Abstract
Background
Chronic rhinosinusitis (CRS) is a disease characterized by inflammation of the mucosa lining the paranasal sinuses; however, recent evidence also indicates the involvement of the sinus bones in the inflammatory process. CRS is a disease with different phenotypes; nonetheless, the characterization of osteitis in the different CRS phenotypes is poorly characterized. Herein, we report on osteitis in two main phenotypes of CRS: a group allergic to aeroallergens who suffers from long-lasting upper airway allergy, and the CRS group with no upper airway allergy.
Patients and methodology
A total of 51 patients (23 females and 28 males, with a mean age of 39.03±13.4) who underwent surgery in our university hospital contributed to this study by providing bone samples from the ethmoid bone. They were divided into three groups: group I is patients who underwent septoplasty with or without partial inferior turbinectomy, and they acted as the control group; group II is patients who underwent operation for non-allergic CRS (NACRS); and group III is patients who underwent operation for allergic CRS (ACRS). Sections of the decalcified ethmoid bone were stained with hematoxylin and eosin for histological evaluation for osteitis (periosteal thickening and remodeling, osteoblastic and osteoclastic activity, and osteomyelitis and bone destruction) that was graded from 0 to IV, where grade 0 is normal histology and grade IV is frank osteomyelitis and bone destruction.
Results
Descriptive histology of the ethmoid bone analysis demonstrated osteitis of different grades in patients suffering from CRS with or without upper airway allergy. In the ACRS group, 80% demonstrated grade I osteitis, and 20% grade II. However, 11.11% of the NACRS group demonstrated normal bone histology, and 88.88% demonstrated osteitis: 33.33% demonstrated grade I, 50% grade II, and 5.5% grade III. The control group showed normal bone histology in 90.47% and grade I osteitis in 9.52%. The mucosal disease was higher in the grade of inflammation than the osteitis in both CRS groups (II and III). There was no correlation between the mucosal and bone grade of inflammation in both CRS groups.
Conclusion
Herein, we show evidence of osteitis in ACRS and confirm the presence of a higher grade osteitis in the NACRS patients. This sinus bone remodeling may contribute to the chronicity of the disease and carries special consideration in the treatment of CRS.
In the field of rhinology, the majority of studies focus on mucosal immunology of the nose without giving attention to the underlying bones. Recent evidence indicates that the inflammation of chronic rhinosinusitis (CRS) is beyond the mucous membrane and involves the underlying bone of the paranasal sinuses as well. Patients with CRS are radiologically assessed with computed tomography (CT) scans that often reveal areas of increased bone density and irregular thickening of the sinus walls. This could explain the recurrence of the mucosal disease after surgical treatment and may indicate that these osteitic lesions act as the source of the chronic inflammation (Citation1–(Citation3). Therefore, proper understanding of the magnitude of bone involvement in CRS inflammation is mandatory for proper treatment. Renato et al. (Citation4) studied the ethmoid bone from 20 patients undergoing endoscopic sinus surgery for CRS, and they reported that the histopathological findings suggested associated osteitis of the underlying ethmoid bone. In a study of the impact of osteitis in CRS on disease severity, the authors found osteitis to be associated with worse baseline measures of disease severity and inflammation (Citation5). Georgalas et al. (Citation6) found that in patients with recalcitrant CRS who have undergone multiple surgeries in the past, the incidence of osteitis can be as high as 64%.
Although it seems certain from the evidence mentioned so far that osteitis is an effector factor in CRS pathophysiology, it is surprisingly an area of research that has not been explored sufficiently. Moreover, no reports have looked at osteitis in CRS patients with atopy or allergy versus CRS patients without allergy. Therefore, our aim in the current study was to evaluate the grade of osteitis in the ethmoid bone from patients who had endoscopic sinus surgery for their CRS and to look at the differences between osteitis in atopic patients versus non-atopic ones. We also correlated the grade of osteitis to the grade of mucosal disease to have an overall evaluation of the inflammatory process in the studied CRS groups. Herein, we show that the ethmoid bone from Allergic CRS (ACRS) patients demonstrated osteitis; however, the grade of this osteitis was less than that of the non-allergic CRS (NACRS) patients. Interestingly, although both groups had mucosal inflammation, there was no correlation in the inflammation grading between the bone and mucosa in both groups (i.e., ACRS and NACRS).
Materials and methods
Patients
A total of 51 patients, who had not undergone operation before for CRS, contributed to this prospective study. There were 23 females and 28 males, with ages ranging between 21 and 66 years, and a mean age of 39.03±13.4 years. They were divided into three groups: group I comprised 21 control patients (M:F°=13:8) who underwent operation for septoplasty with or without turbinoplasty of the inferior turbinates. The deviated part of the perpendicular plate of the ethmoid was studied as a control for the ethmoid bone's osteitic activity from CRS patients. These patients were suffering from neither allergy nor CRS. Group II was 19 patients (M:F°=9:10) who underwent operation for CRS with or without nasal polyps affecting both sides. These patients were neither allergic to aeroallergens nor atopic, as judged by skin tests and a radioallergosorbent test (RAST). The ethmoid bone removed during ethmoidectomy was studied for osteitic activity. Finally, group III was 11 patients (M:F°=6:5) who underwent operation for CRS with or without nasal polyps affecting both sides, and who were having long-lasting allergic rhinitis that was suboptimally controlled and that resulted in CRS as a complication of their nasal allergy. The ethmoid bone removed during ethmoidectomy was studied for osteitic activity. Patients with recalcitrant CRS or allergic fungal sinusitis were excluded from the current study.
Bone preparation for histopathology
The bone specimens were fixed in 10% neutral buffered formalin for more than 24 h, routinely decalcified in formic acid solution, and embedded in paraffin. Sections of 4 µm of each specimen were stained with hematoxylin and eosin for histological evaluation.
The evaluation was performed in a double-blinded fashion for osteitis grading. We used a bony grading as used by Biedlingmaier et al. (Citation7), who graded the osteitis into five grades: grade 0 for normal bone; grade I for periosteal thickening; grade II as in I, in addition to osteoblastic and osteoclastic activity with bone resorption and/or remodeling; grade III as in II, in addition to wide osteoid matrix; and grade IV is frank osteomyelitis, leucocytes infiltration, and bone destruction. We tried to count the number of inflammation cells in bone specimens, but that was not possible in the majority of cases.
For the mucosal grading, we also adopted the same grading system as Biedlingmaier et al. (Citation7). Four grades was defined: grade 0 is for normal histology, grade I is for mild chronic inflammatory cells infiltrate, grade II is for mild to moderate scattered chronic inflammatory cells infiltrate, grade III is for moderate amounts of chronic inflammatory cells infiltrate, and grade IV is for severe significant amounts of chronic inflammatory cells infiltrate in the lamina propria. The evaluation was performed utilizing a Leitz Laborlux D microscope at 40× (high-power field).
Statistical analysis
The correlation between mucosal and bone inflammation was evaluated by Pearson's test using GraphPad Prism statistical software, version 5.
Results
Osteitis in different studied groups
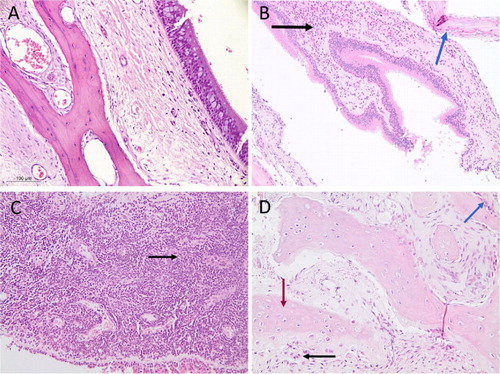
A descriptive histology of one patient representative of each studied group is demonstrated in . A represents the histology from one control patient who underwent septoplasty with partial inferior turbinectomy, and it shows normal histology. In contrast, the histology from the ACRS group (B) demonstrated mixed inflammatory cells infiltrating the lamina propria, including numerous eosinophils, with thick periosteum around the lamellar bone; and the histology from the NACRS group showed severe inflammatory cell infiltrate, predominantly lymphocytes and plasma cells, with osteoid bone interconnected haphazardly with increased osteoblastic and osteoclastic activity.
Fig. 1 Descriptive histology of the ethmoid bone and nasal mucosa. (A) Control: thinner lamina propria with few vessels, thin trabeculae of mature lamellar bone, and a very thinned periosteum. (B) Allergic chronic rhinosinusitis (ACRS): mixed inflammatory cells infiltrating the lamina propria, including numerous eosinophils (black arrow), with thick periosteum around the lamellar bone (blue arrow). (C,D) Non-allergic chronic rhinosinusitis (NACRS): (C) severe inflammatory cells, predominantly lymphocytes and plasma cells (black arrow); and (D) osteoid bone interconnected haphazardly (red arrow) with osteoblastic rim (blue arrow) and focal osteoclastic activity (black arrow).
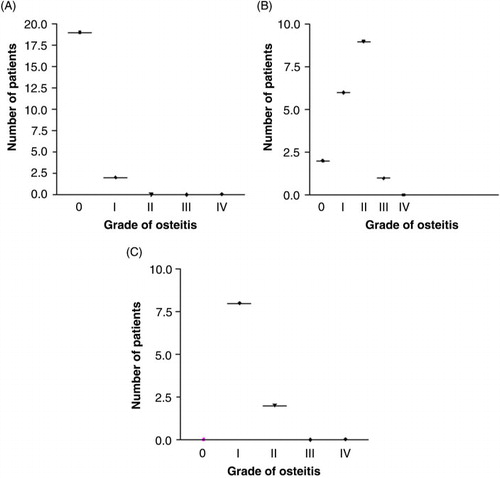
Grade of osteitis in different studied groups
All 51 patients’ histological slides were reviewed in a blinded fashion by the same investigator to grade the osteitis. Afterward, we compared the grading of osteitis in each studied group. As seen in A, histological analysis of the ethmoid bone from control group who underwent septoplasty showed normal bone histology in 90.47% of cases, and 9.52% demonstrated grade I osteitis. In the NACRS group, 11.11% demonstrated normal bone histology, 33.33% demonstrated grade I osteitis, 50% demonstrated grade II osteitis, and 5.5% demonstrated grade III osteitis (B). In the ACRS group, 100% of patients showed osteitis: 80% were grade I and 20% were grade II (C).
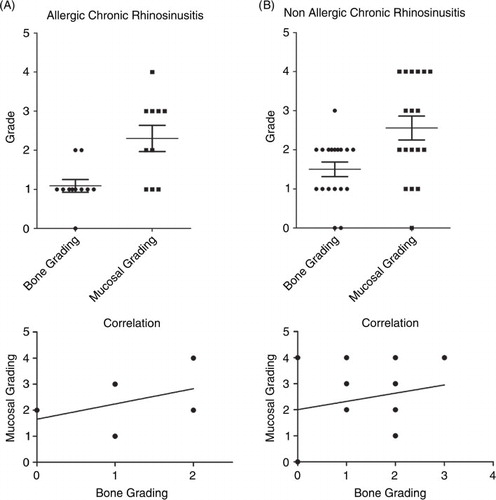
Correlation between bone and mucosal inflammation in CRS
We next investigated whether there is a correlation between the bone and mucosa grade of inflammation. In the NACRS group, the mucosal grading was as follows: 5.55% showed grade 0, 16.66% showed grade I, 27.77% showed grade II, 16.66% showed grade III, and 33.33% showed grade IV. In comparison, the ACRS group mucosal grading was as follows: 30% showed grade I, 20% showed grade II, 40% showed grade III, and 10% showed grade IV. As seen in , there was a higher grade of mucosal inflammation over bone inflammation in both CRS groups. However, there was no correlation between the grade of bone and mucosal inflammation in each studied group.
Discussion
Bone infection in sinusitis has been evident since earlier studies on animal models of severe sinusitis in rabbits that demonstrated a periosteal reaction of fibrosis, bone degradation, and neo-osteogenesis, starting as early as 4 days after sinus infection and also able to affect the contralateral side that was not infected (Citation1, Citation8–Citation10). Histomorphometric studies also demonstrated ethmoid bone remodeling in patients with CRS (Citation11). Bone remodeling involves osteoblast and osteoclast activity. The former function is to produce type I collagen and the components of the bone matrix, including calcifying the matrix and controlling the osteoclast activity. However, osteoclasts solubilize the calcified matrix, which in turn stimulates osteoblast proliferation. Therefore, disturbance of the delicate balance between the dynamics and activity of these cells that take place under normal conditions may significantly affect the process of bone remodeling. This could be seen in inflammation since inflammatory cytokines can influence osteoblast activity (Citation12).
In the current study, we investigated osteitis in two broad phenotypes of CRS, the non-allergic group that is biased to the TH1 cytokine profile and the allergic group that is biased to the TH2 cytokine profile. Herein, we demonstrated increases in osteoblastic and osteoclastic bone activity that resulted in osteitis of the ethmoid bone with its remodeling from patients with non-recalcitrant CRS. This is consistent with earlier reports that demonstrated osteitis of the ethmoid bone in CRS patients. However, we also demonstrated the first evidence that in ACRS, the ethmoid bone also undergoes remodeling. The majority of osteitis witnessed in the allergic group (80%) was in the form of periosteal thickening, and in 20% there were also increases in osteoblast and osteoclast activity with bone remodeling. Interestingly, osteitis was present in all studied patients (100%) in the allergic group. However, 88.88% from the NACRS group showed different grades of osteitis that were most striking in regard to periosteal thickening and osteoblastic and osteoclastic activity; there was bone remodeling in 50% of cases, and 5.5% also demonstrated osteoid bone that was interconnected haphazardly. We did not see any severe-grade osteitis with frank osteomyelitis and bone destruction (i.e., grade IV) in our studied groups; perhaps this is because we excluded patients with recalcitrant CRS from the current study as well as patients with allergic fungal sinusitis. Of note, in the control group, two out of the 21 studied patients showed grade I osteitis. When we reviewed their clinical picture, we found that these two patients also underwent partial inferior turbinectomy for associated chronic hypertrophic rhinitis, but no CT scans for them were available. Therefore, it is difficult to comment on their osteitis, which may be due to associated mucosal sinus changes. Another explanation may be that in nonspecific rhinitis, the underlying bone also may be involved in the inflammatory process. This requires further studies to prove or disprove.
When we compared the mucosal inflammation to bone inflammation in both CRS groups, there was higher a grade of mucosal inflammation than of bone inflammation, reflecting a higher inflammatory index in general in the NACRS group over the ACRS group. However, there was no correlation between the grade of mucosal inflammation and that of bone inflammation in each studied group. This interestingly finding may indicate that although CRS patients demonstrate mucosal and bone inflammation, the severity of inflammation between the mucous membrane and bone is not correlated, and the mucosal and bone inflammation from the NACRS group may be higher in grade than that of the ACRS group.
The definition of chronic sinusitis over the years was limited to chronic inflammation of the mucous membrane lining the paranasal sinuses. The terminology was changed recently to ‘chronic rhinosinusitis’ since the inflammatory process of the mucous membrane of the nasal cavity often also involves the paranasal sinuses. Herein, we also demonstrated the involvement of the underlying ethmoid bone in the process of inflammation that was not correlated to the mucosal inflammation. Our results together with those of previous investigators strongly point to the more appropriate definition of CRS as an inflammatory process involving the mucous membranes of the nasal cavity and paranasal sinuses and the underlying bone. This is also true for patients suffering from ACRS.
The higher osteitis grade seen in the NACRS group over the ACRS group may reflect a specific cytokine profile, since the current thinking is that CRS is biased toward the TH1 cytokine profile and allergy biased to TH2 cytokine profile. Another possible explanation of the differences in the grade of osteitis between both groups could be an extra factor such as the type and virulence of bacterial infection. This is currently under investigation in our laboratory.
In conclusion, herein we demonstrate bone remodeling in patients suffering from ACRS and confirm the bone involvement with a higher grade osteitis in CRS without allergy. These results may open channels for further research exploring the exact mechanisms by which nasal and paranasal mucosal inflammation reaches the underlying bone and how to treat osteitis in nasal and paranasal inflammation.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- Perloff JR Gannon FH Bolger WE Montone KT Orlandi R Kennedy DW . Bone involvement in sinusitis: An apparent pathway for the spread of disease. Laryngoscope. 2000;110:2095-9.
- Lee JT Kennedy DW Palmer JN Feldman M Chiu AG . The incidence of concurrent osteitis in patients with chronic rhinosinusitis: A clinicopathological study. Am J Rhinol. 2006;20:278-82.
- Kennedy DW Senior BA Gannon FH Mantone KT Hwang P Lanza DC . Histology and histomorphometry of ethmoid bone in chronic rhinosinusitis. Laryngoscope. 1998;108:502-7.
- Renato J Giacchi MD Richard A Lebowitz MD . Histopathologic evaluation of the ethmoid bone in chronic sinusitis. Am J Rhinol. 2001;15:193-7.
- Bhandarkar ND Mace JC Smith TL . The impact of osteitis on disease severity measures and quality of life outcomes in chronic rhinosinusitis. Int Forum Allergy Rhinol. 2001;1:372-8.
- Georgalas C Videler W Freling N Fokkens W . Global osteitis scoring scale and chronic rhinosinusitis: A marker of revision surgery. Clin Otolaryngol. 2010;35:455-61.
- Biedlingmaier JF Whelan P Zoarski G Rothman M . Histopathology and CT analysis of partially resected middle turbinates. Laryngoscope. 1996;106:102-4.
- Norlander T Westrin KM Stierna P . The inflammatory response of the sinus and nasal mucosa during sinusitis: Implications for research and therapy. Acta Otolaryngol Suppl. 1994;515:38-44.
- Bolger WE Leonard D Dick EJ Stierna P . Gram negative sinusitis: A bacteriologic and histologic study in rabbits. Am J Rhinol. 1997;11:15-25.
- Khaled AN Hunt J Perloff JR Kennedy DW . The role of bone in chronic rhinosinusitis. Laryngoscope. 2002;112:1951-5.
- Giacchi RJ Lebowitz RA Yee HT Light JP Jacobs JB . Histopathologic evaluation of the ethmoid bone in chronic sinusitis. Am J Rhinol. 2001;15:193-7.
- Nair SP Meghji S Wilson M Reddi K White P Henderson B . Bacterially induced bone destruction: Mechanisms and misconceptions. Infect Immun. 1996;64:2371-80. [PubMed Abstract] [PubMed CentralFull Text]