Abstract
Current estimates indicate that 50% of the population experience at least one mental disorder in their lifetime and that at least 25% have suffered a mental disorder in the past year. recognition, diagnosis, treatment, and referral depend overwhelmingly on general practitioners, at least one third of whose consultations have a direct and explicit psychological component. Yet despite this intensive familiarization with the presentation of mental pathology, and the appropriateness of the primary care setting to its management, even the most recent surveys indicate that performance is best described by the rule of diminishing halves: only half the patients with a thresh-old disorder are recognized; only half of those recognized are treated; and only half of those treated are effectively treated. There is no single solution to this problem, only multiple solutions, which must be aimed, consistently and simultaneously, at the patient, practitioner, practice, and research levels.
Actualmente se estima que el 50% de la población experimenta al menos un trastorno mental a lo largo de la vida y que al menos el 25% ha sufrido algún trastorno mental durante el último año. El reconocimiento, el diagnóstico, el tratamiento y la derivación al especialista dependen de manera casi exclusiva de los médicos generales, cuyas consultas en al menos un tercio de los casos tienen un componente psicológico directo y explicito. Sin embargo, a pesar de una mayor familiarización con la forma de presentar la patologia mental y de las mejoras realizadas en su manejo, los resultados de las investigaciones más recientes muestran que en el mejor de los casos los resultados se ajustan a lo que se puede definir como “la regla de las mitades decrecientes”: es decir, del total de pacientes con trastornos clinicamente relevante, sólo se registran la mitad, de estos sólo la mitad reciben tratamiento, y de estos últimos sólo la mitad son tratados de una forma eficaz. Para este problema no existe una única solución, sino que hay varias respuestas que beben orientarse constistente y simultáneamente para el paciente, el médico, la práctica clinica y la investigación.
On estime actuellement que 50% de la population souffre d'au moins un trouble mental dans sa vie entière et qu'au moins 25% en a souffert au cours de l'année écoulée. La reconnaissance, le diagnostic, le traitement et l'orientation vers le spécialiste dépendent de façon quasi exclusive des médecins généralistes, au moins un tiers de leurs consultations ayant une composante psychologique directe et explicite. Néamoins, en dépit de cette familiarisation intensive avec la maladie mentale et la bonne adéquation du cadre des soins de première intention à la prise en charge de ces troubles, même les enquêtes les plus récentes montrent qu'en ce qui concerne les résultats, la meilleure description correspond à la règle des moitiés dégressives: seulement la moitié des patients cliniquement décelables est identifiée; seulement la moitié de ces derniers est traitée et seulement la moitié des patients traités l'est de façon efficace. Ce problème appelle non pas une solution unique mais plusieurs réponses qui doivent s'adresser simultanément et logiquement au patient, au médecin, à la pratique médicale et à la recherche.
In most health care systems, primary care doctors are the cornerstone of recognition, diagnosis, treatment, and specialist referral for all types of disorders, whether they are somatic, psychological, or both. The past two decades have witnessed a further emphasis of this role, particularly with regard to the treatment of mental disorders in primary care. Several reasons account for this. First, mental disorders are extremely prevalent In the community, and much more than previously thought. Current epidemiological findings suggest that almost 50% of the population will experience at least one mental disorder In their lifetime, and at least 25% have suffered from a mental disorder during the past 12 months.Citation1-Citation3 Second, International epidemiological evidence suggests that, of all the people with mental disorder who receive treatment, a large proportion obtain at least minimal Intervention through their primary care doctor.Citation4,Citation5 Third, the continuing trend of reducing psychiatric hospital beds contributes to a larger burden of psychiatric patients in outpatient and, particularly, primary care settings. Finally, the rapidly accumulating knowledge in clinical neuroscience and clinical psychology has resulted in various new treatment options for a wide range of neuropsychiatrie conditions and disorders, and many of these can be applied in primary care.
In most systems, the majority of people report at least one primary care visit per year, thereby maintaining a stable and enduring relationship. On this basis, the general practitioner (GP) may develop a deeper understanding of individual vulnerability for certain diseases, illness behavior, the waxing and waning of disorders, the development of somatic and mental comorbidities, and the ability to overcome the direct and indirect effects of diseases. GPs also frequently have a more intimate knowledge of the psychosocial context in which patients' distress and illnesses occur (ie, interpersonal and family crises, occupational and employment problems, and social, environmental, and financial difficulties). Finally, a visit to a GP even for mental health reasons does not carry the same amount of stigma as a visit to a mental health specialist. Thus, the barriers to help-seeking and acceptance of treatment are considerably reduced in primary care.
Mental disorders in primary care: poorly studied and poorly understood
In light of this situation, it is paradoxical that mental disorders in primary care - and the way they are managed - remain poorly studied. With a few notable exceptions (see below), this statement applies to both the size of the problem (ie, frequency and type of mental disorders seen in primary care) and the more complex set of questions regarding the quality of care (accuracy of recognition, diagnosis, and management). Thus, the extent to which these functions are fulfilled in primary care remains largely unclear. Another question concerns the domains of mental disorders and specific treatments in which primary care providers are at a disadvantage in terms of qualifications and provision of state of the art therapy.
This lack of data is particularly evident from a broader international perspective. Despite the considerable body of published results on some of these issues, the findings are mostly confined to certain disorders and to selected areas and countries (UK and USA). Thus, they cannot be generalized to the ensemble of countries, health care systems, and disorders. Between countries, especially within Europe, there are tremendous differences in the way primary care services operate. For example, in some countries (eg, USA or Germany), patients have direct access to mental health specialists, whereas in others they require prior referral by a GP.
As part of the International Consortium of Psychiatric Epidemiology (ICPE) program, Bijl et alCitation5 recently highlighted some of these differences in a five country comparison to examine the proportion of people with mental disorders who received treatment in the past 12 months. Ascertained treatment rates varied from a low of 7% in Canada to a high of 17.3% in Chile, with the US rate being 10.9%. Respondents were also asked about the sector of treatment, distinguishing the general medical sector (eg, GP), the specialty sector (psychiatrist or psychologist), and other human services (self-help groups, social services, counseling centers, etc). The distribution by sector varied significantly across countries. The countries in which the majority of patients were seen in the general medical sector were Chile (80.3%), the Netherlands (74.6%), and Canada (65.7%), compared with the USA (43%) and Germany (36.6%). Tremendous national differences are also found with regard to GPs' workload. Whereas Scandinavian doctors rarely see more than 20 patients a day, German doctors usually have 70 or more daily patient contacts. Clearly, it is hard to see how quality measures in a country with 20 patients a day can be compared with countries with up to 100 patients.
With these caveats in mind, this paper will review the patchwork of available findings for mental disorders in an attempt to identify past research achievements and deficits in currently available data. After a few remarks on general diagnostic problems, this review will focus on the most prevalent mental disorders (depression, anxiety, and eating and substance disorders) for which at least one major study is available.
Symptoms and diagnosis of mental disorders
The expression of mental health problems, emotional distress, and even clear cut mental disorders vary widely in terms of presenting problems, severity, complexity, associated impairment, duration, and risks. In most cases, it is not possible to simply equate a diagnosis with a need for immediate intervention. The GP may face even greater problems regarding the relationship between specific disorders and the indication of specific treatments, due to the high degree of comorbidity typically found for mental disorders.Citation6
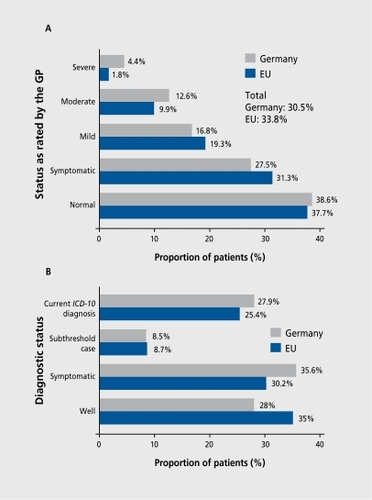
As evidenced by an international WHO study,Citation7 about one third of GP consultations have a direct and explicit psychological component, in terms of full-blown depressive syndrome, anxiety, or somatoform disorder ( .)Citation8,Citation9 European GPs estimate that more than 30% of their patients have a clinically relevant mental disorder, at least to a moderate degree. However, this proportion may be considerably higher if subthreshold conditions or clinically significant psychological problems are considered, adding an additional 30%. Such high numbers are also found when a standardized diagnostic interview is applied. . shows that, according to Diagnostic and Statistical Manual of Mental Disorders, Third Edition Revised (DSM-III-R)Citation10 criteria, the total prevalence of any threshold disorder is 25% to 28%. If subthreshold disorders, which fall short of just one criterion for a full diagnosis, are considered, another 8% to 9% can be added.
This high frequency of clinically significant mental health syndromes (with a total prevalence of over 50%) raises the question of what constitutes a case requiring professional treatment in primary care. For a better understanding of recognition and treatment issues in primary care, it is essential to consider first the patients' presenting complaints and subjective suffering (illness), and then the usual progression from these to the establishment of a diagnosis (disease) of a specific mental disorder and to treatment decisions in medical settings.
To illustrate, when patients complain of persistent sleep problems, they may receive, according to their doctor's diagnostic workup, the diagnosis of a sleep disorder (insomnia) and a prescription for hypnotics. Alternatively, their doctor may notice that the sleep problems have occurred together with a wide range of persistent depressive symptoms over the past 3 weeks, which justifies the diagnosis of major depression (MD), prompting some counseling and a prescription for antidepressants or even referral for psychotherapy. Some, but not all, of the considerable problems involved in the definition and diagnostic classification of physical illnesses may be aggravated in mental illness and disorders. Sleep complaints could be a sign of a disorder like insomnia or depression, but exactly the same symptoms could also be present in transient unhappiness or distress. Thus, the borderline between symptoms due to unhappiness or distress, on the one hand, and symptoms due to threshold mental disorders, on the other, is often indistinguishable.
This problem seems to be aggravated by shifts of paradigms in diagnostic classification for mental disorders. In contrast with previous scientifically unproven nosological classifications of mental disorders, which were of poor reliability and validity, the current versions of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV)Citation11 and International Statistical Classification of Diseases, 10th Revision (ICD-10)Citation9 have now adopted a largely descriptive approach with operationalized criteria for disorders. This shift in paradigm has resulted in a continually increasing number of diagnostic classes from 59 disorders early in the 20th century to 347 major classes in DSM-IV.Citation11 Does this increasing sophistication truly reflect scientific progress (driven by valid data) or is it simply an epidemic of artificial medicalization? Moreover, is it helpful for sufferers and GPs, or only for specialists? Health care professionals in general, and GPs in particular, must constantly reexamine at what point it becomes helpful to the patient to classify their mental distress as mental illnessCitation12 because this decision also implies the danger of stigmatization or suboptimal treatment allocation. Despite the undisputable progress and the consequent increased reliability and validity of psychiatric diagnoses, these problems remain unresolved and have given rise to questionable heuristics aimed at simplifying hétérogèneity (ie, serious versus nonserious, or minor versus major mental disorder).
Prevalence, recognition, and management of mental disorders in primary care
Before presenting some more recent findings on selected disorders, it should be noted that only one major international study has directly addressed the question of prevalence, recognition, and treatment of a wide range of mental disorders in primary care. This benchmark study is the WHO study Psychological Disorders in Primary Care, and was conducted in 18 countries in the eighties.Citation7 Although only a small proportion of mental disorders were covered, the total point prevalence of threshold ICD-10 diagnoses across centers was 24%, with some variation between countries (from 20% in Shanghai to 50% in Santiago de Chile). Major depressive disorders (10%) and generalized anxiety disorders (GADs, 8%) were the most frequent diagnoses, followed by neurasthenia (5%), alcohol dependence (3%), and somatization disorder (3%) (Table I), This study focused on threshold cross-sectional diagnoses and excluded partially remitted or subthreshold disorders; the estimates can thus be regarded as conservative.
In terms of recognition and treatment, the study revealed that GPs recognized only 49% of the mental disorders ascertained by the study instrument. Moreover, only about half of all cases recognized received some specific intervention, and the majority of these treatments were not considered to be state of the art first-line treatments. Another puzzling result was that, in addition to the 25% rate of threshold disorders, the treating physicians also labeled an additional 11% of patients as having a mental disorder that was not ascertained by the study instrument. It remains unclear whether a proportion of these patients were incorrectly diagnosed, or whether these findings reflect partially remitted mental disorders or an episode that did not yet meet current research criteria, or indeed whether the patients or diagnoses were not completely covered by the research study.
The study also highlighted a tremendous variation between centers and between diagnoses in terms of prevalence, recognition, and treatment. This variation may indicate considerable differences in provider models of primary care around the world, cultural distinctions, and the fact that well defined disorders (like depression) are better recognized, diagnosed, and treated than rarer and ill-defined conditions.Citation13
Depressive disorders
Studies in the 1980s and early 1990s conducted in primary care in various countries with fairly convergent methods and designsCitation14 confirmed that depression is indeed a quite frequent problem in primary care. The point prevalence for depressive disorders has been estimated with some variation to be about 10% of all primary care attendees.Citation7,Citation15-Citation19 There is also fairly consistent agreement that, among patients with clinically significant depression, over 50% were not recognized by the treating primary care physician.Citation7,Citation20-Citation22 Moreover, among those recognized, only a fraction appear to receive treatments that could be described as adequate according to expert guidelines.Citation18,Citation22-Citation27 Remarkably, these findings apply even to most recent studies, even after many years of action to improve GPs' ability to recognize the presence of depressive disorder in patients.Citation19
Out of all the mental disorders, depression has certainly received the greatest attention, in terms of both indirect evidence from community studies and direct evidence by investigations in primary care settings. A comprehensive community survey, the ICPE (which reanalyzed data from the general population in 6 countriesCitation2), recently examined the general population who had suffered a depressive disorder in the past 12 months: only about a fifth in Canada (22%) and the USA (22%), and slightly more in the Netherlands (32%) and Germany (29%), actually received any type of treatment. The key role of primary care was strongly confirmed in this study, in that the vast majority of patients in all countries were cared for exclusively in the primary health care sector. Few received treatment from mental health specialists. It is noteworthy that intervention or treatment in this analysis was merely defined as any treatment contact, irrespective of appropriateness in terms of type, dose, and duration of treatment. A further disturbing finding from community studies is that, for the majority of patients, it takes many years from the first onset of their disorder to the prescription of appropriate treatment.Citation28 The recent German study, Depression 2000, was based on a national representative sample of 412 GPs and had a three stage designCitation29 in 15 081 consecutive primary care attendees. This study revealed that of the 11% of patients meeting diagnostic criteria for DSM-IV episode of MD in this study, two thirds were recognized by the primary care practitioner as having a clinically severe mental health problem, but only 39% were correctly diagnosed as definitely having depression, and an additional 16% as having a probable depression. Recognition rates were especially poor in males (correct identification rate 27%) and females (33.2%) aged less than 40 years.Citation30
If the treatments chosen worked equally well in all types of mental disorders, then the poor recognition of depression would not be an important issue. However, it is noteworthy that the unsatisfactory recognition pattern and the diagnostic imprecision had remarkable effects on the doctors' subsequent intervention behavior: more than 40% of all patients meeting DSM-IV criteria for MD did not receive any treatment or significant intervention of any kind! MD cases correctly recognized as at least “probable depression” by the GP had the greatest likelihood (65%) of receiving first-line antidepressants (37%), psychotherapy (9%), or being referred to a mental health specialist (22%). Despite no significant differences in symptomatology, MD cases recognized as simply “having a mental health problem” without a specific depression diagnosis received first-line treatments considerably less frequently (42%), whereas cases without any rating as a clinically significant problem went largely untreated. They were also more likely to be treated with a sedative or hypnotic, but less likely to receive a neuroleptic or a herbal medication. With regard to the type of antidepressant prescribed, modern antidepressants, such as noradrenergic and specific serotonergic antidepressants or selective serotonin reuptake inhibitors (SSRIs), were more likely to be prescribed for patients diagnosed with depression than tricyclic antidepressants. These findings were by and large confirmed in a more recent primary care study using the identical design in ScandinaviaCitation31 (Munk Jurgensen, personal communication).
In accordance with previous research, the Depression 2000 studyCitation29 showed that the correct recognition of depression and the likelihood of receiving adequate treatment were associated with a similar set of predictors on the patient's side: older age, prior depression or treatment history, depressed mood as the primary reason for consulting the doctor, and suicidal ideation. Current severity also had an effect (odds ratio [OR] 1.2), although not as great as that associated with the other factors. On the doctor's side, surprisingly few predictors were identified: doctors who had attended a high number of courses on depression in the previous 2 years had a greater probability of correctly recognizing a patient with depression (OR 2.1); doctors with > 20 years of experience (ie, the older doctors in the sample) had a considerable lower recognition rate (OR 0.5). Taking their attitudes toward depression into account and their theoretical background, the authors speculate that older doctors tend to rely heavily on the traditional nosologleal classification systems, which differentiate between endogenous versus neurotic and reactive depression. This subgroup of older - and seemingly more experienced- doctors were particularly poor at recognizing depression in young people.
The studyCitation29,Citation30 concluded that, despite numerous attempts to improve doctors' recognition rates and prescription of appropriate treatment, only modest improvements have been made. Moreover, although GPs manage the typical severe, melancholic patient relatively well, marked deficits were evident for young patients, new cases of incident depression, and cases with comorbidity with other mental disorders. The major barriers for improved recognition and treatment in this study were the time burden of the treating physician and failure to adopt the current descriptive way of diagnosing depression, as opposed to the traditional nosological approach.
Anxiety disorders
In contrast with the large number of studies in depression, anxiety disorders remain a relatively neglected topic of systematic primary care research. This is surprising considering (i) that about a quarter of the general population is or has been affected at some point in their lives by an anxiety disorder; (ii) the chronic nature of anxiety disorders; (iii) the early onset of most forms of anxiety disorders; and (iv) the high probability that primary anxiety might be a powerful risk factor for secondary depression and substance abuse. Further, there is substantial evidenceCitation32 that psychoeducative efforts and brief interventions might be very effective in uncomplicated cases and in the early stages of anxiety disorders, even if applied in primary care. Obviously, the misconception of anxiety disorders as belonging to the less severe morbidity spectrum, with no explicit need for immediate intervention, is the cause of this neglect.
The available evidence is largely limited to two anxiety disorders: panic disorder (PD) and GAD, which are assumed to be the most severe and chronic forms. The available evidence generally suggests a somewhat worse picture than for depression. Of all anxiety disorders, less than 50% are recognized and even fewer are specifically diagnosed.
Panic disorder
According to Spitzer et al,Citation33 PDs occur in about 4% of patients in US primary care, although other studies suggest that this is an upper bound estimate (ie, the true value might be lower).Citation7 PD is frequently associated with agoraphobia and differs from most phobic disorders in terms of acute severity, extensive use of medical services, high costs, multiple unexplained medical illnesses and therefore increased rates of laboratory testing, and as much impairment and disability as other severe medical illnesses. Similar to depression, < 50% of cases are recognized and few receive adequate diagnosis or treatment in the form of antidepressant drugs, cognitive behavior treatment, or referral to specialists.Citation33
Katon et alCitation34 were unable to show that educational campaigns and treatment guidelines have any sustained and significant effect on improved recognition. However, they recently demonstratedCitation34 that collaborative care interventions in US primary care, consisting of f ollow up with the psychiatrist who made the initial SSRI prescription and psychoeducation, can result in remarkable improvements in terms of symptom reduction. Although direct treatment costs were substantially higher with this approach, the overall costs due to reduction in indirect costs were superior to usual treatment. It is difficult to generalize these findings to other regions and countries, but it nevertheless ranks among the few promising alternative approaches to be pursued in the future for this and other disorders.
Generalized anxiety disorder
GAD is a severe and chronic anxiety disorder, for which effective drug and psychological treatments have recently become available. The lifetime prevalence of GAD in the general population has been estimated to be 5% to 6%,Citation31,Citation35,Citation36 which is more than PD. GAD patients are also frequently described as high health care users, particularly of primary care resources. GAD is a highly disabling condition that results in significant impairments in terms of work productivity, performance of everyday activities, quality of life, and well-being.Citation37,Citation38 This can be equivalent to, or even greater than, those assoelated with other chronic physical or mental disorders.Citation39 While chronic worrying and the physical effects of chronic tension are the principal features of GAD, patients with this condition primarily present to their GP with somatic, pain, or sleeping complaints, rather than anxiety or worry.Citation40 This well known phenomenon of somatization has also been found in many cases with depression and has been held responsible for low recognition of mental disorders in primary care.Citation30,Citation41 The most commonly occurring somatic complaints are insomnia, chest pain, and abdominal pain,Citation13 and patients frequently undergo extensive and costly diagnostic procedures to rule out physical conditions.Citation42 During these investigations, patients often do not receive the treatment that is appropriate for their psychiatric disorder, and may never do so. In addition, an undue financial burden is imposed upon the health services. Another critical issue is the frequent comorbidity with depression, other anxiety disorders, and chronic physical conditions, which complicates the clinical presentation, makes diagnosis more difficult, increases the degree of impairment,Citation43 and worsens the patient's prognosis. In light of the various effective treatment options for GAD that have recently become available, it is important that GAD is diagnosed as early as possible to minimize the potential for the subsequent onset of depression, while improving the patient's quality of life and prognosis, and reducing health care costs. The high point prevalence of 8% of all primary care attendees,Citation7 rendering GAD second only to depression as the most common disorder in primary care,Citation44,Citation45 has made improved recognition and earlier treatment a high priority in recent primary care research (Ballenger et al, personal communication).
In probably the largest primary care study on this issue, the Generalized Anxiety and Depression in Primary Care (GAD P) studyCitation46 recently confirmed the high prevalence of GAD even in its pure form (uncomplicated by depression) and showed that GAD patients are high users of primary care resources.Citation31 For example, it has been reported that gastroenterologists are the specialists seen most often by GAD patients (23 %).Citation47 This contrasts with other disorders such as social anxiety for which the point prevalence is lower in primary care than in the general population.Citation48 In remarkable contrast, the GAD P study revealed that patients with GAD are a great challenge to GPs, as demonstrated by extremely poor recognition and treatment rates. Despite the fact that GPs acknowledged the severity of their GAD patients by assigning some mental disorder in 73% of the patients, only a third were diagnosed correctly and only 10% overall received the current state-of-the-art treatment.Citation31 The predictors for correct diagnosis were similar to those identified for depression; however, poor knowledge about the fact that this diagnosis exists and that specific treatments for this disorder are available played a much greater role than for depression.
Eating disorders
The prevalence of eating disorders in the total population is low, with lifetime estimates of around 1% to 2%; however, the rates among adolescents and young adults are considerably higher (twoto threefold). Despite the low prevalence, the considerable health-related shortand long term consequences and the substantial risk for comorbidity and premature mortality make the GP an important route to specialist care.Citation49 The evidence for increasing rates of bulimia nervosaCitation50 adds further to this need and requires greater attention in the future.
Few systematic studies are available to describe the frequency, recognition, and specific forms of intervention applied in eating disorders in primary care. On the basis of primary care registries with administrative diagnoses for the UK, SchmidtCitation49 estimated that the average GP has about 2 patients with anorexia nervosa and about 18 patients with bulimia nervosa on their list of registered patients. Despite the fact that eating-disordered patients consult their GPs more frequently than control subjects,Citation51 GPs were unaware of the diagnosis in up to 50% of cases discovered by research interview.Citation52,Citation53 These patients presented to their GP with a variety of symptoms, including psychological, gastrointestinal, and gynecological complaints. In many cases, the earlier consultations to the GP had been prompted by complications of the eating disorders, but the diagnosis was missed. Many reasons have been evoked to account for these problems, including the patients' tendency to hide the problem verbally as well as by wearing baggy clothes, social factors (lower socioeconomic status, ethnic minority), and gender (males are not expected to have eating disorders). Some indications were also found for specific communication barriers: female patients do not expect their mostly male doctors to understand their problem or to be sympathetic about it. A survey by the Eating Disorder Association (cited in reference 50) revealed that 43% of 1638 respondents with eating disorders found that their initial consultation with the GP was unhelpful. Other important barriers specifically relate to the problem of the compulsory treatment of severe anorexia nervosa. The few systematic primary care studies available do not lead to any conclusions about how to improve recognition or treatment rates, which seem to be at least as deficient as those for anxiety and depression. There is some evidence that at least early recognition and short motivational interviewing techniques for subsequent specialist treatment are high priority topics for improved primary care in this subgroup of disorders.
Substance abuse disorders
Although there are a considerable number of studies that have highlighted the beneficial effects of improved recognition of alcohol and nicotine disorders by GPs, it should be noted that systematic epidemiological primary care results on prevalence, recognition, and treatment of these conditions are only slowly becoming available. Taking the prevalence obtained from studies in the community, we can estimate that at least a fifth of all primary care patients have some type of substance disorder, most frequently nicotine or alcohol dependence. Although it is hard to conceive how GPs could provide state of theart specialist substance abuse treatment in these patient groups, which are notorious for being particularly challenging, screening, recognition, referral, and motivational enhancement techniques are usually seen as a standard requirement in primary care.
Theoretically, GPs are in a unique position to at least intervene in legal substance abuse problems. They avoid the stigma attached to specialist addiction units and have the advantage of comprehensively overlooking the long-term development and somatic and mental risks. In light of these advantages, numerous short brief intervention packages and programs have been launched and considerable effectiveness has been demonstrated in controlled trials. The focus of most of these programs (for example, the United Kingdom Alcohol Treatment Trial [UK ATT], the National Treatment Outcome Research Study [NTORS], and the Smoking and Nicotine Awareness and Treatment Study [SNICAS]) is mostly on motivational techniques (such as motivational enhancement therapy [MET]) for nicotine and alcohol abusers, as well as behavioral treatments sometimes supplemented by drugs.
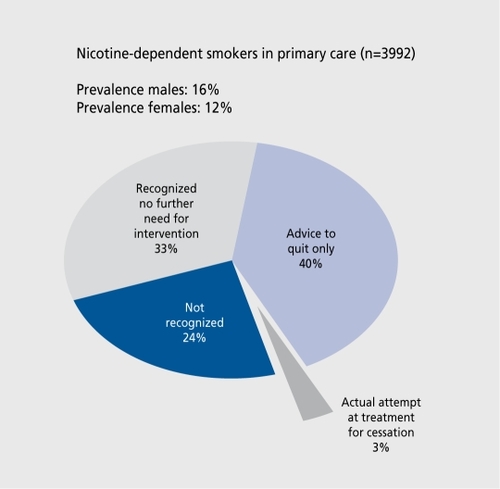
The outcomes of such endeavors are frequently disappointing. The recent SNICAS trialCitation54 in Germany revealed that 16% of consecutive male and 12% of female primary care attendees have a current nicotine dependence ( .) Although they were aware of the aim of the study, the GP recognized only 76% of these patients as smokers, discussed the need for stopping with only 23%, and actually made an attempt to provide help in only 13%.
A further disappointing finding refers to patients' lack of motivation to stop immediately and register for a systematic state-of-the-art smoking cessation program and GPs' apparent inability to perform appropriate motivational techniques. Thus, >1% of smokers actually receive some intervention. These findings clearly indicate that substance abuse treatment in primary care remains far from being a realistic option in routine care.
Discussion
The importance of the problem in mental disorders
Clinical epidemiological studies are providing an increasingly sharper and fairly convergent picture about the importance of mental disorders in society, as well as in primary care. Community studies indicate that mental disorders affect at least 50% of the general population at least once in their lifetime, and generally indicate that about 20% of the population is acutely affected by at least one mental disorder at any point in time. In accord with these prevalence estimates, it is not surprising that the point prevalence among unselected primary care attendees is even higher. Since there are no studies in the literature that have estimated and described a fuller range of all existing mental disorders and their patterns of comorbidity, it is impossible to state at this point what proportion of patients in primary care are suffering from at least one mental disorder. It should also be noted that estimates based on administrative records (case registries) are not informative due to the marked deficiencies of GPs in assigning appropriate and sensitive diagnoses.
Almost all the studies examined one or few selected groups of disorders, most frequently depressive disorders, some types of anxiety disorders, and considerably less frequently somatoform, addictive, and other forms of specific disorders. However, since point estimates for depression and anxiety disorders alone are well above 10%, and on the basis of community surveys, well established patterns of comorbidity, and crude estimates from studies that used diagnostically unspecific caseness questionnaires and rating scales, we can speculate that the overall prevalence of any mental disorder is about 30%. This estimate should be regarded as conservative, because only anxiety, depressive, substance abuse, somatoform, and sleep disorders are taken into account. The broad variation between currently available estimates signals that there is need for further descriptive epidemiological studies. In order to advance our general understanding and assist in the planning of improved care in primary care settings, such descriptive studies should ideally be multinational to reflect cultural and regional differences in help-seeking and system characteristics. They need to take into account: (i) a fuller range of mental disorders than previous studies; (il) a greater detail in describing patterns of comorbidity, both within the spectrum of mental disorders as well as associations with somatic disorders; (iii) measures of severity and pattern, as well as disability; and (iv) some assessment of met and unmet needs for intervention from patients' and doctors' perspectives. We know that mental disorders - like somatic disorders (eg, diabetes, hypertension, retinopathy, and cardiovascular disease55)- are usually comorbid with each other, and that these patterns of comorbidity have dramatic effects on treatment, prognosis, course, and outcome. Diagnostically comprehensive studies are therefore of high priority. The fact that the establishment of mental disorders alone cannot always be equated simply with the need for a specific treatment, the additional coverage of severity, disability, and subjective need for care measures is another core element of improved further studies. Undoubtedly, there might still be some need for studying previously neglected single disorders, especially those for which effective treatment has been established. However, given the time burden of GPs and the numbers of patients with mental disorders, the search for clinically meaningful typologies of patients according to their profile of mental disorders might be the most important target for the future. This is particularly true if we consider that it is unlikely that simplified classifications of mental disorders for use in primary care will become available in the immediate future.
Recognition
If unselected patients are diagnosed independently, using appropriate diagnostic instruments for a given mental disorder, almost all studies- irrespective of the type of diagnosis considered- come to the same conelusion: mental disorders are largely underrecognized in primary care. GPs fail to recognize mental disorders, particularly when the task is to make a specific diagnosis, whereas the more unspecific task of determining whether a given patient has at least some form of mental disorder (“mental health caseness”) seems to be somehow better. Although improvement in diagnosis has been the target of countless campaigns over the past two decades on all levels (patients, doctors, and the public), for example, in depressive disorders, improved rates of caseness and diagnostic recognition are rare or at best quite moderate. The upper limit of the correct recognition of depressive disorders is at most somewhere between 50% and 70%, if threshold major depressive disorders or nicotine dependence are considered. For diagnoses that have received less attention, such as GAD, eating disorders, substance abuse disorders, and somatoform disorders, recognition rates are usually in the range of 30% to 50%. Crude comparisons over the past two decades in regions with campaigns to improve recognition have revealed some, albeit moderate, effect. However, some studies have also pointed out that using recognition rates as a measure of the quality of doctors' diagnostic decisions might be misleading and suggested that it is inappropriate to assume that patients will have a better outcome if they are diagnosed and treated. As noted and discussed recently by GoldbergCitation56 and Hôfler and Wittchen,Citation57 higher recognition rates might occur at the expense of doctors' oversensitivity and increased willingness to diagnose mental disorders at the expense of specificity. Obviously, many patients who clearly fail to meet criteria for depression according to the ICD-10 or the DSM-TV receive a diagnosis of depression by the doctors. The ongoing controversies of lowering the criteria thresholds for MD and/or defining new forms of subthreshold depressive disorders (brief recurrent depression, mixed anxiety/depression, etc) could have added to this problem. However, this tendency toward increased willingness to assign depression diagnoses is not without danger. As noted by Hôfler and Wittchen,Citation57 it remains open, for example, whether established treatments for MD are as effective in these subthreshold manifestations. More disturbing, however, is the fact that, despite doctors' increased willingness to diagnose some form of depression, most patients with clear MD remain undetected and untreated.
This raises two important questions. After considerable efforts at improvement, are the current recognition rates of mental disorders are really poorer than recognition of somatic disorders? Do different factors account for nondetection in mental as opposed to somatic disorders? In the eighties, researchers in hypertension used the rule of halves to describe the fairly consistent finding that only half of all hypertensive patients are recognized, and only half of those correctly recognized receive treatment. This observation has prompted countless clinical and political campaigns and considerable action to improve the quality of care in hypertension. Yet the outcome of 20 years of action in this field has recently been described as disappointing, with no considerable change in primary care.Citation58 Comparing this with depression - a disorder that has seen a similar degree of attention in this time period - suggests that screening, awareness, and recognition studies on depression in primary care world-wide follow the same rule. Even the most recent studies find that only slightly more than 50% of primary care patients with depression are diagnosed correctly by their GP - a finding that resembles that from hypertension research.
The failure of attempts to improve physicians' detection skills has usually been attributed to the fact that most awareness programs - as well as the numerous and heavily campaigned treatment guidelines and programs- have no large and, more importantly, no sustained effect on the primary care physicians' routine behavior. It is not entirely clear why this is the case or to what degree specific diagnostic effects play an essential role. As is the case for hypertension, patients with mental disorders are better recognized when they have a more severe disorder or have been diagnosed or even treated previously, or when they present with core symptoms or clearly associated complications. The core barrier for both mental and somatic disorders is the same: if the patient does not specifically and spontaneously report at least some of those key complaints that give a hint at the diagnosis, the doctor will have few reasons to specifically ask or even screen for this. Some authors have suggested that poor recognition of anxiety and depression is primarily and specifically due to the fact that patients with psychological disorders somatize, ie, they present with common - though misleading- somatic symptoms instead of clearcut mood or anxiety symptoms. Others argued that poor recognition is merely the result of thresholds, meaning that if the depression is severe enough it will be recognized. Both explanations have recently been called into question. The somatization hypotheses do not appear to be specific to mental disorders, because comparable processes also apply to a wide range of somatic disorders (hypertension, cardiac disorders, and diabetes58) not acutely linked to specific patient complaints. The severity or threshold hypothesisCitation56 has been called into question because severity was shown to have no significant effect when one controls for comorbidity and past history in multiple regressions. Thus, there are few indications that poor diagnostic recognition of mental disorders is a unique and specific phenomenon, rather poor diagnostic recognition in primary care seems to be strongly influenced by general factors (see below). Further, it should be noted that there are few reasons to believe that psychiatrists and psychotherapists would generally reveal a considerable better profile of diagnostic recognition, if the same rigid criteria were applied. However, such studies have not yet been conducted with a similar degree of detail in the mental health specialty sector to provide evidence for this claim.
Intervention and treatment
Another question is whether the low recognition rates for mental disorders really matter. An assumption in primary care research on recognition and appropriate treatment is that once patients are recognized correctly their chances of getting appropriate treatment increase, and thus their course and outcome will be more favorable. There is some evidence in depression and anxiety research supporting this.Citation30,Citation34 If, for example, patients are recognized as having “definite” MD, they are at least three times more likely to receive state-of-the-art treatment. Further evidence indicated that if the patient is only recognized as “probable depression” or simply as a “case with a mental disorder,” then doctors' subsequent choice of type and duration of treatment is considerably worse than for patients with a definite depression diagnosis. This clearly signals that diagnostic certainty and precision matters. It may be insufficient- or even dangerous - to simply rely on diagnostically unspecific caseness decisions in treating patients as suggested by Goldberg,Citation56 given the existence of various treatment and management guidelines.
Yet the evidence that improved recognition results in more favorable outcome for the patient is scarce and partly controversial.Citation21,Citation59,Citation60 The failure to demonstrate better outcomes as a result of improved recognition rates and treatment programs, however, could simply reflect the inappropriateness of our illness and diagnostic models, or could be the result of suboptimal designs. It could also reflect a more general core problem: namely that our current treatment methods might not work that well in primary care conditions.
Within our medical models, we assume that treatment demonstrated as effective in randomized clinical trials (efficacy) will also work in primary care (effectiveness). This assumption neglects a considerable number of problems in primary care: patients in primary care might be different from those sampled rigidly with many inclusion and exclusion criteria in randomized clinical trials in specialized settings; doctors might not be able to practice the intervention with the same treatment integrity as specialists; treatment in primary care operates under much more restrictive conditions than in trials; less time is usually available for psychoeducation; and the length of treatment components may be shorter than in trials. The marked lack of systematic research does not allow determination of which of these factors is the most critical.
Another neglected question beyond the recognition issue is which type of mental disorder can appropriately be managed in primary care and which disorders must be treated elsewhere. During the past two decades, quite comprehensive, interdisciplinary, mental health system providers have emerged in most industrialized countries to ensure enhanced availability and improved continuity of appropriate treatment component through the illness process. At the same time (unlike in the seventies), an ever increasing number of effective medications and psychological treatments have become available, which have been shown to be effective in all types of acute depressive disorders, as well as in prevention of further episodes. Numerous national and international management guidelines and allocation rules, based on consensus meetings for more complex combined drug-psychotherapy interventions, have been developed that go far beyond the simple and naive counseling practice frequently applied in clinical routine. However, the available evidence suggests that these more or less complex networks, and their current level of coordination, do not sufficiently match the needs of depressed patients or, indeed, experts' expectations. The existing complexity of various treatments and patient management strategies developed by experts in research settings has to be more appropriately translated into clinical reality, be it in primary care or specialist settings with medical, social, or psychological focus, in order to both improve the patients' acute suffering and manage them through to long-term recovery and improve their quality of life more efficiently. Partial response, incomplete remission, as well as overlooked and persisting comorbid vulnerabilities have all been demonstrated to be unfavorable long term predictors.
Structural issues and policy in the primary care management of mental disorders
To conclude, because of the many problems with the primary care management of mental disorders, it is likely that there is no single solution. Rather, we need to address multiple solutions aimed at various levels and parts of the system simultaneously and consistently.Citation61
Patient education
Since many of the problems involve lack of understanding (and considerable misunderstanding or stigma) of mental disorders and specific diagnoses, at least some continuous and significant efforts must aim toward community and patient education. As the general public, patients, families, and potential patients of all age groups become better informed about specific mental disorders and their treatments, they are more likely to present with “real” problems and seek treatment, and to demand for specific treatment. Such pressures will certainly have some impact on the willingness of GPs to change their behavior.
Training primary care providers
Since it is undisputable that many primary care providers have only minimal training in the detection, treatment, and referral mechanisms of mental disorders, educational programs remain important in both training and practice. Such programs can at least keep providers up to date with new diagnoses, treatments, and management strategies. While other factors (time, motivation) may be important for the actual implementation, at least a very basic understanding is provided. What remains unresolved here is by what mechanisms such programs are most successfully implemented. Clearly, the endless production of guidelines is insufficient, as are continuing education programs and visits by representatives of pharmaceutical companies. Rather, we need to search for the most appropriate dissemination and translation strategies in primary care settings. More systematic research is needed to identify factors related to formats and physicians, as well those related to organizations and financial considerations assodated with successful implementation.
Clinical practice
Primary care physicians' work is subject to considerable time restrictions, in terms of the number of patients (up to 60 patients a day in some countries), the broad spectrum of all medical conditions and presenting symptoms, and the high point-prevalence of variable expressions of depressive disorders (about 10% including all types, severity, and patterns of comorbidity).Citation7,Citation15-Citation49 As managed care predominates, expectations are increasing. Particularly in countries with an extremely high average numbers of patients (over 60 patients a day in Germany), the reduction in time per patient to only a few minutes on a typical day probably forms a severe obstacle to improvement of both recognition and intervention, may it be treatment or referral. While screening tools might be partly successful in countries where GPs have at least 10 to 15 min per patient, they are clearly of little use in countries where GPs have less than 10 min with their patients.
This obstacle can only be overcome by structural changes in the organization and reimbursement schemes, because, even if simple and efficient screening tools are used, a proper differential diagnostic workup is unlikely given the GPs' short period of time per patient. The time pressure in everyday practice is also responsible for difficulties in successful referral to mental health specialists and other more efficient interventions.Citation19 Among models for this, the so-called collaborative model is the most popular. In this approach, nurses, psychologists, and social workers (primary care team) work together within the primary care setting as facilitators taking over some of the burdensome tasks of screening, monitoring, counseling, and patient education.Citation61,Citation62 Other approaches proposed the development of disease management programs for specific types of mental disorders, similar to those existing in diabetes and other chronic conditions. More critical propositions, that target explicitly the cost component, have been the implementation of pharmacy benefit manager. In this model, pharmacists review GPs' prescriptions with regard to drug, dosage, drug interactions, duration, and cost, and make recommendations to the GP and the patient (compliance and adjunctive treatment). Although this model has some attractiveness for policy makers, this approach has also negative effects in terms of invasion of privacy and interference with physicians' treatment decisions.
Research context
In order to set the context for exploring explanations for the gap between what is potentially achievable and what actually exists in primary care, there is a need for systematic stepwise inquiry in four domains: efficacy, effectiveness, practice research, and service systems research. As efficacy studies most frequently serve for approval of medications, the gold standard remains randomized clinical trials, with strict highly controlled inclusion and exclusion criteria, and mostly one or two symptom outcome measures of 8 weeks or a few weeks longer. Because primary care patients are often highly comorbid and rarely allow sufficient adherence to such strict protocols, few efficacy studies on mental health treatments are currently being conducted in primary care settings and, when they are, highly trained specialist components are usually embedded, which means that they do not reflect the typical primary care situation. These limitations call for greater emphasis on effectiveness research, which aims to establish whether an intervention has a measurable effect in broader populations and real service settings; inclusion and exclusion criteria are more relaxed, and clinicians can be less specifically trained in the research methods. The important benefit of this type of research is the expansion of outcome measures, for example, with regard to functional status, quality of life, use of health services, and costs. Because of the interest in expanding the generalization of treatments and interventions, there have been a gradually increasing number of such primary care studies, for example, in depression, suggesting that these studies are feasible in primary care, and that findings similar to those in efficacy studies can be obtained. However, one needs to acknowledge that the findings may be less robust, due to the influence of a higher variability of both patient and physician factors. In addition, explicit practice and service system research, a term that largely overlaps with quality of care evaluation studies (allocation studies, dissemination research), can additionally help identify those factors that affect choice, implementation, and delivery of treatments and services, as well as patient, provider, organizational, and cost factors, which have an impact on quality of care and outcomes of mental health treatments.
REFERENCES
- KesslerRC.McGonagleKA.ZhaoS.et alLifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity SurveyArch Gen Psychiatry.1994518198279933
- AndradeL.Caraveo-AnduagaJJ.BerglundP.et alCross-national comparisons of the prevalences and correlates of mental disorders.Bull World Health Organ,20007841342610885160
- WittchenHU.NelsonCB.LachnerG.Prevalence of mental disorders and psychosocial impairments in adolescents and young adults.Psychol Med.1998281091269483687
- Jacob!F.WittchenHU.HôltïngC.etal.Prevalence, comorbidity and correlates of mental disorders in the general population: Results from the German Health interview and examination Survey (GHS).Psychol Med. In press
- BijlRV.de GraafR.HiripiE.et alThe prevalence of treated and untreated mental disorders in five countries.Health Affairs.20032212213312757277
- WittchenHU.What is comorbidity - fact or artefact?Br J Psychiatry.1996168(suppl30)78
- ÛstùnTB.SartoriusN.Mental Illness in General Health Care: An International Study. Chichester, UK: John Wiley & sons;1995
- LindenM.MaierW.AchbergerM.et alPsychîsche Erkrankungen und ihre Behandlung in Allgemeinarztpraxen in Deutschland. Ergebnisse aus einer Studie der Weltgesundheitsorganisation (WHO).Nervenarzt.1996672052158901278
- World Health OrganizationThe ICD-10 Classification of Mental and Behavioral Disorders. Clinical Descriptions and Diagnostic Guidelines. Geneva, Switzerland: World Health Organization1992
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders. 3rd ed, revised. Washington, DC: American Psychiatric Association1987
- American Psychiatric AssociationDiagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association1994
- HeathI.Commentary: There must be limits to the médicalisation of human distress.BMJ.199931843944010084832
- KroenkeK.SpitzerRL.WilliamsJB.et alPhysical symptoms in primary care: predictors of psychiatric disorders and functional impairment.Arch FamMed.19943744779
- KatonW.SchulbergH.Epidemiology of depression in primary care.Gen Hosp Psychiatry.1992142372471505745
- GoldbergD.Epidemiology of mental disorders in primary care settings.Epidemiol Rev.199571821908521936
- SimonGE.VonKorff M.Recognition, management, and outcomes of depression in primary care.Arch Fam Med.19954991057842160
- TiemensBG.OrmelJ.SimonGE.Occurrence, recognition, and outcome of psychological disorders in primary care.Am J Psychiatry.19961536366448615408
- GoldmanLS.NielsenNH.ChampionHC.Awareness, diagnosis, and treatment of depression.J Gen Intern Med.19991456958010491249
- WittchenHU.PittrowD.Prevalence, recognition and management of depression in primary case in Germany: the Depression 2000 Study.Hum Psychopharmacol Clin Exp.200217(suppl 1)S1S11
- Von KorffM.ShapiroS.BurkeJD.et alAnxiety and depression in a primary care clinic: comparison of Diagnostic Interview Schedule, General Health Questionnaire and Practitioner Assessments.Arch Gen Psychiatry.1987441521563813810
- OrmelJ.KoeterMWJ.van den BrinkW.van de WilligeG.Recognition, management, and course of anxiety and depression in general practice.Arch Gen Psychiatry.1991487007061883252
- SchulbergHC.BlockMR.MadoniaMJ.et alTreating major depression in primary care practice.Arch Gen Psychiatry.1996539139198857868
- RegierDA.HirschfeldRMA.GoodwinFK.et alThe NIMH Depression Awareness. Recognition and Treatment Program: structure, aim, and scientific basis.Am J Psychiatry.1988145135113572847566
- EisenbergL.Treating depression and anxiety in primary care: closing the gap between knowledge and practice.N Engl J Med.1992326108010831463479
- HirschfeldR.KellerMB.PanicoS.et alThe National Depressive and Manic-Depressive Association Consensus Statement on the Undertreatment of Depression.JAMA.19972773333409002497
- SimonGE.LinEHB.KatonW.et alOutcomes of “inadequate” antidepressant treatment.J Gen Intern Med.1995106636708770718
- KatonW.Von KorffM.LinE.BushT.OrmelJ.Adequacy and duration of antidepressant treatment in primary care.Med Care.19923067761729588
- OlfsonM.KesslerRC.BerglundPA.LinE.Psychiatric disorder onset and first treatment contact in the United States and Ontario.Am J Psychiatry.1998155141514229766774
- WinterS.WittchenHU.HôflerM.et alThe Depression 2000 Study. Design, methods and characteristics of participating doctors and patients.FortschrMed.2000118(suppl 1)1121
- WittchenHU.WinterS.HôflerM.et alPrevalence and recognition of depression in primary care.Fortschr Med.2000118(suppl 1)2230
- WittchenHU.KesslerRC.BeesdoK.et alGeneralized anxiety and depression in primary care: prevalence, recognition and management.J Clin Psychol.2002632434
- BallengerJC.Current treatments of the anxiety disorders in adults.Biol Psychiatry.1999461579159410599485
- SpitzerRL.WilliamsJB.KroenkeK.et alUtility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study.JAMA.1994272174917567966923
- KatonWJ.Roy-ByrneP.RussoJ.CowleyD.Cost-effectiveness and cost offset of a collaborative care intervention for primary care patients with panic disorder.Arch Gen Psychiatry.20025910891104
- WittchenHU.ZhaoS.KesslerRC.EatonWW. DSM-III-R generalized anxiety disorder in the National Comorbidity SurveyArch Gen Psychiatry.1994513553648179459
- CarterRM.WittchenHU.PfisterH.KesslerRC.One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sampleDepress Anxiety.200113788811301924
- WittchenHU.CarterRM.PfisterH.MontgomerySA.KesslerRC.Disabilities and quality of life in pure and comorbid generalized anxiety disorder and major depression in a national survey.Int Clin Psychopharmacol.20001531932811110007
- WittchenHU.BeesdoK.KesslerRC.The impact of generalized anxiety disorder. In: Nutt DJ, Rickels K, Stein DJ, eds.Generalized Anxiety Disorder: Symptomatology Pathogenesis and Management. London, UK: Martin Dunitz20021126
- KesslerRC.KellerMB.WittchenHU.The epidemiology of generalized anxiety disorder.Psychiatr Clin North Am.200124193911225507
- HildagoRB.DavidsonJR.Generalized anxiety disorder. An important clinical concern.Med Clin North Am.20018569171011349480
- BridgesK.GoldbergD.Somatic presentations of DSM-III psychiatric disorders in primary careJ Psychosom Res.1985295635694087223
- GreenbergPE.SisitskyT.KesslerRC.et alThe economic burden of anxiety disorders in the 1990s.J Clin Psychol.199960427435
- JuddLL.KesslerRC.PaulusMP.et alComorbidity as a fundamental feature of generalized anxiety disorders: results from the National Comorbidity Study(HCS).Acta Psychiatr Scand.199898(suppl 393)611
- GoldbergDP.LecrubierY.Form and frequency of mental disorders across centres. In: Ùstùn TB, Sartorius N, eds.Mental Illness in General Health Care: an International Study. Chichester, UK: John Wiley & Sons1995323334
- MaierW.GànsïckeM.FreybergerHJ.et alGeneralized anxiety disorder (ICD-10) in primary care from a cross-cultural perspective: a valid diagnostic entityActa Psych iat Scand.20001012936
- KrauseP.WittchenHU.HôflerM.et alDesign and methods of the “Generalized Anxiety and Depression in Primary Care” study (GAD-P),MMWFortsch Med.2001119 (suppl 1)512
- KennedyBL.SchwabJJ.Utilization of medical specialists by anxiety disorder patients.Psychosomatics.1997381091129063040
- LecrubierY.WittchenHU.FaravelliC.et alA European perspective on social anxiety disorder.Eur Psychiatry.20001551610713797
- SchmidtU.Eating disorders. In: Elder A, Holmes J, eds.Mental Health in Primary Care. New York, NY: Oxford University Press2002
- TurnbullS.WardA.TreasureJ.JickH.DerbyL.The demand for eating disorder care: a study using the general practice research data base.Br J Psychiatry.19961697057128968627
- OggEC.MillarHR.PusztaiEE.ThornAS.General practice consultation patterns preceding diagnosis of eating disorders.Int J Eat Disord.19972289939140741
- KingMB.Eating disorders in a general practice population. Prevalence, characteristics and follow-up at 12-18 months.Psychol Med.1989(suppl 14)1622
- WhitehoueseAM.CooperPJ.VizeCV.HillC.VogelL.Prevalence of eating disorders in three Cambridge general practices: hidden and conspicuous morbidityBr J Gen Pract.19924257601493006
- WittchenHU.SNICAS-Studïe. Raucher und ihre Entwôhnung in der Praxis.Der Hausarzt.200285
- WittchenHU.KrauseP.UngerT.et alArterial Hypertension and Diabetes Mellitus in General Practice. Dresden, Germany: Institut fur Klinische Psychologie und Psychothérapie der TU2003
- GoldbergD.The management of anxious depression in primary care.J Clin Psychol.199960(suppl 7)3942
- HôflerM.WittchenHU.Why do primary care doctors diagnose depression when diagnostic criteria are not met?Int J Method Psychiatr Res.20009110120
- WittchenHU.Hypertension and Diabetes Screening and Awareness (HYDRA) study.MMW Fortschr Med.2003121(suppl 1)144
- BarkowK.HeunR.WittchenHU.ÙstùnTB.MaierW.Mixed anxietydepression in a 1-year follow-up study: shift to other diagnoses or remission?J Affect Disord. In press
- RïhmerZ.Can better recognition and treatment of depression reduce suicide rates? A brief review.Eur Psychiatry.20011640640911728853
- MagruderKM.NorquistGS.Structural issues and policy in the primary care management of depression.J Clin Psychol.199960(suppl 7)4551
- KatonW.Von KorffM.LinE.et alCollaborative management to achieve treatment guidelines: impact on depression in primary care.JAMA.1995273102610317897786