a large proportion of VTE events occur after hospital discharge (76% and 47% after THA and TKA, respectively)Citation24. Moreover, severe bleeding events may be associated with important morbidities beyond the hospital stay. Thus, the observation period of the current analysis may not capture the total medical costs associated with such events. Studies involving post-hospital discharge follow-up period, including rehabilitation, are therefore warranted. Despite these limitations, the current research has several advantages including the use of a large, well-known database in a robust, focused population, and a clearly defined in-hospital time frame of costs.
Conclusion
In this retrospective study of inpatients who underwent THA or TKA, the risk of VTE was greater than the risk of any bleeding, and the incremental inpatient cost associated with VTE was greater than that of any bleeding but lower when compared to the sub-set of major bleeding. From a population perspective, however, the higher incremental cost associated with major bleeding compared with VTE would be offset by the higher risk of VTE. The quantification of VTE and bleeding risk and associated cost presented here may help clinical decision-making when determining the risk and benefit of initiating anti-coagulation therapy in THA or TKA patients.
Transparency
Declaration of funding
This research was funded by Janssen Scientific Affairs, LLC, Raritan, NJ, USA.
Declaration of financial relationships
Five of the authors (Vekeman, Laliberté, Duh, Dea, and Lefebvre) are employees of Analysis Group, Inc., a consulting company that has received research grants from Janssen Scientific Affairs, LLC; and four of the authors (LaMori, Bookhart, Schein, and Olson) are employees of Janssen Scientific Affairs, LLC. Three of the authors own stock in Johnson & Johnson (Bookhart, LaMori, Olson). E. Nutescu received research grants from Janssen Scientific Affairs, LLC, Raritan, NJ, USA.
Acknowledgments
The authors would like to acknowledge Isabelle Leach, MBChB, for editorial assistance in the preparation of this manuscript with funding from Janssen Scientific Affairs, LLC.
Parts of this work were presented as posters at the National Association of Orthopaedic Nurses (NAON) 30th Annual Congress, May 15–19, 2010, Seattle, Washington, and the Academy of Managed Care Pharmacy (AMCP) 22nd Annual Meeting and Showcase, April 6–10, San Diego, CA.
References
- Heit JA, Cohen AT, Anderson FA, on behalf of the VTE Impact Assessment Group. Estimated annual number of incident and recurrent, non-fatal and fatal venous thromboembolism (VTE) events in the US. Blood (ASH Annual Meeting Abstracts) 2005;106:910
- Geerts WH, Bergqvist D, Pineo GF, et al. Prevention of venous thromboembolism: American College of Chest Physicians evidence-based clinical practice guidelines, 8th edn. Chest 2008;133:381S-453S
- Kearon C. Natural history of venous thromboembolism. Circulation 2003;107:I22-I30
- Blann AD, Lip GY. Venous thromboembolism. BMJ 2006;332:215-9
- Heit JA, O’Fallon WM, Petterson TM, et al. Relative impact of risk factors for deep vein thrombosis and pulmonary embolism: a population-based study. Arch Intern Med 2002;162:1245-8
- Ollendorf DA, Vera-Llonch M, Oster G. Cost of venous thromboembolism following major orthopedic surgery in hospitalised patients. Am J Health Syst Pharm 2003;59:1750-4
- Caprini JA, Botteman MF, Stephens JM, et al. Economic burden of long-term complications of deep vein thrombosis after total hip replacement surgery in the United States. Value Health 2003;6:59-64
- Agency for Healthcare Research and Quality. Costs for hospital discharges with a primary diagnosis of knee or hip replacement. hcupnet.ahrq.gov 2007 database. Accessed October 10, 2010
- Iorio R, Robb WJ, Healy WL, et al. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. J Bone Joint Surg Am 2008;90:1598-605
- Sullivan SD, Kahn SR, Davidson BL, et al. Measuring the outcomes and pharmacoeconomic consequences of venous thromboembolism prophylaxis in major orthopaedic surgery. Pharmacoeconomics 2003;21:477-96
- Oster G, Ollendorf DA, Vera-Llonch M, et al. Economic consequences of venous thromboembolism following major orthopedic surgery. Ann Pharmacother 2004;38:377-82
- Wolowacz SE, Hess N, Brennan VK, et al. Cost-effectiveness of venous thromboembolism prophylaxis in total hip and knee replacement surgery: the evolving application of health economic modelling over 20 years. Curr Med Res Opin 2008;24:2993-3006
- MacDougall DA, Feliu AL, Boccuzzi SJ, et al. Economic burden of deep-vein thrombosis, pulmonary embolism, and post-thrombotic syndrome. Am J Health Syst Pharm 2006;63:S5-S15
- Bullano MF, Willey V, Hauch O, et al. Longitudinal evaluation of health plan cost per venous thromboembolism or bleed event in patients with a prior venous thromboembolism event during hospitalisation. J Manag Care Pharm 2005;11:663-73
- Muntz J, Scott DA, Lloyd A, et al. Major bleeding rates after prophylaxis against venous thromboembolism: systematic review, meta-analysis, and cost implications. Int J Technol Assess Health Care 2004;20:405-14
- Shorr AF, Jackson WL, Moores LK, et al. Minimising costs for treating deep vein thrombosis: the role for fondaparinux. J Thromb Thrombolysis 2007;23:229-36
- Samama CM, Ravaud P, Parent F, et al. Epidemiology of venous thromboembolism after lower limb arthroplasty: the FOTO study. J Thromb Haemost 2007;5:2360-7
- Caprini JA. Mechanical methods for thrombosis prophylaxis. Clin Appl Thromb Hemost 2010;16:668-73
- Bahl V, Hu HM, Henke PK, et al. A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg 2010;251:344-50
- Anderson Jr FA, Hirsh J, White K, et al. Temporal trends in prevention of venous thromboembolism following primary total hip or knee arthroplasty 1996–2001: findings from the Hip and Knee Registry. Chest, 2003;124:349S–56S
- Memtsoudis SG, Besculides MC, Gaber L, et al. Risk factors for pulmonary embolism after hip and knee arthroplasty: a population-based study. Int Orthop 2009;33:1739–45
- Hitos K, Fletcher JP. Venous thromboembolism following primary total hip arthroplasty. Int Angiol 2009;28:215–21
- Januel JM, Chen G, Ruffieux C, et al. Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review. JAMA 2012;307:294–303
- White RH, Romano PS, Zhou H, et al. Incidence and time course of thromboembolic outcomes following total hip or knee arthroplasty. Arch Intern Med 1998;158:1525–31