Abstract
Background:
Pressure ulcers are a major problem in Danish healthcare with a prevalence of 13–43% among hospitalized patients. The associated costs to the Danish Health Care Sector are estimated to be €174.5 million annually. In 2010, The Danish Society for Patient Safety introduced the Pressure Ulcer Bundle (PUB) in order to reduce hospital-acquired pressure ulcers by a minimum of 50% in five hospitals. The PUB consists of evidence-based preventive initiatives implemented by ward staff using the Model for Improvement.
Objective:
To investigate the cost-effectiveness of labour-intensive efforts to reduce pressure ulcers in the Danish Health Care Sector, comparing the PUB with standard care.
Methods:
A decision analytic model was constructed to assess the costs and consequences of hospital-acquired pressure ulcers during an average hospital admission in Denmark. The model inputs were based on a systematic review of clinical efficacy data combined with local cost and effectiveness data from the Thy-Mors Hospital, Denmark. A probabilistic sensitivity analysis (PSA) was conducted to assess the uncertainty.
Results:
Prevention of hospital-acquired pressure ulcers by implementing labour-intensive effects according to the PUB was cost-saving and resulted in an improved effect compared to standard care. The incremental cost of the PUB was −€38.62. The incremental effects were a reduction of 9.3% prevented pressure ulcers and 0.47% prevented deaths. The PSAs confirmed the incremental cost-effectiveness ratio (ICER)’s dominance for both prevented pressure ulcers and saved lives with the PUB.
Conclusion:
This study shows that labour-intensive efforts to reduce pressure ulcers on hospital wards can be cost-effective and lead to savings in total costs of hospital and social care.
Key limitations:
The data included in the study regarding costs and effects of the PUB in Denmark were based on preliminary findings from a pilot study at Thy-Mors Hospital and literature.
Introduction
In the Danish healthcare system, pressure ulcers have a high prevalence of 13–43% among hospitalized patientsCitation1,Citation2. The high prevalence of pressure ulcers in Denmark is not unique, and similar prevalence tendencies exist in many western countriesCitation2–5. The annual costs of pressure ulcers to the Danish healthcare system are estimated to be €174.5 million, and the average cost of treating a pressure ulcer ranges from €1643 to €22,591Citation2. Pressure ulcers are not only very costly; they also result in decreased quality of life and increased mortalityCitation6.
Pressure ulcers often develop during hospitalization due to immobilization and potentially underlying diseaseCitation7,Citation8. Pressure ulcers can be classified into stages (I–IV) depending on depth and diameter. A preceding stage for pressure ulcers, labelled stage 0, also exists to identify early signs of tissue damageCitation1,Citation9. The more severe stages are associated with a higher risk of complications such as critical colonization, cellulitis, osteomyelitis, and potentially deathCitation5.
The Danish Society for Patient Safety (DSPS) developed the Pressure Ulcer Bundle (PUB) to reduce the prevalence of pressure ulcers in Danish hospitals. It was tested as a pilot study at five Danish hospitals in the period 2010–2013Citation10. The PUB consists of guidelines on how to optimize and secure the use of already existing tools and on structuring the preventive initiatives. The four elements of the PUB are:
All newly hospitalized patients are assessed for the risk of developing pressure ulcers.
Patients at risk of developing pressure ulcers are reassessed daily.
Patients at risk should be nutrition screened.
Patients at risk should be mobilized optimally and decompression should be used when repositioning in accordance with guidelinesCitation9.
Together, the four elements constitute the best practice in the field of pressure ulcer preventionCitation10. The elements were adjusted and implemented in the daily routine at the five Danish hospitals using the Model for Improvement, which includes the model tool “Plan, Do, Study, Act” (PDSA) and the breakthrough method of scaling initiatives from small tests to larger tests before full implementation. The Model for Improvement aims to continuously improve and reflect on the methods used by the involved hospital staffCitation11.
The aim of this study was to estimate the cost-effectiveness of a full implementation of the PUB at a national level in order to inform a decision in the Danish regions (i.e., the owners of the public hospitals). This study used a public healthcare perspective including costs both during hospital admission and after discharge. Hospital acquired pressure ulcers often require long-term care subsequent to admission, which is treated outside the hospital sector by community hired nurses caring for the patients in their own homesCitation5. Effective prevention strategiesCitation12 combined, including supportive surfaces, daily patient repositioning, and optimizing the patient’s nutrition can constitute a high cost when considering the reallocation of nursing time and materialsCitation13,Citation14. On the other hand, implementing preventive strategies may be more cost-effective when comparing to a standard care where it is possible that prevention guidelines are overlookedCitation15. Previous economic studies in the field of prevention of pressure ulcers have estimated the cost of individual treatment strategies such as supportive surfacesCitation16,Citation17. This study is, to our knowledge, the first to estimate the impact on cost-effectiveness of labour-intensive quality improvement initiatives to reduce the incidence of pressure ulcers in Danish hospitals.
Methods
Design of the study
To evaluate whether labour-intensive efforts to prevent pressure ulcers are “worth the struggle”, a cost-effectiveness analysis was conducted. This type of analysis assesses the costs, effects, and health gains of two or more alternatives.
A decision analytic model was developed to estimate the expected incremental cost-effectiveness ratio (ICER) of the PUB compared to the current practice, standard care. The model was constructed using the software TreeAge (Pro 2010, TreeAge Software, Williamstown, MA). All model data input were extracted from best available evidence and primary data collection at Thy-Mors Hospital. Thy-Mors Hospital was used as the representative of the five hospitals where the PUB has been implemented.
Model
The decision analytic model was constructed as a decision tree and the time frame was set to the maximum length of healing time for a pressure ulcer plus potential complications. The healing time for pressure ulcers were derived from the literatureCitation5 and the maximum healing time of a pressure ulcer was not found to exceed one year. Therefore, costs and effects were not discountedCitation18.
For the standard care arm, no specific pressure ulcer prevention strategy was used. In the PUB arm of the model, it was assumed that 100% of the patients experienced an admission with full adherence to all the elements of the PUB, leading to overall reduction of pressure ulcers by 50%.
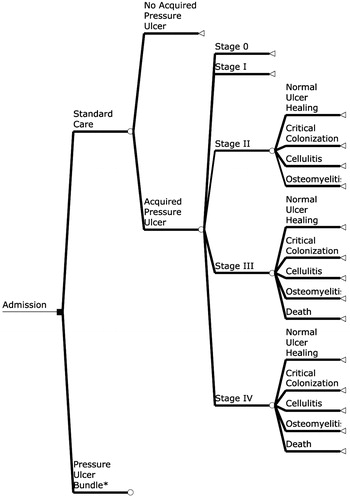
During hospital admission, patients could experience occurrence of the pressure ulcer preceding stage, stage 0, pressure ulcers I–IV, complications, and death. The model was initiated at admission, illustrated in the decision tree (see ), and the patients were tracked through one of the two arms in the model through a single course.
Figure 1. Simplified view of the decision analytic model. From the left, the square-shaped decision node represents the choice between standard care and treatment according to the Pressure Ulcer Bundle. Each circle-shaped chance node represents the probability of acquiring or not acquiring a pressure ulcer, the probabilities of acquiring different stages of pressure ulcers and probabilities of acquiring different kinds of complications, or normal ulcer healing. The triangular-shaped terminal nodes illustrate the end of each possible path in the decision tree and are associated with individual costs and effects. *Indicates that the arm of the “Pressure Ulcer Bundle” is structured exactly as the arm of the “Standard Care”, except that the probability of acquiring a pressure ulcer is reduced by 50%.
Costs
Calculations of costs followed international guidelines for health economic evaluationsCitation18. Only the marginal costs of labour-intensive improvements were included in the analysis. All unit costs were collected using the currency Danish Krone (DKK) for the year 2011 and converted into Euros (exchange rate DKK 749 = 100 €).
Initially all relevant resources for the model were identified and valued. The additional resource use related to the PUB compared to standard care included giving information to the patients at admission, systematic documentation of the daily risk screening, and the continuous work using the Model for Improvement, PDSA. If a patient was identified as being at risk of developing a pressure ulcer or as having one, an additional effort was performed by frequent repositioning of the patient and additional documentation in the electronic medical record system. All costs were based on micro-costing and are listed in . The implementation costs of the PUB were only partially captured in the analysis by the Model for Improvement where a group of dedicated nurses continuously reflected on and developed the PUB.
Table 1. Time and costs estimated for each element in the PUB. Time illustrates the number of minutes per day the nurses use to conduct the elements per patient. Cost is based upon the average salary for a nurse. Total cost is calculated by cost per day multiplied by the number of days.
The total costs related to pressure ulcers included both care during hospital admission and care outside the hospital. The total amount of labour associated with pressure ulcer care depended on the pressure ulcer severity and the healing time. The healing time was derived from the literature along with the average time spent on pressure ulcer care for each pressure ulcer stage. Costs of the most common complications – critical colonization, cellulitis, osteomyelitis, and death – were further included in the calculations. All costs related to complications were valued using a gross-costing method with unit costs taken from the Danish Diagnosis Related Group (DRG) systemCitation19 ().
Table 2. Model input.
The main type of resource usage in both the prevention and care of pressure ulcers was the time spent by the nurses. In order to estimate the nurses’ time, a combination of best available literature and expert opinions were used. A semi-structured interview with a group of PUB specialized nurses from the surgical ward at Thy-Mors Hospital was performed to estimate the extra resources associated with the PUB. The average salary including pension and bonuses for nurses in the public healthcare system was used to estimate the opportunity costs of the extra resourcesCitation20. The salary was estimated by cost per effective hour for each personnel category.
Probabilities
Probabilities for the different health stages included in the decision model were derived from the literature (see ). The probabilities of developing pressure ulcers during a hospitalization were based on the existing Danish prevalence studies estimating both the prevalence of hospital acquired pressure ulcers, stages I–IV, and the early signs of pressure ulcers, stage 0. The baseline was set as a weighted mean calculated from the estimated prevalence and number of patients included in each study. These prevalence studies were conducted following the same methodology, and included all hospital admitted patients above the age of 16 (average age of 72), except patients on intensive, gynaecology and obstetrics wardsCitation1,Citation2. Furthermore, the literature describes that pressure ulcers normally develop within 48 hours after admission, hence it was assumed that pressure ulcers would develop on the second day of admissionCitation21.
Data on the risks of developing complications from different stages of pressure ulcers were taken from a systematic literature reviewCitation5. The risk of death from pressure ulcers was extracted from a Swedish study which found that only the more severe stages (III–IV) of pressure ulcers lead to increased mortalityCitation22.
Effects
The effects of the PUB were measured as the number of prevented pressure ulcers and the number of saved lives. In accordance with the objective of the PUB, developed by the DSPS, the aim was defined as a 50% reduction of hospital-acquired pressure ulcers, and this goal was expected to be a conservative estimateCitation4,Citation8,Citation23. In the model, this expected outcome was incorporated in the decision model as a 50% reduction in prevalence and pressure ulcer associated mortality. The effect goal of a 50% reduction was also supported by other studies showing a reduction of approximately 50%Citation4,Citation23.
Sensitivity analysis
One-way sensitivity analysis was performed on all input parameters. Each parameter was adjusted one at a time by ±25% or a range based on the literature to assess the influence of the individual parameter uncertainty.
A probabilistic sensitivity analysis (PSA) with second-order Monte Carlo simulations was carried out to recalculate the expected ICER 10,000 times to make an empirical sample distribution of the expected ICER (i.e., simulating 10,000 trials). The advantage of this type of sensitivity analysis is that it considers the overall uncertainty around the ICER, taking all parameter uncertainties into accountCitation18. In the PSA, all parameters were assigned a distribution based on best available evidence. All cost parameters were assigned with gamma distributions, and all probability parameters were assigned with beta distributions, as recommended by Briggs et al.Citation24 with a best-worst case variation of +/−25%. The probability of a 50% reduction in pressure ulcers, as an effect of PUB, was also given as a beta distribution approximated from the literature.
The results of the Monte Carlo simulations are illustrated with a cost-effectiveness scatter plot with 95% confidence ellipses. Finally, a cost-effectiveness acceptability curve (CEAC) shows the probability of the PUB intervention being cost-effective compared to standard care, at different willingness-to-pay thresholds.
Results
Cost-effectiveness analysis
The results indicate that an implementation of the PUB in the Danish healthcare system yields both lower costs and greater effects in relation to prevented pressure ulcers and saved lives. The costs of the standard care approach were €118.45 per patient and the costs associated with the PUB were €79.83 per patient. Thus, the potential net savings were estimated to be € −38.62 per patient.
During the standard care approach 81.4% of the patients experienced an admission without developing pressure ulcers, whereas the percentage increased to 90.7% during the PUB. This leads to an incremental effect of a 9.3% reduction in pressure ulcers for the PUB.
The survival rate was 99.06% for the standard care approach and 99.53% for the PUB, respectively. The PUB was associated with an incremental effect of 0.47% of prevented deaths.
Sensitivity analysis
The result of the one-way analysis showed that the ICER was robust to the parameter uncertainty within the defined range, thus the PUB continued to be cost-effective in all cases, except when the prevalence of pressure ulcers was influenced. Hence, a threshold analysis was performed on the parameter pressure ulcer prevalence. The threshold value was found in the scenario where the PUB only reduces the prevalence of pressure ulcers by 23.2% instead of the targeted 50%. In this case, the prevalence of pressure ulcers would be 30.47%. If the effect after this point is lowered further, the PUB is no longer the obvious dominant choice and the cost-effectiveness would depend on the willingness-to-pay of the payer.
The result of the conducted PSA is illustrated in an incremental cost-effectiveness scatter plot and a CEAC. illustrates the second-order Monte Carlo simulations conducted for the effect goal – prevented pressure ulcers. The simulated ICER values are found in the south-eastern quadrant, indicating that the PUB is both cost-saving and reduces pressure ulcer prevalence. The CEAC () illustrates that the PUB is cost-effective in 92.7% of the simulations at a willingness-to-pay of €0.
Figure 2. Incremental cost-effectiveness scatter plot for the effect goals (A) prevented deaths and (B) prevented pressure ulcers.
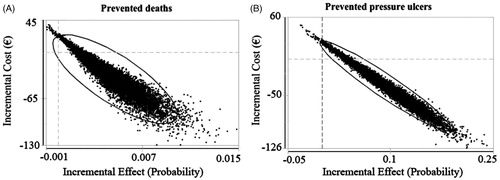
Figure 3. Cost-effectiveness acceptability curve for the effect goals saved lives and prevented pressure ulcers.
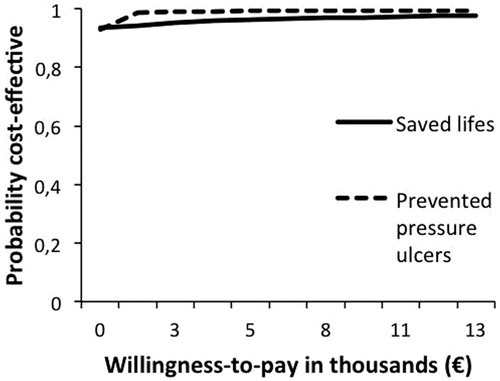
illustrates the second-order Monte Carlo simulations conducted for the effect goal – saved lives. The simulated ICER values are also found in the south-eastern quadrant, indicating that the PUB is both cost-saving and reduces mortality. The CEAC (), shows that the PUB is cost-effective in 93.0% of the simulations at a willingness-to-pay of €0.
Discussion
In this study, the possible cost-effectiveness of implementing the PUB in the Danish healthcare sector, compared to a standard prevention and treatment regime of pressure ulcers, was investigated. The results showed that the PUB was a dominating intervention with better health outcomes and cost-savings. The PSA was used to strengthen the results and confirmed the robustness of the conclusion. Hence, by adopting the PUB the healthcare sector would benefit in both patient outcomes and financial savings.
The primary goal of implementing the PUB in a Danish healthcare setting was to reduce the prevalence of pressure ulcers by 50%. The goal of a 50% reduction is set due to experiences from other countries where similar prevention strategies were implemented. Studies implemented in the USA have resulted in a 33–55% pressure ulcer prevalence reduction and Irish hospitals managed to eliminate hospital acquired pressure ulcers completelyCitation4,Citation8,Citation23.
Health economic modelling is always associated with an amount of uncertainty, especially in this cost-effectiveness analysis (CEA) where the results are based on preliminary findings from the PUB pilot study. Yet, our findings are supported by a similar study conducted by Padula et al.Citation3 in 2011, also finding systemized prevention of pressure ulcers cost-effective compared to standard care.
This study is limited by several factors affecting the cost-effectiveness of the PUB. First, we estimated the opportunity costs of labour in terms of gross wages and numbers of effective working hours spent on the PUB. The main cost related to both prevention and pressure ulcer care was time spent by the nurses. Measuring the cost of time as the expenditure constituted by salary is a standard method in economic evaluations, but it does not necessarily reflect the true marginal value of time, which might be higher or lowerCitation18. The extra amount of labour in relation to the preventive measures in the PUB results in a net saving of time, as the nurses reversely save time normally spent on ulcer care, complications, and death. In addition, both Bennett et al.Citation5 and Schuurman et al.Citation25 conclude that the main cost driver in pressure ulcer care can be ascribed to the nursing salary. These conclusions also support the fact that this study did not include the costs related to materials. Studies investigating the cost-effectiveness of pressure-redistribution foam mattresses and other types of underlay found that these were cost-savingCitation26,Citation27. Hence, including the use of mattresses may even have strengthened the findings of this study.
Second, only extra marginal costs regarding the day-to-day running of the PUB have been estimated and included in this analysis. “Running costs” of the PUB were included in the continuous use of the Model for Improvement, PDSA. The implementation cost would be non-recurrent and reflect the resources spent on designing the intervention, education of staff, and evaluation. The implementation cost was not estimated as the PUB is a pilot study, hence not reflecting a national implementation. Furthermore, the implementation cost would have to be accounted over a longer time period, leading to limited annual costs. Increased costs were already included in the PSA and did not alter the findings.
Third, regarding the prevalence of hospital acquired pressure ulcers, a clear baseline was not measured when the PUB was implemented; hence Danish prevalence studies were applied to estimate a national baseline. The estimated prevalence might be biased, as the Danish prevalence studies did not outline to which extent the patient had a pressure ulcer prior to hospital admission, or if the pressure ulcer developed during the hospital stay. In this study, it was assumed that a pressure ulcer developed on the second day subsequent to admission, and therefore not prior to an admission. Furthermore, the estimated prevalence of hospital acquired pressure ulcers in Denmark was similar to studies from other European countries and the USACitation5,Citation27,Citation28. The pressure ulcer healing times were estimated from current available literature, where a worsening of pressure ulcer grade corresponded to a prolonged healing time. However, several factors impact on the healing time of a pressure ulcer, such as the ulcer size and patient comorbidity. Expert opinions from nurses at Thy-Mors Hospital revealed that pressure ulcer healing time is often longer than the estimates from the efficacy literature; hence we have chosen a conservative estimate.
Only prevented pressure ulcers and saved lives were included as effect outcomes for this study. For future studies, quality-adjusted life years (QALY) could have been implemented as an effect outcome as well. The health related quality of life of a patient developing a pressure ulcer is susceptible to be altered negatively due to the pain, discomfort, and disability arising with pressure ulcers. No reliable literature regarding QALY for pressure ulcer patients exist, however, studies have included QALY estimations based on expert opinions and not from clinical studies. The fact that pressure ulcers often develop secondary to other illnesses complicates QALY estimation and might explain the lack of studies investigating the quality of life for pressure ulcer patients.
This analysis shows that labour intensive efforts from healthcare professionals to prevent pressure ulcers in a Danish hospital setting can be extremely cost-effective. In line with our findings, evidence indicates that quality improvements can be cost-saving, which have inspired the UK National Health Service to rely on this type of strategy in order to save money in the futureCitation29. However, it is important to underpin that implementation of quality improvement strategies depend on the culture among the clinical staff at the implementation sites and the scale-up of this type of intervention is complexCitation30. This cultural aspect questions the transfer and sustainability of the quality improvement strategy in a broad national perspective and a long-time horizon. That is why a decision to implement a quality improvement strategy is not recommended to solely rely on the cost-effectiveness of the strategy, but alongside a contextual evaluation of the strategy.
Conclusion
This study shows that labour-intensive efforts to reduce pressure ulcers at hospital wards can be cost-effective and lead to savings in total costs of hospital and social care.
Transparency
Declaration of funding
This study did not have funding or a financial relationship with an external sponsor.
Declaration of financial/other relationships
The authors have no relevant financial relationship to disclose. JME peer reviewers of this manuscript have no relevant financial relationships to disclose.
Acknowledgements
The authors thank the nurses at K1, Thy-Mors Hospital for sharing their expertise, data, and inputs, all of which contributed to this article.
References
- Bermark S, Jensen LB, Krejberg E, et al. Seks prævalensundersøgelser for tryksår. Sår 2009;17(4):203-10
- Dorsche KM, Fremmelevholm A. Forekomst af decubitus på hospitalerne. Ugeskr læger 2010;172(8):601-6
- Padula WV, Mishra MK, Makic MBF, et al. Improving the quality of pressure ulcer care with prevention: a cost-effectiveness analysis. Med Care 2011;49(4):385-92
- Sendelbach S, Zink M, Peterson J. Decreasing pressure ulcers across a healthcare system: moving beneath the tip of the iceberg. J Nurs Adm 2011;41(2):84-9
- Bennett G, Dealey C, Posnett J. The cost of pressure ulcers in the UK. Age Ageing 2004;33(3):230-5
- National Quality Forum. Safe Practices for Better Healthcare – 2009 Update. 2009. Available at http://www.qualityforum.org/Publications/2009/03/Safe_Practices_for_Better_Healthcare–2009_Update.aspx
- McCance KL, Huether SE. Pathophysiology. 5th ed. St. Louis, MO: Elsevier Mosby, 2006
- Dansk Selskab for Patientsikkerhed. Patientsikkerhed - Forebyggelse af fejl og skader - Sikker Patient. Available at http://www.sikkerpatient.dk/. [Last accessed 7 May 2012]
- Pressure Ulcer Advisory Panel. Guidelines til tryksår. 2009:28:12-13
- Patientsikkert Sygehus. Tryksårpakken. 2010. Available at http://www.sikkerpatient.dk/professionelle/patientsikkert-sygehus/spor-og-pakker/alle-pakker/tryksaarpakken.aspx
- Langley GJ, Moen R, Nolan KM. The improvement guide: a practical approach to enhancing organizational performance. 2nd ed. San Franscisco: Jossey-Bass, 2009:23-5
- Reddy M, Gill SS, Rochon PA. Preventing pressure ulcers: a systematic review. JAMA 2006;296(8):974-84
- Ayello BEA, Lyder CH. Protecting patients from harm: preventing pressure ulcers. Nursing 2007;37:36-40
- Pappas SH. The cost of nurse-sensitive adverse events. J Nurs Adm 2008;38(5):230-6
- Gold M, Siegel J, Russell L. Cost-effectiveness in health and medicine. New York: Oxford University Press, 1996:276-303
- Legood R, McInnes E. Pressure ulcers: guideline development and economic modelling. J Adv Nurs 2005;50(3):307-14
- Iglesias C, Nixon J, Cranny G, et al. Pressure relieving support surfaces (PRESSURE) trial: cost effectiveness analysis. BMJ (Clinical research ed.) 2006;332(7555):1416:1-5
- Drummond M., Schulpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press, 2005:1-375
- Ministeriet for sundhed og forebyggelse. Takster 2011. Available at http://www.sum.dk/Sundhed/DRG-systemet/Takster/2011.aspx
- Det Fælleskommunale Løndatakontor. LOPAKS. 2011. Available at http://fldnet.dk/statistik/lpx7/
- Sterner E, Lindholm C, Berg E, et al. Category I pressure ulcers: how reliable is clinical assessment? Orthoopaedic Nurs 2011;30(3):194-207
- Lindholm C, Bergsten A, Berglund E. Chronic wounds and nursing care. J WoundCare 1999;8(1):5-10
- Gibbons W, Shanks H, Kleinhelter P, et al. Eliminating facility-acquired pressure ulcers at Ascension Health. The joint commission journal on quality and patient safety 2006;41:84-9
- Briggs A, Schulper M, Clarkton K. Decision modelling for health economic evaluation. 1st ed. Oxford: Oxford University Press, 2006
- Schuurman J, Ramshorst BV. Economic evaluation of pressure ulcer care: a cost minimization analysis of preventive strategies. Nurs Econ 2009;27(6):390-415
- Pham B, Teague L, Mahoney J, et al. Support surfaces for intraoperative prevention of pressure ulcers in patients undergoing surgery: a cost-effectiveness analysis. Surgery 2011;150(1):122-32
- Pham B, Teague L, Mahoney J, et al. Early prevention of pressure ulcers among elderly patients admitted through emergency departments: a cost-effectiveness analysis. Ann Emerg Med 2011;58(5):468-78
- Lahmann N, Dassen T, Kottner J. Frequency of pressure ulcers in German hospitals. Das Gesundheitswesen 2012;74(12):793-7
- NHS improving quality. Our strategic intent. 2013:1-11
- Øvretvit J. Does improving quality of care save money? A review of evidence of which improvements to quality reduce costs to health service providers. London: The Health Foundation; 2009:95