Abstract
Objective:
Asthma is one of the most common childhood illnesses and accounts for a substantial amount of pediatric emergency department visits. Historically, acute exacerbations are treated with a beta agonist via nebulizer therapy (NEB). However, with the advent of the spacer, the medication can be delivered via a metered dose inhaler (MDI + S) with the same efficacy for mild-to-moderate asthma exacerbations. To date, no study has been done to evaluate emergency department (ED) length of stay (LOS) and opportunity cost between nebulized vs MDI + S. The objective of this study was to compare ED LOS and associated opportunity cost among children who present with a mild asthma exacerbation according to the delivery mode of albuterol: MDI + S vs NEB.
Methods:
A structured, retrospective cross-sectional study was conducted. Medical records were reviewed from children aged 1–18 years treated at an urban pediatric ED from July 2007 to June 2008 with a discharge diagnosis International Classification of Disease-9 of asthma. Length of stay was defined: time from initial triage until the time of the guardian signature on the discharge instructions. An operational definition was used to define a mild asthma exacerbation; those patients requiring only one standard weight based albuterol treatment. Emergency department throughput time points, demographic data, treatment course, and delivery method of albuterol were recorded.
Results:
Three hundred and four patients were analyzed: 94 in the MDI + S group and 209 in the NEB group. Mean age in years for the MDI + S group was 9.57 vs 5.07 for the NEB group (p < 0.001). The percentage of patients that received oral corticosteroids was 39.4% in the MDI + S group vs 61.7% in the NEB group (p < 0.001). There was no difference between groups in: race, insurance status, gender, or chest radiographs. The mean ED LOS for patients in the MDI + S group was 170 minutes compared to 205 minutes in the NEB group. On average, there was a 25.1 minute time savings per patient in ED treatment time (p < 0.001; 95% CI = 3.8–31.7). Significant predictors of outcome for treatment time were chest radiograph, steroids, and treatment mode. Opportunity cost analysis estimated a potential cost savings of $213,532 annually using MDI + S vs NEB.
Conclusion:
In mild asthma exacerbations, administering albuterol via MDI + S decreases ED treatment time when compared to administering nebulized albuterol. A metered dose inhaler with spacer utilization may enhance opportunity cost savings and decrease the left without being seen population with improved throughput.
Limitations:
The key limitations of this study include its retrospective design, the proxy non-standard definition of mild asthma exacerbation, and the opportunity cost calculation, which may over-estimate the value of ED time saved based on ED volume.
Introduction
A major question in healthcare is the underlying value of time. Specifically, the development of improved clinical efficiencies often leads to time saved per patient or per procedure. This time saved has not been accurately or consistently assigned value to evaluate the potential financial benefitCitation1. To our knowledge, there is no standardized method or approach to calculate the value of time saved in healthcare settings. Two methods for evaluating the value of time savings in a specific case study of time savings with the use of a faster asthma treatment in children were described.
Asthma is the most common chronic illness in children with a prevalence of 5–10%Citation2. It accounts for a significant amount of hospital emergency department (ED) visits and admissionsCitation2,Citation3. Standard treatment for acute asthma exacerbations include the use of β2-agonist bronchodilators, such as albuterol, delivered by a metered dose inhaler with spacer (MDI + S) or nebulization (NEB). In the past, children less than 5 years of age were frequently treated with nebulized albuterol because their level of co-ordination precluded MDI use. However, with the advent of spacer and facemask devices, children ≥12 months are now able to receive adequate amounts of a bronchodilator through MDI + SCitation4. Despite this development, MDI + S use lags far behind NEBs in the treatment of acute asthma exacerbations in the pediatric ED settingCitation2,Citation4.
Compared to nebulized albuterol, MDI + S has several advantages. These advantages include: less tachycardia and side-effectsCitation2,Citation5,Citation6, decreased costCitation7–9, better portability, ease of use, and the absence of a required electrical power source at home. In addition, previous studies found MDI + S to be equally effective as NEB in medication deliveryCitation2–4,Citation6,Citation7,Citation10,Citation11 and associated with a lower likelihood of admission to the hospitalCitation2,Citation12.
With regards to hospital cost, one study found that the potential hospital cost savings was ∼$83,000 annually by switching to MDI + S from NEB for the delivery of β2-agonist bronchodilators. In addition, charges to patients were lowered by ∼$300,000 per yearCitation9. In this study, the authors focused on cost savings in terms of patient charges and hospital costs from respiratory care charge data, rather than cost savings solely in terms of time saved.
A more recent study, using the Cochrane database, found that substituting MDI + S for NEBs for children with mild-to-moderate asthma exacerbations would, in most cases, result in both cost savings and a reduction in hospitalizations. This Canadian study, however, was conducted in a single payer healthcare model, which may not be generalizable to the US healthcare settingsCitation13. It was hypothesized that, for mild asthma exacerbations, pediatric patients treated with albuterol MDI + S have shorter ED treatment time and ED length of stay (LOS) than patients treated with nebulized albuterol. The specific aim was to assign values to ED treatment time by two models: an opportunity cost model and a model that assesses ED treatment time and estimates decreasing the ‘left without being seen’ (LWBS) rate.
Methods
After Institutional Review Board approval, all charts from Kosair Children’s Hospital ED from July 1st 2007 to June 30th 2008 of children aged 1–18 years with acute mild asthma exacerbation who received albuterol were evaluated for study eligibility. Charts were initially identified using ICD-9 codes (493.0, 493.1, 493.2, 493.8, 493.9, and 786.0) for the following: wheezing, cough-variant asthma, asthma exacerbation, and asthma. A functional definition of mild exacerbation to include patients who required only one standard albuterol nebulization or one albuterol metered dose inhaler treatment during the ED visit was utilized.
Through the ED’s electronic patient tracking system, the lower acuity levels (3, 4, and 5) were included in the review. Medical records were then evaluated individually to determine whether or not they met inclusion criteria.
Patients were excluded if they were admitted to the hospital, seen in urgent care, received more than one standard treatment dose of albuterol, those who required admission, or returned to the ED within 72 hours for asthma complaints. Data review and abstraction was performed by a single reviewer, the principal investigator (LS), using a data abstraction form before transcription into an electronic database.
Demographic data included age, sex, ethnicity, and type of insurance. Historical data included symptoms leading up to their current illness, previous history of wheezing, home medications, and interventions completed at home prior to arrival to the ED.
Clinical measurements recorded included temperature, pulse rate, respiratory rate, and oxygen saturation. The following treatment interventions were recorded: method of albuterol delivery, corticosteroid administration, and chest radiograph (CXR). Time measurements included in the study were: (1) patient arrival time; (2) time the patient signed into the ED; (3) time at which the physician first saw the patient and ordered the albuterol; (4) times of albuterol initiation and completion as documented by either the nurse or RT on the respiratory order sheet; (5) the time the physician wrote the discharge order; and (6) time the caregiver signed the discharge instructions.
The two main clinical outcomes evaluated were ED LOS and ED treatment time. The ED LOS was defined as the time the patient was initially triaged to the time the guardian signed the discharge instructions. Emergency department treatment time was defined as the time elapsed from when the patient was initially seen by the physician/nurse practitioner to the time the discharge order was written. The Mann-Whitney U-test was used to compare ED treatment time and ED LOS for the MDI + S group vs the NEB group. Mann-Whitney U was also used to evaluate the various predictors for inclusion in the multiple linear regression analysis. Logistic regression was used to compare ED treatment times between MDI + S and NEB. The ratio of the times was used to calculate the difference between MDI + S and NEB. The unpaired student’s t-test was used to compare the demographic data between the two groups as appropriate.
Methods of cost analysis
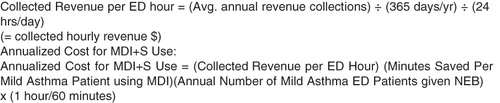
Annual collections for 2007–2008 were calculated from financial hospital data. Utilizing patient census and collections, a collected revenue per ED hour was calculated. This hourly collected revenue data was combined with time savings to estimate an annual ED opportunity cost (). The term ‘opportunity cost’ is used to describe the revenues foregone as a result of the less efficient nebulizer mode of albuterol delivery.
The authors used a second calculation to estimate potential increased revenue was used and based on decreased left without being seen rates (LWBS) because it may more accurately reflect improved ED efficiency. Although the opportunity cost calculation may be more easily determined due to fewer variables, it may over-estimate the value of time saved.
Using 2007–2008 data and electronic patient tracking data, a sensitivity analysis of potential increased revenue from decreased LWBS was performed. These sensitivity analyses utilized billing and acuity data from 2007–2008 and modeled decreased LWBS by 25%, 50%, and 75%.
Results
Demographics
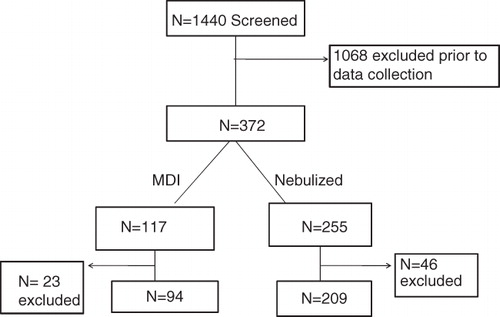
Initially, 1440 patients were found to be eligible for review based on the ICD-9 code and acuity. Of those, 1068 were excluded prior to data collection due to failure to meet initial inclusion criteria. The most common reason for exclusion was treatment in the urgent care setting. Of the remaining 372 patients, 255 were given nebulized albuterol and 117 were given albuterol via MDI. After chart review, 46 of the nebulized patients and 23 of the MDI patients were excluded due to criteria defined in the study methods. The final analyzed study population had 303 patients: 209 in the nebulized group and 94 in the MDI group ().
The mean age for the nebulized group was 5.1 years compared to 9.6 years for the MDI group. When the authors evaluated other demographic data, such as gender, insurance status, and ethnicity, there were no significant differences between the two groups.
In analyzing the adjuvant treatment administered in the ED, there was no difference between the groups in the proportion who underwent CXR. There was a difference among those given oral corticosteroids, however, with 60% of the patients in the NEB group receiving oral steroids vs 42% in the MDI + S group (p < 0.001) ().
Table 1. Demographic data*.
Study outcomes for model 1: Opportunity cost basis
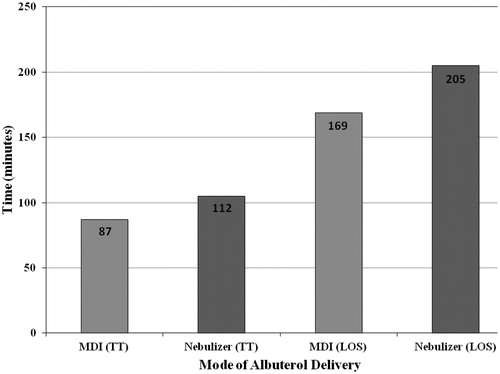
Utilizing the Mann-Whitney U, predictors associated with ED treatment time were mode of treatment, oral corticosteroids, and CXR. Specifically, nebulized albuterol, administering oral corticosteroids, and CXR all predicted a longer ED treatment time. The predictors associated with a longer total ED LOS were mode of treatment, systemic corticosteroids, CXR, and age ().
Table 2. Linear regression analysis of log ED treatment time*.
Table 3. Multiple regression analysis: Log ED treatment time.
Table 4. Multiple regression analysis: Log ED length of stay.
Table 5. Potential increased collected revenue when substituting MDI + S for nebulizer.
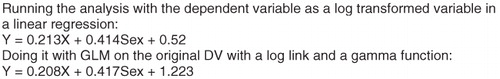
The mean ED treatment time for the MDI + S group was 87 minutes. With a regression model predicting the logarithm of treatment time, the ratio of times predicted between the two modes will be constant for any combination of other predictors. In this analysis that ratio was 1.288. The authors set up a simple SPSS file with two predictors and a dependent variable and ran the analysis using both the dependent variable as a log transformed variable in a linear regression and as a GLM analysis on the original dependent variables with a log link and gamma function. The same result using both methods was found ().
Thus, our estimate of the most typical ED treatment time for the NEB group was calculated to be 112 minutes (). There was, therefore, a predicted time saving of 25.1 minutes for the MDI + S group compared to the NEB group in ED treatment time (). The mean ED LOS for the nebulized group, defined as the time from initial triage to the time the caregiver signed the discharge instructions, was 205 minutes compared to 169 minutes for the MDI + S group. That results in a mean time savings for the MDI + S group of 36 minutes ().
Based on revenue data for 2007–2008, our total ED charges were $1783.31/hour; the hospital collected $517 per hour, which was 29% of the average hourly ED charge. The potential increased revenue for substituting MDI + S for nebulizers based on ED treatment time was calculated (). According to the data, both prior to and after exclusion, ∼68.6% of study patients received nebulized albuterol vs albuterol via MDI + S. The authors used this percentage to determine the total number of patients that would have been given a NEB rather than a MDI + S. For study inclusion, 1440 patients were screened, thus 987 would have theoretically been treated with NEB. With a 25.1 minute time savings substituting MDI + S for NEB, the calculated opportunity cost is $213,532 (). This value reflects the maximal incremental collected revenue for utilizing MDI + S instead of NEB. A more accurate, conservative value may be 25% of this maximal value, $53,383. This value is based on the assumptions that a baseline use of MDI exists in most EDs and that barriers to MDI adoption may continue, as well as a linear relationship exists between LWBS and increased revenue. We also calculated 50% and 75% of the total maximal incremental collected revenue for ED treatment time and found them to be $106,766 and $160,149, respectively.
Study outcomes for model II: Left without being seen basis
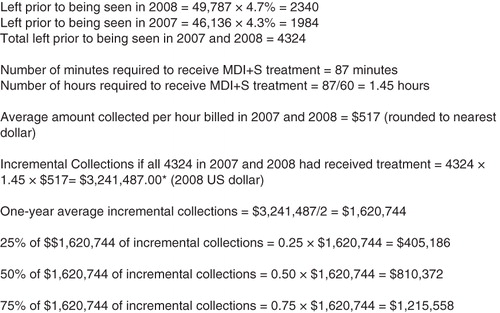
During 2008 at Kosair’s Children’s Hospital, 49,787 patients visited the ED for an evaluation. Of those, 4.7% (2340) left prior to being seen by a physician, up from 4.3% in 2007. This appears to be due, in part, to the increasing ED volume, as only 46,136 patient visits occurred in 2007. Previous research performed in our facility on patient data from 2007–2008 showed that decreasing our wait times to less than 2 hours can decrease our LWBS rate from 8.3% to 2.4%Citation14. Based on our calculations shown in , decreasing our LWBS rate by 25% would increase collections for the 2-year period by $810,622. When the LWBS rate is decreased by 50% potential collections would increase by $1,621,244. A 75% reduction in LWBS would increase collections for the 2-year period by $2,431,867. Of note, these increased collections are predicated on the reduction of the wait time and the availability of respiratory therapists and nurses.
Discussion
Our retrospective cohort study examined the time difference of MDI + S vs NEB therapy in a pediatric ED setting. Among a cohort of pediatric asthma patients with mild exacerbations, treatment with MDI + S was associated with a reduction in both ED treatment time and ED LOS. It was demonstrated that when a nebulizer is substituted with MDI + S for albuterol delivery the time saved can translate to increased revenue. The major advantage of our opportunity cost approach is that it is a relatively simple value to calculate and easy to apply for return on investment calculations for future interventions to impact ED care.
It is possible to draw some important conclusions from our financial models. The opportunity cost model shows that if 25.1 minutes could have been saved for each NEB performed during the 1-year period (July 1, 2007 through June 30, 2008), $213,532 of additional revenue could have been collected. These collections assume that there were ED patients waiting and available to use up all of that newly-available capacity. Our LWBS model () indicates that decreasing the LWBS rate by 25% could lead to a $405,311 increase in collected revenue. When the LWBS rate is decreased by 50% the potential incremental collected revenue increases to $810,622 and there is a collected revenue gain of $1,215,933 for a 75% reduction in LWBS.
The benefit of MDI + S may extend beyond financial considerations. Less time spent per patient allows the ED system of nurses, physicians, and ancillary staff to spend more time with other patients. These benefits are more difficult to evaluate but are clearly important, as patient satisfaction increases with increased physician contact and faster ED throughputCitation15. Substituting MDI + S for NEB has the potential of increasing collections by reducing the patient wait time and thereby decreasing the number of potential patients who leave without being treated. Additionally, MDI + S has the potential of increasing capacity to permit the treatment of additional patientsCitation13. The dollar value of that increased capacity can be estimated in terms of our collections calculation.
Interestingly, the mean difference in ED LOS for our study (36 minutes) was nearly identical to those reported by previous investigatorsCitation8. Factors associated with a longer treatment time and LOS in the ED, in addition to treatment mode, were corticosteroids and CXRs. These factors make intuitive sense, because obtaining CXRs and administering oral medications require more time. Additionally, those who received a CXR or corticosteroids may have been experiencing a more significant asthma exacerbation or there may be concerns for an alternate diagnosis, thus leading the treating physician to monitor them for a longer period of time compared to those who did not receive those interventions.
Age predicted a longer ED LOS, but not a longer treatment time. Whether this was incidental or truly represented a difference among this population of patients is difficult to establish retrospectively. It may be that the younger patients tended to be seen and treated in the ED during peak hours and are less likely to be sent to our urgent care setting, thus resulting in a longer ED LOS. Additionally, older patients may have been triaged at a lower acuity level and waited longer to be seen, but then were found to need an albuterol treatment. Patients may have appeared ill to the physicians, thus resulting in longer treatment time and LOS. The acuity assigned to these patients was not found to be a predictor of either treatment time or LOS. Our methods excluded the higher acuity patients (1 and 2) due to our operational definition of a mild exacerbation of asthma and selected for similar acuity in our study population.
At Kosair Children’s Hospital ED, we evaluated, in a 12-month period, 1440 mild asthma patients. Instituting a clinically-effective ED intervention of albuterol via MDI + S for all mild asthmatics greater than 1-year old can potentially decrease ED throughput time, allow more patients to be seen and treated, decrease the respiratory therapists time with each patient, and likely improve LWBS rate. Substituting MDI + S for current NEB treatments may lead to a substantial overall increase in collected revenue for the ED.
Limitations
There were several limitations with our study. First, this retrospective study utilized ICD-9 codes, and our electronic tracking system to capture the patients. Our proxy definition of a mild asthma exacerbation excluded patients based in part on their response to the therapy. This definition was non-standard and could bias the results. Also, we relied on the input of accurate data, specifically time data, from the written medical record. The times written on the charts may not have been accurate. Additionally, patients were excluded based in part on their response to therapy which was not standardized and could have biased our results.
One limitation of our opportunity cost calculation is that it may over-estimate value of ED time saved because it assumes that there are patients waiting to be seen by healthcare providers and maximal ED capacity occurs 100% of the time, with RT and nursing staff capacity at 100%. In a 12-month period, our emergency department had a wait time greater than 2 hours, on average 30% of the time from the months of September through May, with a peak in February and MarchCitation14. An advantage of using an asthma model is that asthma exacerbations peak during the late winter respiratory season. This season coincides with high ED census across North America.
The opportunity cost calculation is a maximal value. Our tiered sensitivity analysis may more accurately evaluate this cost. Our conservative approach using 25% of this maximal value may offset the over-estimation. Also, modeling by quartiles may provide a familiar context for physicians who use quartiles to determine interventionsCitation15,Citation16. A future prospective study may be able to evaluate non-financial benefits such as patient satisfaction in a pre- and post-implementation design as well as accurate LWBS rates and ED respiratory therapist and nursing utilization.
Finally, this study is from the hospital perspective, the benefits of opportunity cost would be only to the hospital and to the patient for more time spent outside of the ED.
Conclusion
Substituting MDI + S for NEB albuterol delivery in mild asthma exacerbations in a pediatric ED can decrease both ED treatment time and ED LOS. This time saved can then be translated into financial revenue gained using either an opportunity cost analysis model or a LWBS-based estimate. Our models can be used to compare other equally-effective but different treatment ED regimens when analyzing time savings and opportunity cost. In addition, our second LWBS model can estimate increased collected revenue based on improved ED efficiencies in patient throughput.
Transparency
Declaration of funding
Funding for this study came from a grant for the University of Louisville, Department of Pediatrics’ Fellows.
Declaration of financial/other relationships
The authors have disclosed that they have no relevant financial relationships to be declared.
Acknowledgments
The authors would like to acknowledge and thank Kendra Sikes, a research co-ordinator who has helped out at all stages of this research project. The authors would also like to thank Ellerbe Powell, the former IT supervisor for the ED, who helped pull all of the eligible charts from our electronic medical record system.
References
- Lama T, Small K. Transportation Research Part E. Logist Transport Rev 2001;2–3:231-51
- Benito-Fernandez J, Gonzalez-Balenciaga M, Capape-Zache S, et al. Salbutamol via metered-dose inhaler with spacer versus nebulization for acute treatment of pediatric asthma in the emergency department. Pediatr Emerg Care 2004;20:656-9
- Delgado A, Chou KJ, Silver EJ, et al. Nebulizers vs. metered-dose inhalers with spacers for bronchodilator therapy to treat wheezing in children aged 2 to 24 months in a pediatrics emergency department. Arch Pediatr Adolesc Med 2003;157:76-80
- Ploin D, Chapuis FR, Stamm D, et al. High-dose albuterol by metered-dose inhaler plus a spacer device versus nebulization in preschool children with recurrent wheezing: a double-blind, randomized equivalence trial. Pediatrics 2000;106:311-7
- Chou KJ, Cunningham SJ, Crain EF. Metered-dose inhaler with spacers vs nebulizers for pediatric asthma. Arch Pediatri Adolesc Med 1995;149:201-5
- Schuh S, Johnson DW, Stephens D, et al. Comparison of albuterol delivered by a metered-dose inhaler with spacer versus a nebulizer in children with mild acute asthma. J Pediatr 1999;135:22-7
- Hendlers L, Hatton RC, Coons TJ, et al. Automatic replacement of albuterol nebulizer therapy by metered-dose inhaler and valved holding chamber. Am J Health-Syst Pharm 2005;62:1053-60
- Amirav I, Newhouse MT. Metered-dose inhaler accessory devices in acute asthma—efficacy and comparison with nebulizers: a literature review. Arch Pediatr Adolesc Med 1997;151:876-82
- Bowton DL, Goldsmith WM, Haponik EF. Substitution of metered-dose inhalers hand-held nebulizers. Success and cost savings in a large, acute-care hospital. Chest 1992;101:305-8
- Rodrigo C, Rodrigo G. Salbutamol treatment of acute severe asthma in the ED: MDI versus hand-held nebulizer. Am J Emerg Med 1998;16:637-42
- Mandelberg A, Chen E, Noviski N, et al. Nebulized wet aerosol treatment in Emergency Department—is it essential? Comparison with large spacer device for metered-dose inhaler. Chest 1997;112:1501-5
- Rubilar L, Castro-Rodriguez JA, Girardi G. Randomized trial of salbutamol via metered-dose inhaler with spacer versus nebulizer for acute wheezing in children less than 2 years of age. Pediatr Pulmonol 2000;29:264-9
- Doan Q, Shefrin A, Johnson D. Cost-effectiveness of metered-dose inhalers for asthma exacerbations in the pediatric emergency department. Pediatrics 2011;127:e1105-11
- Cross K, et al. Identifying key metrics for reducing premature departure from the pediatric emergency department. Working Paper. Louiseville, KY: University of Louisville, 2010
- Maio RF, Herbert GG, Spaite, et al. Emergency Medical Services Outcomes Project I (EMSOP I): prioritizing conditions for outcomes research. Presented in part at the Society for Academic Emergency Medicine Annual Meeting, Washington DC, May 1997, and the National Association of EMS Physicians, Mid-Year Meeting, Lake Tahoe, NV, July 1997
- Hung GR, Chalut D. A consensus-established set of important indicators of pediatric emergency department performance. Pediatr Emerg Care 2008;24:9-15