Abstract
Post-traumatic stress disorder (PTSD) is unique amongst psychiatric disorders in two ways. Firstly, there is usually a very clear point of onset- the traumatic event The second unique feature of PTSD is that it is characterized by a failure of the normal response to resolve. Given these two characteristics, PTSD appears a good candidate for secondary prevention, ie, interventions immediately after the trauma. Evidence available starting from current concepts and contemporary research of potential secondary prevention interventions are presented. Common practices in the aftermath of trauma such as debriefing and benzodiazepines need to be carefully considered, taking into account their potential harm to the spontaneous recovery process, and the trajectory of PTSD, and not only judging them according to their immediate (comforting) effects. A discussion of the balance required between aiding recovery but not interfering with the potent natural resolution of symptoms (that is expected in most cases), along with potential avenues of future research, are presented. Results of a small pilot study with a single intervention of hydrocortisone immediately after trauma appear to be promising, and clearly indicate the need for further studies.
El trastorno por estrés postraumático (TEPT) es singular entre los trastornos psiquiátricos por dos aspectos. Primero, porque habitualmente hay un claro punto de inicio: el acontecimiento traumático. El segundo aspecto singular del TEPT es que se caracteriza por una falla en la respuesta normal de resolución. Considerando estas dos características, el TEPT aparece como un buen candidato para la prevención secundaria, es decir, las intervenciones inmediatamente después del trauma. Se presentan las evidencias disponibles a partir de los conceptos actuales y la investigación reciente acerca de las potentiates intervenciones para la prevención secundaria. Es necesario que las prácticas habituales para las consecuencias del trauma como son el debriefing y las benzodiazepinas sean consideradas cuidadosamente, teniendo en cuenta el riesgo potencial para el proceso de recuperación espontáneo, y la evolución del TEPT, y no calificarlas sólo en relación con los efectos inmediatos (aliviadores). Se presenta una discusión acerca del balance que debe hacerse entre favorecer la recuperación y no interferir con la potente resolución natural de los síntomas (lo que se espera en la mayor parte de los casos); además se discuten los potentiates caminos para futuras investigaciones. Si bien parecen ser promisorios los resultados de un pequeño estudio piloto en que se empleó una dosis única de hidrocortisona inmediatamente después del trauma, es claro que se requieren futuros estudios.
L'état de stress post-traumatique (ESPT) est un trouble psychiatrique original par deux aspects. Tout d'abord, son point de départ est habituellement très clair, l'événement traumatique, La seconde caractéristique originale de l'ESPT se traduit par un échec de la réponse normale pour le résoudre. Ces deux caractéristiques font de l'ESPT un bon candidat pour la prévention secondaire, c'est-à-dire pour une intervention immédiate après le traumatisme. Nous présentons ici les arguments en faveur des interventions de prévention secondaire potentielles issus des concepts et de la recherche actuels. Les pratiques courantes utilisées dans les suites de traumatisme comme le debriefing et les benzodiazepines méritent d'être envisagées avec précaution, en prenant en compte leur potentiel délétère sur le processus de guérison spontanée et l'évolution de l'ESPT, et sans tenir compte uniquement de leurs effets (bénéfiques) immédiats. Une discussion de l'équilibre nécessaire entre l'aide à la guérison sans interférence avec la possibilité de résolution naturelle des symptômes (attendue dans la plupart des cas), et les éventuelles perspectives offertes par la recherche future est présentée. Les résultats d'une petite étude pilote sur l'administration unique d'hydrocortisone immédiatement après le traumatisme semblent prometteurs et indiquent clairement le besoin d'études supplémentaires.
Post-traumatic stress disorder (PTSD) is a disorder where patients are haunted by their traumatic memories. For a patient with PTSD, it is as if time has stopped. It could be 10, 20 (or even more) years after the exposure, yet he/she is still there, reliving, re-experiencing, and retraumatized by the event which changed his or her life so dramatically.
What is a traumatic event which could lead to PTSD? In DSM-IV, such an event was defined as “an event or events that involved actual or threatened death or serious injury, or a threat to the physical integrity of self or others.”Citation1 However, as such a description might leave too much room for different interpretations, the intention in DSM-5 is to tighten this up somewhat. One suggestion is to specify that the event involves death, serious physical injury, or sexual violation (either actual or threatened), and that this exposure takes the form of a personal experience, first-hand witnessing of the event as it occurred to others, learning of the event as it occurred to a close friend or relative, or repeated exposure to the event as it occurred to others (such as to police officers or paramedics repeatedly exposed to the traumatic experiences of others).
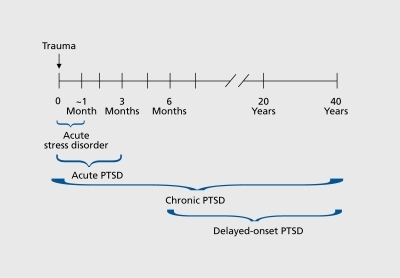
An important part of the definition of PTSD is the time requirement - at least a month following the trauma - which means that one cannot diagnose PTSD during the first month after the exposure. Acute PTSD is considered if the symptoms last more than a month and up to 3 months (if it is more than 3 months, it is defined as chronic PTSD - ). Beyond the actual presence of the relevant symptoms, the sixth criterion for clinical diagnosis of PTSD is clinically significant distress or impairment of functioning, which is a common denominator for all anxiety disorders.
In the minds of many, PTSD is related to mega-events such as 9/11, tsunami, war, etc. However, the major contributors to PTSD are actually daily civilian events, such as car accidents, work-related accidents, violence, and armed robbery, to name a few PTSD can also occur after exposure to a serious illness (for example myocardial infarction). In modern civilian life, exposure to traumatic events (that might lead to PTSD) is prevalent. In fact, about 50% of the (Western) population would have been exposed to a traumatic event that might later on lead to PTSD during their lifetime.Citation2
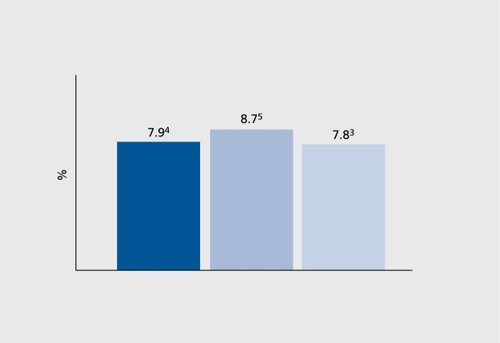
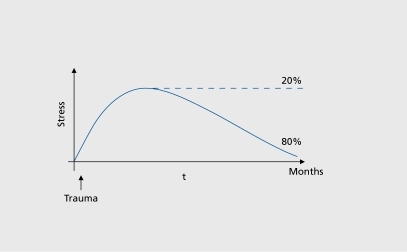
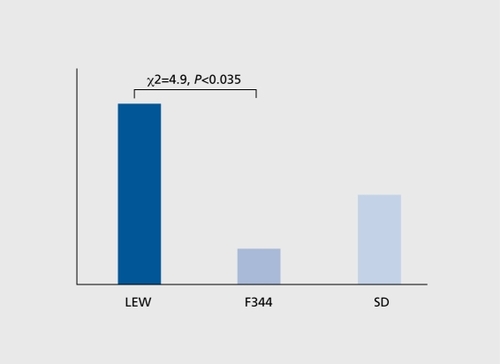
What is unique about PTSD is that the vast majority (80% to 90%) of those exposed to this type of trauma will eventually adapt. Only 10% to 20% become fixated on the event, and develop PTSD.Citation3 If 50% of the population are exposed at some point of their life to traumatic events, and if on average 15% of them will develop PTSD, then the expected prevalence of PTSD in the population would be 7.5%. Indeed, in the National Comorbidity Survey,Citation2 the prevalence was found to be 6.8%, while in earlier studies the prevalence ranged from 7.8% to 8.7%Citation3-Citation5 ().
What are the risk factors for PTSD?
Pretraumatic risk factors
A meta-analysis of risk factorsCitation6 proposed trauma intensity as an important factor, along with previous traumatic history,Citation7 family history of psychiatric disorders,Citation8,Citation9 personal history of emotional or psychiatric disorders prior to the trauma, history of substance abuse, and poorer intellectual abilities.Citation10 In a semiprospective study conducted by our group,Citation11 we compared 2362 war veterans who developed PTSD with an equal number of war veterans who did not develop PTSD. Comparisons were made on predrafting personal factors and pretrauma army characteristics. The intention was to find out whether careful predrafting cognitive and behavioral screening would help to predict who will develop PTSD. It turned out that neither behavioral assessment, including measures such as socioeconomic background and motivation to serve, nor training were found to predict PTSD. Hence, predraft screening done at age 17 failed to predict who would develop PTSD either during their mandatory service (age 18 to 21), or during reserve duties (age 21 to 49). The only exception was a borderline significance related to intelligence, which in any case measures the ability of individuals to adapt, and is therefore believed to be a nonspecific mediator.
Post-traumatic risk factors
The intensity and magnitude of the immediate response to the traumatic event are associated with increased risk of developing PTSD. Reactions like dissociative symptoms, panic-like response, extreme withdrawal, psychotic-like symptoms, and suicidality all raise red flags regarding the person's vulnerability to developing PTSD.Citation11
Why is PTSD suitable for prevention?
PTSD is different from other psychiatric disorders, in that it has a very clear point of onset. In most cases, the traumatic event is also the point of onset of symptoms. The second unique feature of PTSD is that it is characterized by a failure of the normal response to disappear. The expected response after exposure to a traumatic event is to experience shock, horror fear, terror, grief, etc. This is a normal response to an abnormal situation. It becomes a disorder when this normal response continues (according to DSM-IV, for more than a month). Moreover, as mentioned earlier, the vast majority (80% to 90%) experience spontaneous recovery from these symptoms, and hence, one way to conceptualize PTSD is as a disorder where there is a failure to recover (). If PTSD is a failure to recover, then our obligation, as clinicians, to the patient is primum non nocere (“First, do no harm” ), ie, not to interfere with the potent spontaneous recovery process which usually takes place. It seems that what we do in this “window of opportunity,” in those “golden hours” - the first few hours after the exposure to the traumatic event - might have the potential to dramatically alter the trajectory of PTSD.
Memory and PTSD
We submit that the main feature of PTSD is the traumatic memory, which is clinically expressed by criterion B of the DSM-IV, namely that the traumatic event is persistently re-experienced through recurrent and intrusive distressing recollections and/or recurrent distressing dreams, acting or feeling as if the traumatic event were recurring (including dissociative flashback episodes) and intense psychological distress and physiological reactivity upon exposure to internal or external cues that symbolize or resemble an aspect of “the event.” Thus, the core pathology of PTSD is the re-experiencing - the distressing recollections, flashbacks, nightmares, etc. One way to describe this is that patients with PTSD arc haunted by the memory of the event. For them, the past is always present; it is as if the clock has stopped, and they are constantly either reliving the experience, or fighting very hard not to be exposed to triggers which might set off a flashback. The avoidance, numbing, and increased arousal would then be secondary phenomena. One question would be regarding the consolidation of the traumatic event. Consolidation is the transition from unstable to stable memory, and the question is, if we could prevent this consolidation, whether or not it would be beneficial.
When individuals with traumatic brain injury with amnesia of the traumatic events were compared with those without amnesia, it was found that 6% of those with amnesia of the traumatic presented PTSD symptoms at a 6-month follow-up, as opposed to 23% in those without amnesia.Citation12 This naturalistic study suggests that impaired memory for the traumatic event reduces the risk for PTSD.
Repressive coping style and PTSD
A repressive coping style is a cognitive and emotional strategy aimed at ignoring or diverting attention from a threatCitation13 and, in a way, could mimic amnesia. If the hypothesis is that amnesia for traumatic events reduces the rate of PTSD, we would expect that individuals with repressive coping styles would be less vulnerable to developing PTSD. Indeed, in a study of prevalence of PTSD after MI,“ it was found that in individuals with repressive coping style the prevalence of PTSD was lower (7.1%), as compared with individuals with low anxiety (20%), high anxiety (19.4%) or defensive coping style (17.2%) - Table I.
Table I. Repressive coping style. PTSD, post-traumatic stress disorder. Adapted from ref 14: Ginzburg K, Solomon Z, Bleich A. Repressive coping style, acute stress disorder, and posttraumatic stress disorder after myocardial infarction. Psychosom Med. 2002;64:748-757. Copyright © Lippincott Willams and Wilkins 2002
Actually, the possibility that repressive coping style could be an adaptive way of dealing with trauma has been known for close to 30 years.Citation15 This observation was described as follows: “Avoidance, suppression, and denial (avoiding coping strategies) are effective in reducing traumatic stress-induced distress.”
Debriefing and spontaneous remission
If a reduction in fear memory associated with the trauma is beneficial, then psychological interventions which enhance memories of the trauma, eg, debriefing, would interfere with the potent beneficial spontaneous recovery. In a study of psychological debriefing for road traffic accident victims,Citation16 it was found in a follow-up 4 months and 3 years after the accident, that a subset of individuals - those who experienced high anxiety after the accident and received debriefing - were doing significantlyworse (as measured by Impact of Event Score), 4 months and 3 years later, as compared with those who did not receive the debriefing. That is, the expected and welcome spontaneous recovery process was hampered by this intervention, which is associated with enhancing memories of the traumatic event. Other studiesCitation17-Citation20 also reported similar findings, and a meta-analysisCitation21 also supported the caution that one should exercise in indiscriminate utilization of single-session debriefing.
Amnesia and medications
What about medications which might have a potential effect on consolidation of the traumatic memory? How would intervention with medication which modulates consolidation of emotional memory fit with the theme that reduction in fear memory associated with trauma is beneficial?
It is quite common to use benzodiazepine (BNZ) in order to calm down the horror and fear associated with exposure to a traumatic event. However, BNZ is associated with enhancing access to emotional memories (but not to procedural memory). Actually, until the 1970s, one of the major techniques to treat PTSD was via the “benzodiazepine interview,” which used BNZ (or sodium pentothal) in order to help the individual to go through full re-experience of the event. However, how does this fit with our line of reasoning that reducing fear memory is beneficial? In a small study, Gelpin et alCitation22 compared at 1-and 6-month follow-up individuals who received BNZ (clonazepam 2.6 mg/day or alprazolam 2.5 mg/day) with those who did not receive it. Out of the 13 who received BNZ, 9 developed PTSD, as compared with 3 of the 13 controls. These findings were also replicated by Mellman et al in a small study.Citation23 In a unique animal model, which is based on setting affected (rats) apart from the unaffected,Citation24 administration of alprazolam 1 hour after the exposure was associated with significantly more extreme behavioral response (the behavioral equivalent of PTSD) for the rats who were given alprazolam as compared with those who got saline.Citation25 Hence, some pilot human data, plus a signal from animal studies suggest that early administration of BNZ might interfere with the normal potent spontaneous recovery.
Hypothalamic-pituitary-adrenal axis, PTSD, and BNZ
Glucocorticoids were found to reduce phobic fear in humans.Citation26 Individuals with arachnophobia who were injected with Cortisol 1 hour before exposure reported less fear (as measured on a visual analog scale) as compared with individuals who got saline.
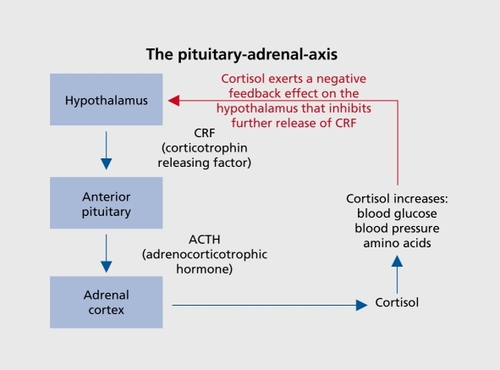
Stress is associated with activation of the hypothalamicpituitary-adrenal (HPA) axis, and consequently with secretion of hydrocortisone. What is the effect of BNZ on this normal, primary cornerstone of the normal response to stress? What is the effect of BNZ on Cortisol? Why does administration of BNZ seem to interfere with the normal recovery process? Administration of BNZ abolishes the expected activation (the normal response) of the HPA axis.
The HPA axis is the main component in the neuroendocrine response to acute and chronic stress (). In response to stress, a chain of reactions stimulates the adrenal cortex to synthesize and release glucocorticoids, in particular Cortisol. These hormones are instrumental in adaptation to stress.Citation27 A main function appears to be in the regulation and containment of the sympathetic and parasympathetic responses to stress (ie, changes in heart rate, blood pressure, respiration), responses that help the body accommodate to an immediate demand. In animal studies, it has been demonstrated that blunted HPA-axis response increased PTSD-like reactions in rats exposed to trauma,Citation28 which strengthens the notion that an intervention aimed at bolstering this natural response with an early intervention immediately after the trauma could help reduce PTSD ().
However, the data supporting a potential low plasticity of the HPA axis as a potential risk factor for PTSD does not derive only from animal studies. In a study looking at the trajectory of PTSD in motor accident victims,Citation29 it was found that patients who developed PTSD had significantly less urinary Cortisol compared with individuals who experienced the same trauma, but did not develop PTSD. Taking together the human and animal data suggests that a proper reactivity (plasticity) of the HPA axis is instrumental for spontaneous remission after exposure to a traumatic event.
BNZs do exactly the opposite - they abolish the usual HPA axis response, and it is conceivable that this might have a calming effect to begin with, but in the long run it might increase the risk of developing PTSD. A potential explanation for this might be associated, among other activities, with the role of Cortisol, not only in decreasing the fear response, but also in its conceivable role in consolidation of the traumatic memory.
Cortisol administration in the “golden hours”
The logical step at this point would be to see whether early administration of Cortisol would be associated with secondary prevention of PTSD. Looking at a medical setting where patients usually receive Cortisol (as part of their treatment) could provide us with a hint regarding the question of the potential beneficial role of early administration of Cortisol after exposure to traumatic events.
In an intensive care unit, after cardiac surgery, some patients receive Cortisol as part of their treatment. Indeed it was found that those who were treated with Cortisol seemed to have significantly fewer traumatic memories compared with those who did not.Citation30 This had also been found in a study of septic shock patients.Citation31
Would an immediate, postexposure intervention clinically affect the restoration of stability, encourage resilience, and improve the ability to cope and thrive in the face of adversity? Or, to put it differently, would stress doses of hydrocortisone be useful for secondary prevention of PTSD?
This question was tested in an animal model study,Citation32 which aimed to address the question of the value of prescribing a single dose of Cortisol, immediately after being exposed to a traumatic event. The results were quite impressive - medium-to-high doses of hydrocortisone given 1 hour after exposure to the smell of a predator were associated with significantly less “anxiety index” (a measure which takes into account time spent in open arms, time spent on exploration, and number of openarm entries). The finding suggests that early administration of corticosterone significantly decreased the vulnerability and increased resistance to PTSD, and that at least a part of the effect is through involvement in memory consolidation.
However, it is not always simple to give hydrocortisone immediately after the event, in this short window of opportunity. Consequently, the question arises of whether hydrocortisone administration would be useful if not administered right after the exposure (in the “golden hours”). When the same dose of Cortisol was administered 14 days after the stressor and 1 hour after presenting a reminder, the results were strikingly different. Cortisol given not in the “golden hours” was totally ineffective in reducing the “anxiety index.”
The current lack of prospective studies following the lead of animal studies regarding the potential utility for early administration of Cortisol spurred us to initiate a pilot study to examine this.Citation33 Three major points were raised. The first was whether psychiatry has a “window of opportunity” for treatment as in other medical fields (ie, stroke or myocardial infarction). The second was whether it would be possible to reach people within a short time after the trauma and to give them the treatment in a timely fashion. The third question is whether a single medium to high dose of IV hydrocortisone (1 00 to 120 mg) would alter the trajectory of PTSD. In this study, the window of opportunity was limited to the first 6 hours after the exposure, and consequently this was done in the emergency room of a general hospital. Patients who had a higher risk of developing PTSD were selected, in order to have an enriched sample. To achieve this, the patients selected were those fulfilling criteria A, 2 of the symptoms in criteria B, 3 out of 4 of criteria C, D, E, and F, and meeting criterion H of the ASD criteria set out in DSM-IV.Citation1
Twenty-five patients were recruited from the emergency room; 20 after traffic accidents and 5 following other civilian events. They were randomly assigned to treatment with IV hydrocortisone (100 to 140 mg) (n=15) or placebo (n=10).The patients were followed up by telephone the day after the treatment, and then at 2 weeks, 1 month, and 3 months, with a personal interview including the Clinician Administered PTSD Scale (CAPS). Out of the 25 patients, 19 completed 2 weeks, 15 completed 1 month, and 17 completed the 3-month followup. The results of this preliminary study suggest that Cortisol was effective in reducing both acute stress disorder (20% in the Cortisol group vs 66.7% in the placebo condition) as well as rates of PTSD (12.5% vs 37.5% at 1month (ns), and 0% vs 37.5% at 3-month follow-up). This is shown in .
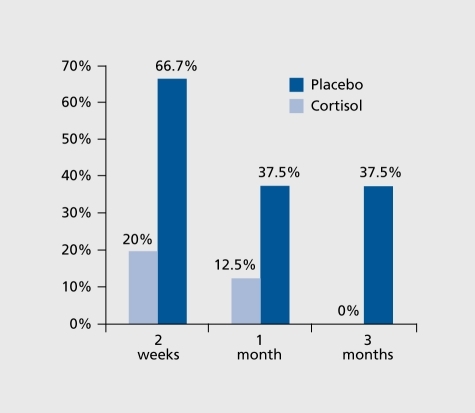
The results reflect both the utility of the enriched sample concept, ie, in the placebo group, 37.5% had indeed developed PTSD at 1- and 3-month follow up, and it also points out the effect of early intervention with hydrocortisone, as only 12.5% at 1 -month and none at 3month follow-up presented with PTSD.
There are other studies which look at long-term effects of early administration of different pharmacological interventions. The first one was a study by Pitman et al,Citation34 in which administration of propranolol for 10 days was compared with placebo given in the same fashion. In this study, supported also by the work of Debiec and Ledoux,Citation35 a modest effect of early propranolol administration was found. However, follow-up studies failed to replicate this initial positive yet modest response.Citation36-Citation37
Another possibility explored as a potentially beneficial “golden hours” intervention is related to morphine. A lower rate of PTSD was found in a large retrospective study which included 696 American soldiers in Iraq with serious injuries, out of whom 243 developed PTSD and 453 did not.Citation38 The major finding is related to the difference in prevalence of morphine administration for those two groups. A significantly lower percentage of individuals got morphine in the PTSD group than in the group that did not develop PTSD (61 % vs 76% respectively). This work is in line with an earlier small study with similar findings.Citation39
Clinical implications
As it seems that traditional approaches like debriefing and anxiolytics (BNZ) are not effective, and might actually interfere with the recovery process, what should a clinician do for a patient who comes to the emergency room after experiencing a trauma? We suggest differentiating between acute stress management and acute stress reaction treatment.
The acute stress management is not usually carried out by mental health professionals, and should be designed accordingly. The goals are to help the individual to return to full functioning, help him or her to regain behavioral and emotional control, and facilitate restoration of interpersonal communication. The management should focus on addressing basic needs. Firstly, reducing the exposure to the stress (ie, finding a secure place, etc). Secondly, restoring physiological needs (food, drink, hygiene, etc), and also providing some information and orientation, and helping to locate a source of support (family, friends, etc) along with emphasizing the expectation of returning back to normal. Alongside the actions that need to be taken, there arc interventions that should not be done. This is summarized as the three Ps, namely: don't Pathologize (“this is a normal response to an abnormal situation”), don't Psychologize (don't facilitate emotional reaction via group therapy, or stressful debriefing), and don't Pharmacol ogize (Table II). Citation40
Table II. What not to do; the “3R”
The treatment goes along the same lines, with an emphasis on return to previous functioning via affirmation of self-control and facilitation of return to previous activities. If the expected recovery does not take place after a couple of months, then referral to specific psychological intervention in the framework of cognitive behavioral therapy should be explored.Citation41
Conclusion
PTSD is a severe, disabling disorder, with dramatic consequences, both on the individual him- or herself and his or her family. The core symptom is the traumatic memory, and the patient is constantly haunted by the memory of the event; for him or her the past is always present. It is conceivable that the future of this disorder would focus on the window of opportunity (“golden hours”), ie, intervention in the first few hours after the exposure. Whilst we continue the search for a “morningafter pill,” it is important first to make sure that our intervention does not interfere with the normal potent recovery process which takes place in the majority of patients. Along these lines, the contemporary knowledge about debriefing and use of BNZ should be considered at these stages. Interventions such as adrenergic medication (like propranolol or morphine) have been studied. As for propranolol, replications of the data were not encouraging, and morphine has its inherent consequences, which should be taken into account. Animal studies of Cortisol appear promising, and the same is true for pilot data in humans, but undoubtedly more work should be done in order to better explore and consequently improve our current strategies.
PTSD provides a unique opportunity for exploring secondary prevention in psychiatry, and from a disorder that is often associated with guilt and accusations, it has the potential to become a disorder where scientific knowledge could open a window to dramatically changing its trajectory.
REFERENCES
- American Psychiatric Association.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association1994
- KesslerRC.BerglundP.DernierO.JinR.MerikangasKR.WaltersEE.Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication.Arch Gen Psychiatry.20056259360215939837
- KesslerRC.SonnegaA.BrometE.HughesM.NelsonCB.Posttraumatic stress disorder in the National Comorbidity Survey.Arch Gen Psychiatry199552104810607492257
- DavidsonJR.HughesD.BlazerDG.GeorgeLK.Post-traumatic stress disorder in the community: an epidemiological study.Psychol Med.1991217137211946860
- BreslauN.DavisGC.AndreskiP.PetersonE.Traumatic events and posttraumatic stress disorder in an urban population of young adults.Arch Gen Psychiatry1991482162221996917
- BrewinCR.AndrewsB.ValentineJD.Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults.J Consult Clin Psychol.20006874876611068961
- EngelCC.Jr.EngelAL.CampbellSJ.McFallME.RussoJ.KatonW.Posttraumatic stress disorder symptoms and precombat sexual and physical abuse in Desert Storm veterans,J Nerv Ment Dis.19931816836888228950
- FontanaA.SchwartzLS.RosenheckR.Posttraumatic stress disorder among female Vietnam veterans: a causal model of etiology.Am J Public Health.1997871691759103092
- KulkaRA.SchlengerWE.FairbankJA.et al.Trauma and the Vietnam Vilar Generation: Report of Findings from the National Vietnam Veterans Readjustment Study. Brunner/Mazel psychosocial stress series, No. 18. Philadelphia, PA: Brunner/Mazel1990
- GurvitsTV.GilbertsonMW.LaskoNB.et al.Neurologic soft signs in chronic posttraumatic stress disorder.Arch Gen Psychiatry.20005718118610665621
- ZoharJ.FostickL.CohenA.et al.Israeli Consortium on PTSD. Risk factors for the development of posttraumatic stress disorder following combat trauma: a semiprospective study.J Clin Psychiatry.2009701629163519852906
- GilS.CaspiY.Ben-AriIZ.KorenD.KleinE.Does memory of a traumatic event increase the risk for posttraumatic stress disorder in patients with traumatic brain injury? A prospective study.Am J Psychiatry.200516296396915863799
- RothSusanCohenLawrenceJ.Approach, avoidance, and coping with stress.Am Psychologist.198641813819
- GinzburgK.SolomonZ.BleichA.Repressive coping style, acute stress disorder, and posttraumatic stress disorder after myocardial infarction.Psychosom Med.20026474875712271105
- LazarusRS.The costs and benefits of denial. In Breznitz S, ed.The Denial of Stress. New York, NY: International Universities Press1983130
- MayouRA.EhlersA.HobbsM.Psychological debriefing for road traffic accident victims. Three-year follow-up of a randomised controlled trial.Br J Psychiatry.200017658959310974967
- BromD.KleberRJ.HofmanMC.Victims of traffic accidents: incidence and prevention of post-traumatic stress disorder.J Clin Psychol.1993491311408486794
- HobbsM.AdsheadG.Preventive psychological intervention for road crash survivors. In: Mitchell M, ed.The Aftermath of Road Accidents. London, UK: Routledge1997159253
- ZatzickDF.Roy-ByrneP.RussoJE.et al.Collaborative interventions for physically injured trauma survivors: a pilot randomized effectiveness trial.Gen Hosp Psychiatry.20012311412311427243
- SijbrandijM.OlffM.ReitsmaJB.CarlierIV.GersonsBP.Emotional or educational debriefing after psychological trauma. Randomised controlled trial.Br J Psychiatry.200618915015516880485
- van EmmerikAA.KamphuisJH.HulsboschAM.EmmelkampPM.Single session debriefing after psychological trauma: a meta-analysis.Lancet.200236076677112241834
- GelpinE.BonneO.PeriT.BrandesD.ShalevAY.Treatment of recent trauma survivors with benzodiazepines: a prospective study.J Clin Psychiatry.1996573903949746445
- MellmanTA.BustamanteV.DavidD.FinsAI.Hypnotic medication in the aftermath of trauma.J Clin Psychiatry.2002631183118412530420
- CohenH.ZoharJ.MatarM.The relevance of differential response to trauma in an animal model of post-traumatic stress disorder.Biol Psychiatry.20035346347312644351
- MatarMA.ZoharJ.KaplanZ.CohenH.Alprazolam treatment immediately after stress exposure interferes with the normal HPA-stress response and increases vulnerability to subsequent stress in an animal model of PTSD.Eur Neuropsychopharmacol.20091928329519167197
- SoraviaLM.HeinrichsM.AerniA.et al.Glucocorticoids reduce phobic fear in humans.Proc Natl Acad Sci U S A.2006103558516567641
- LupienSJ.MaheuF.TuM.FioccoA.SchramekTE.The effects of stress and stress hormones on human cognition: Implications for the field of brain and cognition.Brain Cogn.20076520923717466428
- CohenH.ZoharJ.GidronY.MatarMA.et al.Blunted HPA axis response to stress influences susceptibility to posttraumatic stress response in rats.Biol Psychiatry.2006591208121816458266
- DelahantyDL.RaimondeAJ.SpoonsterE.Initial posttraumatic urinary Cortisol levels predict subsequent PTSD symptoms in motor vehicle accident victims.Biol Psychiatry.20004894094711074232
- SchellingG.KilgerE.RoozendaalB.et al.Stress doses of hydrocortisone, traumatic memories, and symptoms of posttraumatic stress disorder in patients after cardiac surgery: a randomized study.Biol Psychiatry.20045562763315013832
- SchellingG.BriegelJ.RoozendaalB.StollC.RothenhäuslerHB.KapfhammerHP.The effect of stress doses of hydrocortisone during septic shock on posttraumatic stress disorder in survivors.Biol Psychiatry.20015097898511750894
- CohenH.MatarMA.BuskilaD.KaplanZ.ZoharJ.Early post-stressor intervention with high-dose corticosterone attenuates posttraumatic stress response in an animal model of posttraumatic stress disorder.Biol Psychiatry.20086470871718635156
- ZoharJ.YahalomH.KoslovskyN.et al.High-dose hydrocortisone immediately after trauma may alter the trajectory of PTSD: Interplay between clinical and animal studies.Eur Neuropsychopharmacol. In press.
- PitmanRK.SandersKM.ZusmanRM.et al.Pilot study of secondary prevention of posttraumatic stress disorder with propranolol.Biol Psychiatry.20025118919211822998
- DebiecJ.LedouxJE.Disruption of reconsolidation but not consolidation of auditory fear conditioning by noradrenergic blockade in the amygdala.Neuroscience.200412926727215501585
- SteinMB.KerridgeC.DimsdaleJE.HoytDB.Pharmacotherapy to prevent PTSD: Results from a randomized controlled proof-ofconcept trial in physically injured patients.J Trauma Stress.20072092393218157888
- NugentNR.ChristopherNC.CrowJP.BrowneL.OstrowskiS.DelahantyDL.The efficacy of early propranolol administration at reducing PTSD symptoms in pediatric injury patients: a pilot study.J Trauma Stress.20102328228720419738
- HolbrookTL.GalarneauMR.DyeJL.QuinnK.DoughertyAL.Morphine use after combat injury in Iraq and post-traumatic stress disorder.N Engl J Med.201036211011720071700
- BryantRA.CreamerM.O'DonnellM.SiloveD.McFarlaneAC.A study of the protective function of acute morphine administration on subsequent posttraumatic stress disorder.Biol Psychiatry.20096543844019058787
- ZoharJ.SonninoR.Juven-WetzlerA.CohenH.Can posttraumatic stress disorder be prevented?CNS Spectr.200914:1(suppl 1)445119169193
- DavidsonJR.SteinDJ.ShalevAY.YehudaR.Posttraumatic stress disorder: acquisition, recognition, course, and treatment.J Neuropsychiatry Clin Neurosci.20041613514715260364