Abstract
Objective:
Literature on the economic burden of anal cancer in Germany is scarce. About 84% of these cancers are associated with human papillomavirus infection. This study, therefore, aimed to assess the annual costs of human papillomavirus-related anal cancer incurred by hospitalization, inpatient rehabilitation, and sick leave in 2008 in Germany.
Methods:
A cross-sectional retrospective analysis of five German databases covering hospital treatment, inpatient rehabilitation, and sick leave in 2008 was performed. All hospital, inpatient rehabilitation, and sick leave cases due to anal cancer in 2008 were analyzed. Associated numbers of anal cancer hospitalizations, healthcare resource use, and costs were identified and extracted using the ICD-10 code C21 as the main diagnosis. The annual cost of human papillomavirus-related anal cancer was estimated based on the percentage of anal cancer likely to be attributable to human papillomavirus.
Results:
In 2008, there were 5774 hospitalizations (39% males, 61% females), 517 inpatient rehabilitations, and 897 sick leaves due to anal cancer representing costs of €34.11 million. The estimated annual costs associated with human papillomavirus-related anal cancer were €28.72 million, mainly attributed to females (62%). Direct costs accounted for 90% (86% for hospital treatment, 4% for inpatient rehabilitation) and indirect costs due to sick leave accounted for 10% of human papillomavirus-related costs.
Conclusions:
The economic burden of human papillomavirus-related anal cancer in 2008 in Germany is under-estimated, since costs incurred by outpatient management, outpatient chemotherapy, long-term care, premature retirement, and premature death were not included. However, this study is the first analysis to investigate the economic burden of anal cancer in Germany. The estimated annual costs of human papillomavirus-related anal cancer contribute to a significant economic burden in Germany and should be considered when assessing health and economic benefits of human papillomavirus vaccination in both genders.
Introduction
Anal cancers comprise squamous cell carcinomas of the anal canal and the anal verge, whereas adenocarcinomas in this region are classed as rectal cancerCitation1. The precursor lesion of anal cancer is anal intraepithelial neoplasia (AIN), which is graded from 1 (low-grade) to 3 (carcinoma in situ)Citation2. Although the prevalence of AIN in the general population is unknown, AIN has been detected with increasing frequency, and long-term studies have shown that ∼5% of high-grade AIN lesions progress to invasive cancerCitation2.
Seven regional German cancer registries have reported age-standardized (world) incidence rates of anal cancer of 0.4–1.0 per 100,000 males and 0.6–1.4 per 100,000 females in different parts of the countryCitation3. However, to our knowledge, there are no official data on the incidence and prevalence of anal cancer in the German population as a whole. In general, the incidence of anal cancer increases with age and is more common in females than in malesCitation4,Citation5.
HPV infection has been detected in 84.2% of anal cancersCitation6. Most HPV-related anal cancers are associated with the high-risk HPV types 16 and 18Citation6,Citation7. Several other risk factors for anal cancer have been reported, such as smoking, immunosuppression, receptive anal intercourse, higher lifetime number of sexual partners, and human immunodeficiency virus (HIV) infectionCitation7. However, clinical awareness of AIN is less developed than for cervical intraepithelial neoplasia (CIN), the equivalent precursor lesions of cervical cancer, and, as no organized screening for AIN exists, diagnosis is often delayed due to a lack of clinical symptoms8.
There are a number of studies assessing the disease burden and cost of HPV-related anal cancer in other countriesCitation8–10; however, this is poorly documented in Germany as no studies from the German setting exist. Therefore, the objective of the present study was to estimate the economic burden due to hospitalization, inpatient rehabilitation, and sick leave of HPV-related anal cancer in 2008 in Germany. These data will also be useful in terms of assessing whether an HPV vaccination strategy would be cost-effective, considering the potential vaccine’s impact on the burden of HPV-associated anal cancer in Germany.
Methods
The annual cost of anal cancer was estimated by considering the expenditure of social insurance bodies as proxies for direct medical costs incurred by hospital treatment and inpatient rehabilitation. Indirect costs due to sick leave were estimated using a human capital approach. Outpatient management, patients’ co-payments and out-of-pocket expenses were not considered. Further information on which component is included or not in the study is presented in .
Table 1. Cost components of the analysis.
The study was based on a retrospective cross-sectional analysis of five German databases that cover hospitalizationsCitation11, distribution of diagnosis-related groups (DRG) and major categories of treatment during hospital stayCitation12, inpatient rehabilitationCitation13, and sick leaveCitation14,Citation15, each with the reference year 2008. Associated numbers of anal cancer hospitalizations, healthcare resource use, and unit costs were identified and extracted using the International Classification of Diseases, 10th revision code for malignant tumor of the anus and anal canal (ICD-10 code C21) as the main diagnosis. The same diagnostic code (C21) could be used for extraction as it is documented in each of the above-mentioned databasesCitation11–14 used. Thus, the extracted numbers of cases refer to resource consumption units and not to patients, due to the nature of the databasesCitation11–14 used. Annual costs of HPV-related anal cancer were estimated by using the proportion of 84.2% attributable to HPV infectionCitation6.
Estimation of direct costs incurred by hospitalization
The annual cost incurred by hospital treatment (medical attendance, care, drugs, devices, physical therapy, board and lodging) of anal cancer (C21 coded as the main diagnosis) was based on the number of hospitalizations and the average cost per hospital stay. The number of hospital stays with the main diagnosis of anal cancer (C21) was extracted from the hospital statistics published by the Federal Statistical Office Germany (Destatis)Citation11. These statistics are by law exhaustive for all GermanyCitation11 and provide information on the number of hospitalizations by ICD-10 code, age group, and genderCitation11.
The average hospital treatment cost per C21 hospital stay was derived from the type and number of German diagnosis-related group (G-DRG) positions reimbursed for the main diagnosis of C21. G-DRG data are by law exhaustive for all GermanyCitation12. These are published by the Institute for the Hospital Remuneration System (InEK) as G-DRG BrowserCitation12, which provides information on type and frequency of reimbursed G-DRGs per ICD-10 main diagnosis as well as type and frequency of major treatment categories such as surgery, radiotherapy, and medical treatment per reimbursed G-DRG position.
Costs for each extracted G-DRG position related to C21 were calculated by multiplying the cost weight of each extracted G-DRG positionCitation12 with the Germany-wide average base rate of €2803.05 in 2008Citation1Citation6,Citation17.
For all G-DRG positions, the G-DRG Browser only lists the top-20 main diagnoses. If a case has a main diagnosis that is among the top-20 of a certain DRG, this case shows up in the Browser data. If a rare main diagnosis uses a G-DRG that is used by many other more frequent main diagnoses, it will not show up in the Browser. Therefore, the extrapolation of costs from the number of cases in the G-DRG Browser to the number of cases from the hospital statistics was supplemented by collection of aggregate anonymized data on the distribution of G-DRG positions for treatment of C21 in one hospital to identify potential important missing G-DRGs.
Hospital treatment costs extrapolated from the G-DRG BrowserCitation12 data were stratified by gender assuming the same distribution for costs as for the number of hospitalizations extracted from the hospital statisticsCitation11.
Estimation of direct costs incurred by inpatient rehabilitation
For patients with anal cancer, inpatient rehabilitation following acute hospital cancer treatment comprises training to cope with rectal incontinence, nutritional counseling, treatment of radiation damage, etc., and is intended to enable employed patients’ further labor force participation. In Germany, inpatient rehabilitation is paid by the Public Pension InsuranceCitation13, whereas acute hospital treatment is paid by sick funds. The annual cost incurred by inpatient rehabilitation due to the main diagnosis of anal cancer (C21) after acute hospital cancer treatment was based on the number and average duration of rehabilitation stays (in days) and the average cost per day.
The number of rehabilitation stays with the main diagnosis of anal cancer (C21) was extracted from rehabilitation statistics published by the holder of the German Public Pension Insurance (DRV)Citation13. These statistics are by law exhaustive for all GermanyCitation13 and provide information on the number of inpatient rehabilitation stays and duration in days by ICD-10 3-digit main diagnosis code and genderCitation13. Outpatient rehabilitation is not included in the present study, as the related data are aggregated over disease groupsCitation13, thus preventing ICD-10 3-digit codes from being extracted.
The average cost per day of inpatient rehabilitation was also derived from rehabilitation statisticsCitation13. Total costs of €2689.84 millionCitation13 divided by a total of 24,120,180 days (804,006 stays with a mean of 30 days per stay)Citation13 resulted in an average cost of €111.52 per day for inpatient rehabilitation. The average cost per day is not disease-specific.
The number, duration (in days), and cost of inpatient rehabilitation stays were stratified by gender.
Estimation of indirect costs incurred by sick leave
The annual cost incurred by sick leave due to the main diagnosis anal cancer (C21) was based on the number of sick leaves, the average duration per case in days and cost per day.
The number and duration of sick leaves were estimated in two steps. In the first step, the number of sick leave cases and average duration per sick leave case in days due to the main diagnosis of anal cancer (C21), each by gender, were extracted from statistics covering the population of all compulsory members (i.e., insured without co-insured dependants and pensioners) of the Local Statutory Health Insurance (SHI) fund (AOK), which is the biggest SHI fund in Germany. These statistics are available via the Information System of Federal Health Monitoring (GBE)Citation14. As these data are not exhaustive for all Germany, a second step was applied to extrapolate the numbers and duration of sick leave cases extracted from the AOK statisticsCitation14 to the total German compulsory SHI member population based on statistics for the total German SHI population published by the Federal Ministry of Health (BMG), the KM6 statisticsCitation15. This was done based on the gender-specific share compulsory AOK members took in the total compulsory SHI member population in 2008 available from the KM6 statisticsCitation15.
Using the human capital approachCitation18, overall employee compensation per employee per day was used as cost per day of sick leave. The overall employee compensation per employee per day in 2008 was derived from the Statistical YearbookCitation19. An overall employee compensation of €1225.84 billionCitation19 divided by 35,845,000 employeesCitation19 and 365 days resulted in a cost of €93.69 per employee per day.
The number, duration (in days), and costs incurred by sick leave were stratified by gender.
Estimation of annual cost of anal cancer and of HPV-related anal cancer
The annual cost of anal cancer was estimated by adding costs incurred by hospitalization, inpatient rehabilitation, and sick leave. These annual costs were stratified by direct and indirect costs as well as by gender.
A separate calculation was made to estimate the annual cost of HPV-related anal cancer, based upon the proportion of 84.2% of anal cancers attributable to HPV infectionCitation6.
Statistical methods
Due to the nature of the databasesCitation11–14 used, which exclusively provide average values of all the cases comprised, no measure of variability could be quoted for the estimated cost figures. This, however, is deemed acceptable as the hospital and rehabilitation statisticsCitation11,Citation13 are by law exhaustive for all GermanyCitation11,Citation13. In addition, the G-DRG-related base rateCitation16,Citation17 to estimate costs incurred by hospitalization and the cost per day of inpatient rehabilitationCitation13 to estimate costs incurred by inpatient rehabilitation each are Germany-wide averagesCitation13,Citation16,Citation17. Hence, the use of Germany-wide averages and the fact that the data are exhaustive allowed us to refrain from sensitivity analysis as no variability is expected. All analyses were performed using Microsoft® Excel 2007 (Microsoft Corp., Redmond, WA).
Results
Direct costs incurred by hospitalization
Number of hospitalizations
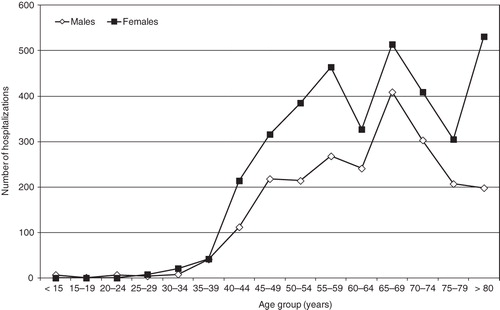
In 2008, there were 5774 hospitalizations for anal cancer (C21) in Germany: 2238 for males (39%) and 3536 for females (61%). The number of anal cancer hospital stays increased starting from age 35–39 years and reached a plateau at ∼55–59 years. Sixty per cent of the hospitalizations were for patients older than 60 years; 50% were for patients older than 65 years. In males, the peak hospitalization age range was 65–69 years; for females, there were three distinct peaks in hospitalization age groups (55–59 years, 65–69 years, and >80 years). The distribution of the number of hospitalizations by age group and gender is given in .
Major categories of treatment
The distribution of major treatment categories during hospitalization was derived from the G-DRG codes extracted from the G-DRG BrowserCitation12 (). Most of the hospitalizations due to anal cancer (C21) were linked to radiotherapy exclusively (85%), followed by surgery alone (13%). Combination treatment of surgery and radiotherapy accounted for 1% of the hospitalizations, as did medical treatment (e.g., exploration, chemotherapy) alone. All important G-DRGs for anal cancer treatment seem to be accounted for in the G-DRG Browser as the hospital data showed.
Table 2. G-DRGs reimbursed for hospital treatment of anal cancer in 2008 in GermanyCitation12.
Costs
The extracted G-DRGs used to estimate the average cost per hospital case with anal cancer (C21) are listed in : 2018 casesCitation12 compared to the total of 5774 cases documented in the hospital statisticsCitation11. The average cost per hospitalization amounted to €5109 and was applied to the total of 5774 hospitalizations, as the collected hospital data showed that no important G-DRG was missed. Total cost of hospitalization was €29.50 million, with €11.43 million for males (39%) and €18.07 million for females (61%) (). The main contributors to these costs were radiotherapy (69%) and surgery (28%).
Table 3. Annual cost (€) of anal cancer incurred by hospitalization, inpatient rehabilitation, and sick leave in 2008 in Germany (inconsistencies are due to rounding).
Direct costs incurred by inpatient rehabilitation
In 2008, there were 517 inpatient rehabilitation stays for the main diagnosis of anal cancer (C21) in Germany: 173 for males (33%) and 344 for females (67%). The average duration of stay of 23 days for both genders resulted in a total of 11,891 days of inpatient rehabilitation. Based on an average cost per day of €111.52, the costs incurred by inpatient rehabilitation were estimated at €1.33 million ().
Indirect costs incurred by sick leave
In 2008, compulsory AOK members comprised 5,409,955 males and 4,067,300 femalesCitation15. There were 150 sick leave cases due to anal cancer for males, corresponding to a total of 4327 sick leave days (≈28.85 days per case); there were 135 sick leave cases due to anal cancer for females, corresponding to a total of 6517 sick leave days (≈48.27 days per case)Citation14. In 2008, the total German compulsory SHI member population comprised 15,374,034 males and 14,174,791 femalesCitation15. Hence, the factors were 15,374,034/5,409,955 = 2.8414 for males and 14,174,791/4,067,300 = 3.4851 for females to extrapolate cases and days of sick leave from compulsory AOK members to the German compulsory member population.
There were a total of 897 cases (47% for males, 53% for females) and 35,008 days (35% for males, 65% for females) of sick leave due to the main diagnosis of anal cancer (C21) in 2008 in Germany. At a cost of €93.69 per workday lost, indirect costs incurred by sick leave are estimated at €3.28 million, with €1.15 million attributed to males (35%) and €2.13 million to females (65%) ().
Annual cost incurred by hospitalization, inpatient rehabilitation, and sick leave
In 2008, the annual cost of anal cancer (C21) amounted to €34.11 million. Of these costs, 90% were direct costs (86% hospitalization, 4% inpatient rehabilitation) and 10% were indirect costs incurred by sick leave ().
Based on the prevalence of HPV in anal cancer of 84.2%Citation6, the annual cost attributable to HPV infection was estimated at €28.72 million (38% males compared to 62% females).
Discussion
This study estimated that the annual cost due to hospitalization, inpatient rehabilitation, and sick leave incurred by HPV-related anal cancers in Germany was €28.72 million in 2008 (38% males), with 90% direct costs (86% hospitalization, 4% inpatient rehabilitation) and 10% indirect costs due to sick leave.
Several factors contribute to the strength of the present study. Most importantly, the data sources used for the number of cancer-specific hospitalizationsCitation11 and inpatient rehabilitationsCitation13 were exhaustive for all Germany. These databases were also used in previous cost-of-illness (CoI) analysesCitation20–22.
Limitations of the present study are mainly linked to the cost components covered compared to the components of overall CoI. The present study covered only three out of 10 components of overall CoI (); it excluded outpatient management, patients’ co-payments and out-of-pocket expenses which are expected to be important contributors to the total economic burden of anal cancer management. In addition to the restrictions mentioned above, costs incurred by complications, side effects, or sequelae of the treatment of anal cancers, such as the need for adult diapers, were not included. It is reported that ∼US$400 million are spent on adult diapers in the US per yearCitation8. Given the factors outlined above, it is clear that this study under-estimated the total annual cost of anal cancer and of HPV-related anal cancer in 2008 in Germany to a considerable extent. However, in order to avoid speculative assumptions and to keep a conservative approach, no attempts were made to roughly estimate the potential contribution of all the costs not included.
The present study used a cross-sectional approach to estimate these annual costs. The data used to estimate the number of hospitalizationsCitation11, inpatient rehabilitationsCitation13, and sick leavesCitation14 are from patients with at least one such resource consumption in the reference year. Hence, as the numbers refer to resource use or consumption units and not to single patients in that yearCitation11–14, no patient level information is available with respect to co-morbidities or numbers of hospitalizations, inpatient rehabilitations or sick leaves, each per patient per year. Indeed, in the G-DRG BrowserCitation12 data co-morbidity information is exclusively given per reimbursed G-DRG position. As a given G-DRG position applies to inpatient treatment of cases with different underlying main diagnoses, no co-morbidity pattern specific to anal cancer cases (main diagnosis ICD-10 code C21) can be identified and extracted. Additionally, for hospital treatment, no incident cases with high resource consumption can be distinguished from prevalent cases with less resource consumption due to the nature of the databasesCitation11,Citation12 available. Thus, the estimated average cost of hospitalization reflects the average cost for all anal cancer cases treated in hospital and is consequently lower than the average cost per patient or per new cases, as patients may be hospitalized several times per year.
In 2008 in Germany, there were 1158 incident cases of anal cancer (403 males and 755 females)Citation23. The 5-year partial prevalence (i.e., number of patients alive with a diagnosis of cancer for no longer than 5 years who are likely to receive primary treatment) is the best suited reference point to be compared with the number of treated cases in 2008 found in the present study. The 5-year partial prevalence amounted to ∼4840 patients with anal cancer in 2008 in Germany, assuming that 2%Citation24 of ∼241,990 patients with colorectal cancerCitation25 suffer from anal cancer. These 5-year partial prevalence data compare well to the 5774 hospitalizations found in the present study for 2008 in Germany.
The estimation of costs incurred by sick leave was based on the gender-specific extrapolation of the AOK dataCitation14 to the total German compulsory SHI member population in 2008Citation1Citation5. This extrapolation may have been limited by the fact that age distribution is not given in the AOK dataCitation14 and compulsory AOK members are of somewhat lower socioeconomic status than the average populationCitation26. However, in 2008, compulsory AOK members had 11.74 days of sick leave per sick leave case and 106.5 sick leave cases per 100 membersCitation27, while the total German compulsory SHI member population had 12.45 days of sick leave per sick leave case and 95.1 sick leave cases per 100 membersCitation28. Therefore, the bias introduced by the extrapolation of the cancer-specific sick leave data of the compulsory AOK membersCitation14 to the total German compulsory SHI member populationCitation15 may be minimal. In addition, the majority (60%) of the hospitalizations for anal cancer were for patients older than 60 years (); this is past the average age of retirement of 60.7 years in 2008 in GermanyCitation29. Hence, the above-mentioned minimal extrapolation bias only affects a relatively small amount of indirect costs due to sick leave of employed patients with anal cancer, i.e., those younger than the average retirement age.
Due to differences in study designs, national healthcare systems, unit costs, incidence patterns, and in cost components available, the results of the present study are difficult to compare with previous CoI analyses of HPV-related anal cancerCitation8–10. The results of our study, however, are similar to results found for FranceCitation8 with respect to hospital costs. Costs incurred by hospitalization amounted to €20.33 million (2006 values), with €17.89 million attributable to HPV-infection in FranceCitation8, compared to €29.50 million and €24.84 million (2008 values), respectively, in our study in Germany.
Conclusion
To our knowledge, this study is the first analysis to investigate the economic burden of anal cancer incurred by hospitalization, inpatient rehabilitation, and sick leave in Germany. The estimated annual costs of HPV-related anal cancer contribute to a significant economic burden of at least €28.72 million in Germany; this information could be useful for decision-makers when considering the potential impact of HPV vaccination on anal cancers in males and females in Germany. Indeed, the quadrivalent HPV vaccine has recently demonstrated high clinical efficacy on anal pre-cancers in malesCitation30; this should be considered when assessing the full potential benefits of a HPV vaccination program. Furthermore, these costs are under-estimated since, inter alia, outpatient management and management of precursor lesions could not be included as there is currently no data on this. Hence, further research is required to fully estimate the economic burden of HPV-related anal cancer in Germany.
Transparency
Declaration of funding
This study was funded by Sanofi Pasteur MSD, Lyon, France.
Declaration of financial/other interests
W.H. is an executive physician (Department of General Visceral, Vascular, and Thorax surgery) at the Bogenhausen Hospital, Teaching Hospital of the Technical University of Munich, Munich, Germany, and has received honoraria from Sanofi Pasteur MSD, Lyon, France (SPMSD). P.K.S. and X.C. are employees of IGES Institut GmbH, Berlin, Germany, and have worked on projects of IGES Institut GmbH that have been funded by SPMSD. V.R. is an employee of SPMSD, manufacturer of one HPV vaccine, and L.M. is a former employee of SPMSD. All authors contributed equally to conception and design, acquisition, analysis, and interpretation of the data, as well as to drafting and critical review of the article. All authors have read and approved the final version to be published. JME Peer Reviewers on this manuscript have no relevant financial relationships to disclose.
Acknowledgments
The information contained in this manuscript was presented in part at the 27th International Papillomavirus Conference, Berlin, Germany, September 17–22, 2011; and at the 14th Annual European Congress of the International Society for Pharmacoeconomics and Outcomes Research, Madrid, Spain, November 5–8, 2011.
References
- Uronis HE, Bendell JC. Anal cancer: an overview. Oncologist 2007;12:524-34
- Abbasakoor F, Boulos PB. Anal intraepithelial neoplasia. Br J Surg 2005;92:277-90
- Curado MP, Edwards B, Shin B, et al., editors. Cancer incidence in five continents, Vol. IX. IARC Scientific Publications No. 160. Lyon, France: International Agency for Research on Cancer, 2007
- Frisch M, Fenger C, van den Brule AJC, et al. Variants of squamous cell carcinoma of the anal canal and perianal skin and their relation to human papillomaviruses. Cancer Res 1999;59:753-7
- Parkin DM, Bray F. Chapter 2: the burden of HPV-related cancers. Vaccine 2006;24(3 Suppl):S11-S25
- de Vuyst H, Clifford GM, Nascimento MC, et al. Prevalence and type distribution of human papillomavirus in carcinoma and intraepithelial neoplasia of the vulva, vagina and anus: a meta-analysis. Int J Cancer 2009;124:1626-36
- Daling JR, Madeleine MM, Johnson LG, et al. Human papillomavirus, smoking, and sexual practices in the etiology of anal cancer. Cancer 2004;101:270-80
- Abramowitz L, Rémy V, Vainchtock A. Economic burden of anal cancer management in France. Rev Epidemiol Sante Publique 2010;58:331-8
- Ekwueme DU, Chesson HW, Zhang KB, et al. Years of potential life lost and productivity costs because of cancer mortality and for specific cancer sites where human papillomavirus may be a risk factor for carcinogenesis – United States, 2003. Cancer 2008;113(10 Suppl):2936-45
- Hu D, Goldie SJ. The economic burden of noncervical human papillomavirus disease in the United States. Am J Obstet Gynecol 2008;198:500.e1-e7
- Destatis – Statistisches Bundesamt Deutschland (Federal Statistical Office Germany). Tiefgegliederte Diagnosedaten der Krankenhauspatientinnen und -patienten 2008. https://www-ec.destatis.de/csp/shop/sfg/bpm.html.cms.cBroker.cls?cmspath=struktur,vollanzeige.csp&ID=1025095. Accessed January 4, 2011
- InEK – Institut für das Entgeltsystem im Krankenhaus (Institute for the Hospital Remuneration System in Germany). GDRGBrowser_2008_Par21_100202.zip (G-DRG V2009 Daten 2008 gem. § 21 KHEntgG - G-DRG Browser) 2010. www.g-drg.de/cms/index.php/Datenveroeffentlichung_gem._21_KHEntgG. Accessed March 15, 2010
- DRV – Deutsche Rentenversicherung (German Public Pension Insurance). Statistik der Deutschen Rentenversicherung. Band 174. Rehabilitation 2008. Berlin: Deutsche Rentenversicherung, 2009
- GBE – Gesundheitsberichterstattung des Bundes (Federal Health Monitoring Germany). Arbeitsunfähigkeit bei AOK-Mitgliedern ohne Rentner. Jahr 2008: Arbeitsunfähigkeitsfälle, Arbeitsunfähigkeitstage, Tage je Fall (Gliederungsmerkmale: Jahre, Deutschland, Geschlecht, ICD-10). www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=3&p_aid=91546134&nummer=683&p_sprache=D&p_indsp=-&p_aid=70513394. Accessed December 7, 2010
- BMG – Bundesministerium für Gesundheit (German Federal Ministry of Health). Mitgliederstatistik KM6, 2008. www.bmg.bund.de/fileadmin/redaktion/excel_statistiken/krankenversicherung/KM6-juli-08.xls. Accessed January 11, 2011
- Platzer H. Zukünftige Vergütungsstrukturen der Krankenhäuser. 2008. www.oberender-online.de/fileadmin/oberender/pdf/Platzer_ExpertentagungUniBayreuth_08052008.pdf. Accessed December 12, 2010
- von der Schulenburg JM, Prenzler A, Schurer W. Cancer management and reimbursement aspects in Germany: an overview demonstrated by the case of colorectal cancer. Eur J Health Econ 2010;10(1 Suppl):S21-6
- von der Schulenburg JM, Greiner W, Jost F, et al. German recommendations on health economic evaluation: third and updated version of the Hanover Consensus. Value Health 2008;11:539-44
- Destatis – Statistisches Bundesamt Deutschland (Federal Statistical Office Germany). Statistical Yearbook 2010 for the Federal Republic of Germany including International tables. Wiesbaden: Statistisches Bundesamt, 2010
- Brecht JG, Poldrugo F, Schädlich PK. Alcoholism: the cost of illness in the Federal Republic of Germany. Pharmacoeconomics 1996;10:484-93
- Brecht JG, Schädlich PK. Burden of illness imposed by osteoporosis in Germany. Eur J Health Econ 2000;1:26-32
- Schädlich PK, Brecht JG. Burden of illness imposed by venous thromboembolism as an original disease in Germany. Perfusion 2003;16:250-6
- SPMSD – Sanofi Pasteur MSD. Expected numbers of anal cancer incident cases in 2008. Lyon: Sanofi Pasteur MSD, 2011
- Onmeda. Analkarzinom (Analkrebs). Häufigkeit 2010. www.onmeda.de/krankheiten/analkarzinom-definition-haeufigkeit-1411-3.html. Accessed July 10, 2011
- RKI – Robert Koch-Institut. Verbreitung von Krebserkrankungen in Deutschland. Entwicklung der Prävalenzen zwischen 1990 und 2010. Beiträge zur Gesundheitsberichterstattung des Bundes. Berlin: Robert Koch-Institut, 2010
- Schnee M. Sozioökonomische Strukturen und Morbidität in den gesetzlichen Krankenkassen. In: Böcken J, Braun B, Amhof R, editors. Gesundheitsmonitor 2008. Gütersloh: Verlag Bertelsmann Stiftung, 2008. p 88-104
- GBE – Gesundheitsberichterstattung des Bundes (Federal Health Monitoring Germany). Arbeitsunfähigkeit bei AOK-Mitgliedern ohne Rentner. Jahr 2008: Arbeitsunfähigkeitstage, Arbeitsunfähigkeitsfälle, Tage je Fall (Gliederungsmerkmale: Jahre, Kassenart, Versichertengruppe). www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/WS0100/_XWD_FORMPROC?TARGET=&PAGE=_XWD_1074&OPINDEX=7&HANDLER=_XWD_CUBE.SETPGS&DATACUBE=_XWD_1100&D.003=1000004&D.008=3078&D.009=3053. Accessed January 22, 2011
- GBE – Gesundheitsberichterstattung des Bundes (Federal Health Monitoring Germany). Arbeitsunfähigkeit bei Mitgliedern der gesetzlichen Krankenkassen insgesamt ohne Rentner. Jahr 2008: Arbeitsunfähigkeitstage, Arbeitsunfähigkeitsfälle, Tage je Fall (Gliederungsmerkmale: Jahre, Kassenart, Versichertengruppe). www.gbe-bund.de/oowa921-install/servlet/oowa/aw92/dboowasys921.xwdevkit/xwd_init?gbe.isgbetol/xs_start_neu/&p_aid=i&p_aid=60283303&nummer=267&p_sprache=D&p_indsp=-&p_aid=86537257. Accessed January 22, 2011
- DRV – Deutsche Rentenversicherung (German Public Pension Insurance). Statistik der Deutschen Rentenversicherung. Band 173. Rentenzugang 2008. Berlin: Deutsche Rentenversicherung, 2009
- Giuliano AR, Palefsky JM, Goldstone S, et al. Efficacy of quadrivalent HPV vaccine against HPV infection and disease in males. N Engl J Med 2011;364:401-11