Abstract
Background:
Atrial fibrillation (AF) is the most common cardiac rhythm disturbance in the US, with an estimated prevalence of 2.7–6.1 million persons in 2010.
Objective:
This study evaluates the progression of daily hospitalization costs among non-valvular atrial fibrillation (NVAF) patients treated with anticoagulant therapy.
Methods:
A claims analysis was conducted with Premier Perspective Comparative Hospital Database records from January 2009–March 2013. Patients of 18 years or older who were diagnosed with NVAF and used anticoagulant therapy were studied. Treatment patterns and mean daily costs of hospitalization per patient as well as total costs of hospitalization were reported. Comparisons of mean daily costs with those of the previous day were presented to identify statistical cost differences between hospitalization days.
Results:
A total of 375,560 patients were identified; 67,017 with AF as admitting/primary diagnosis, and 308,543 with AF as a secondary diagnosis. The mean age of the overall population, primary AF diagnosis cohort, and secondary AF diagnosis cohort was 73.8, 67.9, and 75.0 years, while their proportion of females was 46.3%, 45.6%, and 46.5%, respectively. The mean length of stay was 6.8 days, 3.7 days, and 7.5 days for the overall population, the primary AF diagnosis cohort, and the secondary AF diagnosis cohort, respectively. For all cohorts, mean daily costs stabilized on the third day (overall population: $2103; primary AF diagnosis cohort: $1505; secondary AF diagnosis cohort: $2208).
Limitations:
Claims data may have contained inaccuracies or omissions in coded procedures, diagnoses, or pharmacy claims.
Conclusion:
The study showed that daily hospitalization costs for NVAF patients stabilized on the third day of hospitalization and that any reduction or prolongation in hospital length of stay could have a significant impact on the cost burden associated with AF.
Introduction
Atrial fibrillation (AF) is the most common cardiac rhythm disturbance in the US. An estimated 2.7–6.1 million persons in 2010 suffered from AF, and the prevalence is expected to rise to between 5.6–15.9 million in 2050Citation1–5. The incremental cost burden of AF patients compared to that of non-AF patients was estimated at $26 billion in the US in 2010, with more than 50% of this amount being hospitalization costsCitation5–8. Studies have reported that the annual total direct cost per patient after a diagnosis of AF is estimated at $20 670, and that the principal cost driver of the burden of AF is hospitalization, accounting for 44–75% of the total AF costsCitation4,Citation7,Citation8.
Anticoagulant agents are regularly used by patients with non-valvular atrial fibrillation (NVAF) for stroke prevention, and warfarin and other oral vitamin-K antagonist (VKA) agents have been the only oral anticoagulant drugs available for decadesCitation9. Recently, non-VKA oral anticoagulants (NOACs) have been approved for the treatment of NVAF by the US Food and Drug AdministrationCitation10–13. Studies of anticoagulants have reported reductions in hospital length of stay (LOS) among NVAF patients treated with NOAC agents compared to patients treated with warfarin, which could potentially lead to reduced hospitalization costsCitation14–16.
To the best of our knowledge, there is currently no information on the progression of daily hospitalization costs among NVAF patients. Calculating daily costs allows the impact of any increase or decrease in LOS due to different therapies to be quantified, which is not usually done in studies that report total hospitalization costs. Therefore, the scope of this paper is to quantify the progression of daily hospitalization costs among patients with a primary or a secondary diagnosis of AF.
Methods
Data source
This study was based on data from the Premier Perspective Comparative Hospital Database covering the period from January 2009 to March 2013. Premier is the largest hospital-based database in the US and contains detailed information for more than 45 million inpatient discharges from over 600 acute-care hospitals across all US regions. Data elements include patient demographics and primary and secondary diagnoses for every hospitalization as well as all procedures, and other department activities. In comparison with centralized healthcare claims recorded by insurance companies, patients’ medical information available in the Premier database comes from records collected for billing purposes at the hospital level. Actual costs including fixed (overhead) and variable (direct) cost are reported for each procedure of a hospital stay and are collected by Premier directly from the hospital cost accounting systems. These include costs for all supplies, labor, depreciation of equipment, etc. Premier data are de-identified and fully compliant with all HIPAA privacy and security requirements to protect participant anonymity and confidentiality.
Study design
A retrospective cohort design was used to quantify the progression of daily hospitalization costs among patients with an admitting/primary or secondary AF diagnosis (ICD-9-CM: 427.31), and the index date was defined as their first hospitalization day. Although the current study was conducted on a different population, it employed a similar study design as a study published in Thrombosis Research by the present authors on a population of patients with venous thromboembolismCitation17.
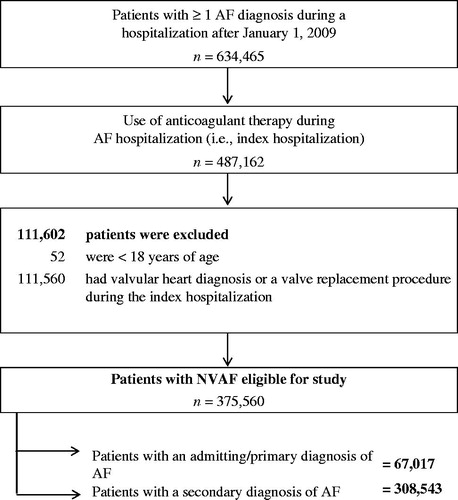
Patients included in the analysis were 18 years of age as of the date of index hospital admission and used anticoagulant therapy during their hospitalization. Patients with valvular heart disease or valve replacement procedure during the hospital stay were excluded from the study. The observation period for the analysis was the hospital stay. In addition to the overall cohort, patients were further stratified into two distinct groups: (a) patients with an admitting or primary AF diagnosis during their hospital stay and (b) patients with a secondary AF diagnosis during their hospital stay.
Study endpoints
The primary endpoint of the analysis was the NVAF patients’ daily costs of hospitalization. The mean total hospitalization costs were also reported. Exploratory end-points included stratified hospitalization costs in mutually exclusive categories (i.e., room and board, nursing, surgery, supply, laboratory, pharmacy, and other costs). In addition, pharmacy costs were further stratified by the top five types of medication used.
Statistical analysis
Descriptive statistics were used to summarize patients’ characteristics evaluated at the index hospital admission. Means, medians, and standard deviations (SDs) were reported for continuous variables, while frequencies and percentages were reported for categorical variables.
Lengths of stay and treatment characteristics (e.g., number of different medications used, number of doses [i.e., oral or injections] per day) were evaluated during the hospitalization. Frequencies and percentages were reported for categorical variables, and means, medians, and SDs were reported for continuous variables.
Mean hospitalization costs were reported per day for the first 7 days, and mean daily costs were reported for the ranges of days 8–14 and days 15–30. Overall mean daily costs of hospitalizations per patient as well as mean total costs of hospitalizations were reported. Statistical comparisons were made between the daily costs using standardized difference to assess the day where the costs became stable (i.e., standardized difference <10%). The standardized difference was calculated by dividing the absolute difference in the mean costs of two consecutive days by their pooled standard deviation. The pooled standard deviation was calculated as the square root of the average of the squared standard deviationsCitation18–20. All costs were adjusted to the 2013 $US value based on the medical care component of the Consumer Price Index.
Results
A total of 375,560 patients with NVAF were identified (67,017 had an admitting/primary AF diagnosis, and 308,543 had a secondary AF diagnosis; ). The mean age of the study population was 73.8 years and 46.3% were female. The mean age of the cohort with a primary AF diagnosis was 67.9 years and 45.6% were female, while 46.5% of patients with a secondary AF diagnosis were female and mean age was 75.0 years (). In the sample of patients with a secondary AF diagnosis, ∼60% of patients had a major or extreme degree of severity for the admission diagnosis-related group as defined by 3M’s algorithm (APR-DRG grouper code)Citation21, compared to only 29% of patients with a primary AF diagnosis. Among patients with a secondary AF diagnosis, the three most common primary diagnoses were heart failure (7.4%), septicemia (6.6%), and acute myocardial infarction (6.2%; Appendix 1).
Table 1. Patient demographics and clinical characteristics of NVAF patients.
presents the LOS and the treatment patterns of NVAF patients. The mean LOS for the overall population, the primary AF diagnosis cohort, and the secondary AF diagnosis cohort was 6.8 days, 3.7 days, and 7.5 days, respectively. In addition, the proportion of patients that had an intensive care unit (ICU) stay during their hospitalization was 29.7%, 18.4%, and 32.1% in the overall population, the primary AF diagnosis cohort, and the secondary AF diagnosis cohort, respectively. The corresponding mean days to administration of anticoagulant during the hospitalization were 1.9 days, 1.4 days, and 2.0 days, respectively.
Table 2. Length of stay and treatment characteristics of NVAF patients.
The daily hospitalization costs stratified by department are presented in . In the study population, the mean (SD) daily costs were $2391 ($2227), with costs ranging from $4282 ($6363) to $1959 ($3339) in the first 7 days, the most expensive being the admission day and the least the 6th day. The costs stabilized on the 3rd day of the hospitalization (mean (SD) = $2103 [$3261]) since the mean (SD) costs of the 4th day ($1993 [$3397]) were not statistically different than those of the 3rd day (standardized difference = 3.3%). Among the stratified costs, the room and board costs were the biggest cost category, accounting for 27–49% of the total costs, depending on the day ( and ).
Figure 2. Daily hospitalization costs of all NVAF patients stratified by cost categories during the first 14 days. NVAF, non-valvular atrial fibrillation.
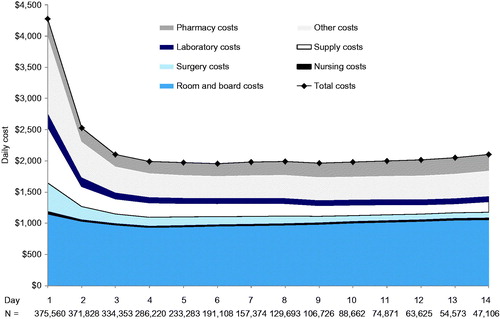
Table 3. Daily hospitalization costs of NVAF patients.
Patients with a primary AF diagnosis had mean daily costs of $2101 ($2398), ranging from $3332 ($5242) to $1476 ($2639) in the first 7 days, the most expensive being the admission day and the least the 4th day. Patients with a secondary AF diagnosis had mean daily costs of $2455 ($2183), ranging from $4489 ($6563) to $1998 ($3375) in the first 7 days, the most expensive being the admission day and the least the 6th day. In both stratified analyses, the costs stabilized on the 3rd day (mean costs on day 3: primary AF diagnosis cohort = $1505; secondary AF diagnosis cohort = $2208). The mean (SD) total hospitalization costs among all patients were $18,631 ($27,096). For the sub-set analysis of patients in the primary AF diagnosis cohort, the mean hospitalization costs were $9273 ($12,116), while in the secondary AF diagnosis cohort they were $20,664 ($28,959) ().
presents daily pharmacy costs stratified by the top five types of medication used during the hospital stay. The total pharmacy costs were relatively stable throughout the hospitalization, and the most costly medication used was an injectable anticoagulant (). Daily pharmacy costs were higher for the first 3 days in the cohort of patients with a secondary AF diagnosis, at $287, $238, and $205, while patients with a primary AF diagnosis incurred daily pharmacy costs of $160, $144, and $126 for the same 3 days. The proportion of pharmacy costs related to anticoagulants was bigger in the cohort of patients with a primary AF diagnosis than that in the cohort of patients with a secondary AF diagnosis (proportion of the overall hospitalization: 30% vs 13%; ).
Table 4. Daily hospitalization pharmacy costs of NVAF patients.
Discussion
Based on real-world hospital-based Premier data, this large retrospective study was conducted to quantify the progression of daily hospitalization costs among NVAF patients that used anticoagulant therapy during their hospital stay. During the 5-year period, a total of 375,560 NVAF patients were studied. In the overall population and the sub-sets of patients with a primary and a secondary AF diagnosis, the daily costs of hospitalization decreased during the first 2 days and tended to stabilize on the 3rd day at $2103, $1505, and $2208, respectively. In addition, pharmacy costs remained stable throughout the hospital stay for the overall population and both cohorts.
To our knowledge, this study is the first to quantify the progression of daily costs among NVAF patients; however, some studies have reported the total costs of NVAF hospitalization for patients treated with warfarin. For example, Song et al.Citation22 reported total hospitalization costs of $6160 for primary AF diagnosis patients and $13,194 for secondary AF patients. They also reported a longer LOS for hospitalized patients with a secondary AF diagnosis compared to those with a primary AF diagnosis of 3.01 days (mean LOS primary AF diagnosis = 3.80 days, secondary AF diagnosis = 6.81 days). These results are similar to those found in our study and present an important distinction between patients with a primary vs secondary AF diagnosis. Patients with a secondary AF diagnosis were admitted to the hospital with other major conditions (i.e., heart failure, septicemia, acute myocardial infarction; Appendix 1) and compared to patients with a primary AF diagnosis; which seem to be two fundamentally different populations.
Recently, Fonseca et al.Citation23 studied a sample of NVAF patients treated with dabigatran vs warfarin therapy and reported a shorter LOS of 1.1 days for dabigatran users compared to warfarin users in the overall population. For the same population, the authors reported hospitalization costs of $18,362 for dabigatran users and $22,602 for warfarin users (cost difference = $4240, p < 0.01). More recently, Laliberté et al.Citation15 used a sample of NVAF patients from the Premier database who were administered rivaroxaban vs warfarin during a hospitalization and reported that rivaroxaban users had a shorter hospital LOS of 0.81 days compared to warfarin users (LOS rivaroxaban = 4.46 days; warfarin = 5.27 days; p < 0.001). Using data from the apixaban trial, Cowper et al.Citation16 also presented a shorter LOS for patients treated with apixaban than patients treated with warfarin (LOS difference = 0.11 days; p = 0.05). Overall, recent studies of NOAC agents showed that patients treated with these new agents incurred shorter LOS than patients treated with the standard of care. A study conducted by Arowolaju and Gillum.Citation24 using the US National Hospital Discharge Survey for discharges estimated a total of 2,643,000 hospital diagnoses of AF in the US in 2009, of which 467,000 and 2,176,000 were primary and secondary diagnosis of AF, respectively. Based on the reduction of ∼1 day in LOS that has been estimated in the literature for NOAC compared to warfarin usersCitation14,Citation15,Citation23,Citation25, and the findings of the current study using the mean costs on Days 5–7 (possibly where a hospitalization day that may be prevented) of ∼$1550 for primary AF and $2000 for secondary AF, the use of NOAC agents may generate substantial savings (over $700 million and $4 billion per year for primary and secondary diagnosed hospitalizations, respectively).
Our results showed that any decrease of LOS in NVAF patients can have an impact on costs in any department or cost category (e.g., room and board, nursing, supply, surgery, laboratory, pharmacy) occurring during a hospitalization. Furthermore, pharmacy costs excluding anticoagulant agents represented a large proportion of the total pharmacy costs in our study, and any decrease in LOS would also impact these pharmacy costs, decreasing the burden of other medications used by NVAF patients during their hospitalization. Although new NOACs have higher acquisition costs than warfarin or other VKA treatments, the costs of the new agents may be offset by their impact of a shorter LOS. New treatment protocols or alternatives for anticoagulation such as NOACs are, thus, of great interest to potentially reduce the cost burden of AF. Moreover, since NOAC agents have advantages compared to warfarin, such rapid onset of action and more predictable pharmacokinetics, and no need for INR monitoring, their use may possibly shift the treatment of patients with AF toward the outpatient setting and, thus, further reduce the costs burden of AFCitation13,Citation26.
This study was subject to limitations associated with data constraints. First, in spite of information accuracy and completeness required by administrative databases for payment purposes, billing inaccuracies and missing data may still occur. Second, the observational design was susceptible to various biases such as information or classification bias (e.g., identification of false-positive AF events). Despite these limitations, the current research has several advantages including reliance on 5 years of real-world utilization data, a novel approach of evaluating atrial fibrillation costs (i.e., daily), and a considerable sample size from a large database.
Conclusion
This large retrospective study of over 375,000 hospitalized NVAF patients that used anticoagulant therapy based on real-world data indicates that hospitalization costs were higher for the first 2 days of hospitalization and tended to stabilize after. Results presented differences in LOS and costs between primary and secondary AF diagnosis patients, and suggested that change in disease management strategies, treatments, or protocols that could decrease or increase the hospital LOS may impact healthcare department costs.
| Abbreviations: | ||
| AF | = | atrial fibrillation |
| NVAF | = | non-valvular atrial fibrillation |
| VKA | = | vitamin-K antagonist |
| LOS | = | length of stay |
| US | = | United States |
| HIPAA | = | health insurance portability and accountability act |
| ICD-9-CM | = | international classification of disease, ninth revision, clinical modification |
| SD | = | standard deviation |
| ICU | = | intensive care unit. |
Transparency
Declaration of funding
This research was funded by Janssen Scientific Affairs, LLC, Raritan, NJ.
Declaration of financial/other relationship
DP, FL, GG, and PL are employees of Analysis Group, Inc., a consulting company that has received research grants from Janssen Scientific Affairs. BKB is an employee of Janssen Scientific Affairs and SHM and JL were employees of Janssen Scientific Affairs at the time the study was conducted. JFD is a consultant for Janssen Scientific Affairs. EAN is a consultant and received research funding from Janssen Scientific Affairs.
References
- Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the AnTicoagulation and Risk Factors in Atrial Fibrillation (ATRIA) Study. JAMA 2001;285:2370-5
- Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation 2006;114:119-25
- Naccarelli GV, Varker H, Lin J, et al. Increasing prevalence of atrial fibrillation and flutter in the United States. Am J Cardiol 2009;104:1534-9
- Ball J, Carrington MJ, McMurray JJ V, et al. Atrial fibrillation: profile and burden of an evolving epidemic in the 21st century. Int J Cardiol 2013;167:1807-24
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation 2013;127:e6-e245
- Wu EQ, Birnbaum HG, Mareva M, et al. Economic burden and co-morbidities of atrial fibrillation in a privately insured population. Curr Med Res Opin 2005;21:1693-9
- Coyne KS, Paramore C, Grandy S, et al. Assessing the direct costs of treating nonvalvular atrial fibrillation in the United States. Value health j Int Soc Pharmacoecon Outcomes Res 2006;9:348-56
- Kim MH, Johnston SS, Chu B-C, et al. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circulation. Cardiovasc Qual Outcomes 2011;4:313-20
- Mantha S, Cabral K, Ansell J. New avenues for anticoagulation in atrial fibrillation. Clin Pharmacol Therapeut 2013;93:68-77
- U.S. Food and Drug Administration. FDA approves Pradaxa to prevent stroke in people with atrial fibrillation. Silver Spring, MD, 2010. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm230241.htm. Accessed January 2014.
- U.S. Food and Drug Administration. FDA approves Xarelto to prevent stroke in people with common type of abnormal heart rhythm. Silver Spring, MD, 2011. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm278646.htm. Accessed January 2014.
- U.S. Food and Drug Administration. FDA approves Eliquis to reduce the risk of stroke, blood clots in patients with non-valvular atrial fibrillation. Silver Spring, MD, 2012. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm333634.htm. Accessed January 2014.
- Hankey GJ, Eikelboom JW. Novel oral anticoagulants for atrial fibrillation. Curr Atheroscler Rep 2013;15:344
- Fonseca E, Walker DR, Hill J, et al. Abstract 282: Dabigatran Etexilate is associated with shorter hospital length of stay compared to Warfarin in patients with nonvalvular atrial fibrillation. Circ Cardiovasc Qual Outcomes 2012;5:A282
- Laliberté F, Pilon D, Raut MK, et al. Hospital length of stay: is rivaroxaban associated with shorter inpatient stay compared to warfarin among patients with non-valvular atrial fibrillation? Curr Med Res Opin 2014;30:645-53
- Cowper PA, Pan W, Anstrom K, et al. Apixaban reduces hospitalization in patients with atrial fibrillation: an analysis of the effect of Apixaban therapy on resource use in the Apixaban for reduction in stroke and other thromboembolic events in atrial fibrillation trial. J Am Coll Cardiol 2013;61:E1576
- Dasta JF, Pilon D, Mody SH, et al. Daily hospitalization costs in patients with deep vein thrombosis or pulmonary embolism treated with anticoagulant therapy. Thromb Res 2015;135:303-10
- Cohen J. Statistical power analysis for the behavioral sciences. New York, NY: Toronto Academic Press, Inc, 1977
- Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol 2001;54:387-98
- Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput 2009;38:1228-34
- 3M. M Health Information Systems - US. APR DRG Software. Salt Lake City, UT: 3M, 2013. http://solutions.3m.com/wps/portal/3M/en_US/Health-Information-Systems/HIS/Products-and-Services/Products-List-A-Z/APR-DRG-Software/. Accessed January 2014.
- Song X, Sander SD, Johnson BH, et al. Impact of atrial fibrillation and oral anticoagulation on hospital costs and length of stay. AJHP Off J Am Soc Health-Syst Pharm. 2012;69:329-38
- Fonseca E, Walker DR, Hess GP. Abstract 258: Dabigatran Etexilate is associated with shorter hospital length of stay and lower hospital costs compared to Warfarin in treatment-naive, newly-diagnosed nonvalvular atrial fibrillation patients. Circulation: Cardiovasc Qual Outcomes 2013;6:A258
- Arowolaju A, Gillum RF. A new decline in hospitalization with atrial fibrillation among the elderly. Am J Med 2013;126:455-7
- Farr A, Jing Y, Johnston S, et al. Abstract 16698: comparison of hospital length of stay between hospitalized non-valvular atrial fibrillation patients treated with either Apixaban or Warfarin. Circulation 2014;130(2 Suppl):A16698
- Wong CX, Lau DH, Sanders P. Atrial fibrillation epidemic and hospitalizations how to turn the rising tide? Circulation 2014;129:2361-63
Appendix 1