Abstract
Background: The International Network of field sites with continuous Demographic Evaluation of Populations and Their Health (INDEPTH) has 34 Health and Demographic Surveillance System (HDSS) in 17 different low and middle-income countries. Of these, 23 sites are in Africa, 10 sites are in Asia, and one in Oceania. The INDEPTH HDSS sites in Asia identified chronic non-communicable diseases (NCDs) as a neglected area of attention. As a first step, they conducted NCD risk factor surveys within nine sites in five countries. These sites are now looking to broaden the agenda of research on NCDs using the baseline data to inform policy and practice.
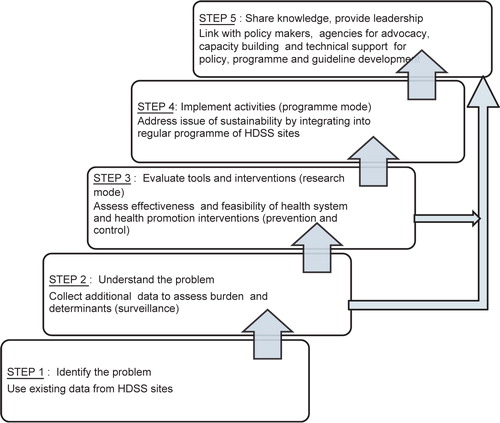
Methods: A conceptual framework for translating research into action for NCDs at INDEPTH sites was developed. This had five steps – assess the problem, understand the nature of the problem, evaluate different interventions in research mode, implement evidence-based interventions in programme mode, and finally, share knowledge and provide leadership to communities and countries. Ballabgarh HDSS site in India has successfully adopted these steps and is used as a case study to demonstrate how this progress was achieved and what factors were responsible for a successful outcome.
Results: Most of the HDSS sites are in the second step of the process of translating research to action (understand the problem). The conduct of NCD risk factor surveys has enabled an assessment of the burden of NCD risk together with determinants in order to understand the burden at the population level. The experience from Ballabgarh HDSS exemplifies that the following steps – pilot testing the interventions, implementing activities in programme mode, and finally, share knowledge and provide leadership – are also possible in rural settings in low-income countries. The critical success factors identified were involvement of a premier medical institution, pre-existing links to policy makers and programme managers, strong commitment of the HDSS team and adequate human resource capacity.
Conclusion: All INDEPTH HDSS sites now need to strengthen their links to health systems at different levels and enhance their capacity to engage different stakeholders in their respective country settings so as to translate the current knowledge into actions that can benefit the health of the population they serve and beyond.
Introduction
The World Report on Knowledge for Better Health in 2004 laid strong emphasis on translating knowledge into action to improve health, thereby bridging the gap between what is known and what is actually done Citation1. Initiatives are needed to facilitate interaction between researchers and policy makers to foster greater use of research findings and evidence in policy making and to narrow the know-do gap Citation2. Thailand's Health System Research Institute suggests the need for mediating mechanisms especially those of governments and civil society agencies Citation3. The International Network of field sites with continuous Demographic Evaluation of Populations and Their Health (INDEPTH) could be one of the potential agencies for this purpose. It is a not-for-profit organisation that currently consists of 34 Health and Demographic Surveillance System (HDSS) sites in 17 countries in Africa, Asia and Oceania Citation4. The HDSS have provided platforms for research on measles vaccines, maternal mortality, insecticide treated nets and verbal autopsies among many other important areas Citation5Citation6Citation7Citation8. INDEPTH sites focused appropriately on their national health priorities and played critical roles in their translation into policy. However, it is clear that there is a large know-do gap in the field of non-communicable disease (NCD) prevention and control in Asia where much of the focus has been on maternal and child health and infectious disease control Citation9.
The nine HDSS in Asia decided in 2004 to address the issue of NCDs as all these countries were undergoing epidemiological transition and yet very little emphasis had been placed on this neglected area. Although NCDs had not become national priority in many of these countries, there was an increasing recognition of their growing burden in the region. One of the major reasons for this lack of prioritisation was that both governments and policy makers believed that chronic NCDs are an issue only in wealthy countries and wealthy people. It was necessary to generate local evidence to dispel these myths. As a first step, the nine Asian HDSS combined their efforts in a multi-site risk factor survey using standardised materials and methods Citation10. This survey was undertaken in 2005 and completed in 2006; the results form the main content of this issue of Global Health Action.
The studies published in this supplement show wide variation in the prevalence of different risk factors among the sites and between men and women Citation11Citation12Citation13Citation14Citation15Citation16Citation17. The sex differences in measured behaviours raise socio-cultural issues. These are exemplified by high tobacco use among women in sites in Bangladesh and in Vadu, India, but not in other sites. Some differences, for example, differences observed in fruit and vegetable intake and physical activity in rural areas may be explained by different agricultural cropping patterns, mechanisation of farming, farm pricing policies, affordability and household food distribution practices. It is therefore important to place the results in the context of these factors to better understand both the level and determinants of risk factors. The levels of risk factors are also influenced by the intensity of existing NCD prevention and control programmes, which are invariably inadequate in the countries of South-east Asian Region Citation18. While data generated by these surveys assesses the current burden of risk factors, there is also a need for qualitative studies at a local level to support surveillance data in order to inform action. INDEPTH sites provide a micro system where the interplay of different determinants and factors can be studied and understood while systems are put in place to understand its complexity in the national context.
One of the INDEPTH sites, in Ballabgarh, India, has been working in the area of NCDs since the year 2000. The objective of this paper is to describe the experience of Ballabgarh HDSS in the area of NCD surveillance, prevention and control, and to discuss the potential contribution that other sites can provide in strengthening NCD prevention and control in the South-east Asian Region.
2 A framework for translating research into practice
A framework for understanding the process of translating research to action as applicable to NCDs in the INDEPTH HDSS site is shown in . This framework borrowed from frameworks developed by WHO for the role of government and a framework for translational research. The WHO stepwise framework for NCD prevention includes three planning steps – estimate population need and advocate for action, formulate and adopt policy, and identify policy implementation steps Citation19. The translational research framework used three ‘A's – Awareness, Acceptability and Application Citation9Citation20Citation21. The ‘awareness’ phase relates to the actual invention (knowledge acquisition) or discovery and its validation by other researchers. The phase of ‘acceptability’ starts when newly generated knowledge is put to practical use in clinical settings. Many translational researchers stop at this point of ‘bench to bedside’ translation. The third and crucial phase of ‘application’ addresses the issue of an accepted clinical practice being translated into a national level policy, programme or plan. In order to do so, it has to enter into the public health research agenda since health service or operational research would be needed to test the feasibility of a large-scale programme. Appropriate economic analyses and advocacy are required in this phase to convince the policy makers about its cost-effectiveness. HDSS sites could contribute greatly to overcome the barriers to the second level of translational research, i.e. ‘bedside to community’.
The framework used for this analysis comprises of five steps in an ascending manner ():
The first step is the use of existing information sources to identify a new public health problem. In the case of NCDs in HDSS sites, this includes mortality surveillance data which demonstrate that NCDs are a significant and major contributor to deaths in their population.
The second step is to develop a better understanding of the problem by undertaking additional data collection to measure changes in the burden and determinants of NCD risk factors using both quantitative (surveillance) and qualitative methods.
The third step is to evaluate the feasibility and effectiveness of different interventions related to NCDs. These are primarily in two domains – health promotion interventions directed at the whole population (prevention) and health systems interventions directed at individuals at high risk (treatment). This step requires close co-operation with the local health system and other stakeholders. The activities undertaken in a research mode provide key results to be shared with relevant stakeholders at higher levels.
In the fourth step, the activities related to NCD surveillance, prevention and control that are found to be feasible and cost-effective in research mode would be implemented in a regular routine programme mode to ensure sustainability.
In the final step, the HDSS sites share knowledge and provide leadership in their own communities, countries and region by supporting advocacy, encouraging capacity building and providing technical assistance in the development of NCD related policies, programmes and guidelines.
3 The Ballabgarh HDSS: a case study
This section traces the progress of the Ballabgarh HDSS site over the five steps listed above and draws lessons for implementation elsewhere.
The Comprehensive Rural Health Services Project (CRHSP) in Ballabgarh was started in 1965 by the All India Institute of Medical Sciences (AIIMS), New Delhi, and is situated in the state of Haryana in Northern India. The CRHSP is run in active collaboration with the State Government of Haryana. The Intensive Field Practice Area (IFPA) of the project comprises of 28 villages catering to a population of 85,552 in 2008. CRHSP Ballabgarh has been part of INDEPTH Network since 2003. Unlike most other HDSS sites, the primary responsibility of CRHSP Ballabgarh is training of medical and nursing students, as well as delivering health care services patterned on national norms.
CRHSP conducts demographic surveillance on an ongoing basis. Routine data (births, deaths, in-migration, out-migration) is collected on a monthly basis and a yearly census is also conducted in the month of December. The demographic database has been stored electronically since 1991. Every individual in the project area has been assigned a unique identification number that is present in all the files and which is used to link all the databases. The computerised database is updated and revised to accommodate the needs of the users and introduction of new national programmes. Verbal autopsy is carried out for all deaths in the area by the health workers and the cause of death is determined by the Medical Officer. This platform was used to conduct NCD surveillance, prevention and control activities at Ballabgarh. This setup is similar to other INDEPTH sites except that the managers of the site are also the health care providers for the population. Its link to AIIMS, a premier public sector medical college in India, means that there are pre-existing direct links with policy makers.
3.1 Step 1: Identify the problem
The analyses of mortality data for the years 2002–2007 show that the proportion of deaths due to NCDs among the population 15 years and over was 56% (61% of deaths in males and 52% in females); the remaining deaths were due to injury or infectious diseases; about 17% of deaths could not be classified by verbal autopsy. All INDEPTH sites generate this information on mortality using verbal autopsy tools in a regular and sustainable way and help in establishing the mortality burden of NCDs.
3.2 Step 2: Understand the problem
Qualitative and quantitative studies can be used in measuring the burden and understanding the determinants of disease. As a first step, Ballabgarh HDSS site was involved in the pilot testing of the WHO STEPwise approach to Surveillance (STEPS) (http://www.who.int/chp/steps/en/) and in the validation of the physical activity tool Citation22. Subsequently, Ballabgarh HDSS has been a part of a nationwide multicentre survey for behavioural and anthropometric NCD risk factors surveillance using the WHO STEPS methodology in 2003 that included urban, urban slum and rural areas Citation23. In 2005, in a sub-sample of the population, assessment of the biochemical risk factors (Step 3 of WHO STEPS) was also carried out. These studies provided valuable insight into the practical aspects of carrying out community-based surveillance activities, especially in Step 3 where quality assurance in handling and processing of blood samples was of utmost importance Citation24. The results of these surveys have been published and widely disseminated nationally Citation25Citation26Citation27Citation28.
A second risk factor survey was carried out in 2006 in the same population using the same WHO STEPS instrument to allow an assessment of the trend of risk factors in the absence of any active intervention. The results show that the risk factor levels are more or less stable (unpublished data). There was no specific ongoing intervention in the villages for NCD prevention and control during this time period. A third measure is required in order to determine trends in the population levels of risk; this is planned for 2010.
Most of HDSS sites have completed only the baseline or first round of risk factor surveys and will need to ensure that these are repeated in the same populations using the same methodology.
3.3 Step 3: Evaluate feasible and cost-effective interventions
As a part of the WHO's efforts to generate local evidence, Ballabgarh has been involved in the demonstration project of community-based intervention in urban Ballabgarh Citation29. One of the faculty members (SKK) went on a training visit to North Karelia for this purpose. Again, the process and results of this exercise are being disseminated and shared regularly with national and regional policy makers and programme managers. Recently this programme was evaluated and the results are in the process of being published.
Currently, Ballabgarh is also implementing a programme for management of chronic diseases under the primary health care system in rural Ballabgarh funded by the Department of Health Research, Ministry of Health and Family Welfare (MOHFW), Government of India. This ongoing research work looks at operational issues like cost and impact on workload of adding NCD work to health workers. A weekly NCD clinic was started in 2001.The experience of managing these diseases at secondary level hospital has been published Citation30. A tobacco cessation clinic has been started at the hospital with support from the National Ministry of Health and Family Welfare and WHO India. These activities demonstrate close collaboration of the site with the Central Ministry of Health.
These activities have been possible largely due to the high credibility of Ballabgarh and AIIMS as an academic institution among a spectrum of stakeholders ranging from international agencies to local community, a physical location near New Delhi (capital of India), existing links to WHO and Ministry of Health, and the presence of a good team of epidemiologists and social workers. Many of the sites in Asia have strong links to academic institutions.
3.4 Step 4: Implement activities in programme mode
Currently, Ballabgarh HDSS has integrated and included in its routine programme mode, activities related to surveillance, prevention and control. In 2002, ‘Surveillance for Demographic, Environment and Health Information (SUDEHI)’ was initiated at the HDSS with the objective of collecting information on human behaviour which predisposes the population to both common communicable diseases and NCDs, and to ascertain health care seeking behaviour. It also included questions on NCD risk factors such as tobacco use, alcohol consumption, consumption of excess fats and oils, and leisure time physical activities in the past week, mean number of days of consumption of vegetables and fruits, soft drinks, fried food, sweets and whether or not blood pressure had been measured in the last year. A comparison of the result of SUDEHI using routine health workers in surveillance mode with the result of the STEPS NCD risk factor surveys showed that similar results were obtained Citation31. This experience shows that it is possible for HDSS sites to integrate a few core elements of a larger NCD risk factor survey into its routine surveillance activities without imposing an excessive burden on the existing system, though this restricts the number of questions.
All the health system interventions (risk screening by health workers, management of the at-risk population at primary health centres and in an NCD clinic) have been integrated with the system and are currently funded by the regular budget of the site. This was largely possible because each institution is also responsible for health service delivery to the population. For other HDSS sites, this step calls for a much stronger link with the health care delivery system in their community. Similarly NCD issues, especially tobacco use, are discussed in all community-based activities.
3.5 Step 5: Share knowledge and provide leadership
The capacity of Ballabgarh to carry out NCD prevention and control activities has been strengthened over these years by its team members being formally trained (WHO STEPS methodology, community-based intervention in a community setting) as well as informally trained through involvement in planning and implementation of different NCD-related activities. Ballabgarh is now in a position to provide guidance and assistance to others. The list of extramural activities of Ballabgarh HDSS and the different partners that it works with for capacity building, advocacy and technical support, is at both national and international level as shown in . At the international level, the staff of the site was involved in the Regional STEPs training workshop for member countries of the SEA Region. One of the authors (KA) of this paper has also been involved in providing technical support to other countries of the South-east Asian region including Nepal, Maldives, Bhutan and DPR Korea. A workshop in WHO STEPS methodology was organised for participants from INDEPTH – Asia HDSS, after which NCD risk factor surveillance activities were initiated in their respective sites. The outcome of these efforts have been the conduct of multiple risk factor surveys in the countries of this region with more than 100 people being trained in the WHO STEPwise approach to NCD surveillance.
Table 1. Summary of extramural NCD prevention and control activities in Ballabgarh HDSS
At a national level, WHO in-country fellows were trained in different aspects of NCD prevention and control activities. A workshop for sensitising the state health departments and faculty from various medical colleges in NCD prevention and control activities was carried out in 2003. The team members have participated in numerous efforts to sensitise different stakeholders in NCD prevention and control. It is very difficult to quantify the outcomes of these efforts. Suffice to say, that this teams’ contribution in creating a paradigm for a shift in thinking of different stakeholders to a health agenda which is inclusive of NCDs, is well recognised. It is only because of this that formal recognition by the Government of India has come its way. Ballabgarh HDSS has been designated as a resource centre for training and monitoring the NCD surveillance component of the Integrated Disease Surveillance Project. Ballabgarh HDSS is also contributing to the National Programme for Prevention and Control of Diabetes, Cardiovascular Diseases and Stroke that was launched in India in January 2008 through technical assistance input and by providing a platform for training (http://www.mohfw.nic.in/D4.htm).
4 Lessons for other sites
This paper focuses on the activities of Ballabgarh HDSS and consequently the role that it is playing in national and international efforts to strengthen NCD prevention and control activities. Based on our experience at Ballabgarh HDSS, the possible roles that HDSS sites can play in NCD prevention and control include the following:
A demographic surveillance system provides a unique platform on which a range of health, social, economic and behavioural studies can be carried out through community-based, longitudinal follow up of populations. Ideally this is what a surveillance system requires – a system where populations can be followed up to monitor trends and identify action points for intervention. HDSS can provide a platform for carrying out surveillance of NCD risk factors to measure trends in population risk in the absence of such information at national level. A study from three INDEPTH sites (Ethiopia, Vietnam and Indonesia) has reported that combining WHO STEPS with HDSS activities can address epidemiologic questions on NCDs Citation32.
Since all HDSS conduct regular demographic surveillance activities for census purposes, the potential of including a few selected key core questions related to risk factor surveillance in the surveillance activity of the HDSS sites in a cyclical manner is innovative. This approach reduces the need for repeated separate cross-sectional surveys for NCD surveillance in HDSS sites, although some measures do require full surveys.
The HDSS sites included in this series differ in the prevalence of these risk factors that needs further exploration. These differences need to be studied in the context of differences in the stage of epidemiological transition as well as socio-cultural differences between the sites. These differences provide opportunities for understanding the social determinants of risk better so as to formulate appropriate policies. As these sites also measure socio-economic status of individuals and families, these sites can provide valuable evidence to raise the issue of equity. Reports from other INDEPTH sites, particularly in Africa, have brought out the potential of HDSS sites to measure mortality and morbidity differentials, thus addressing the issue of equity Citation33. These can be done for NCDs as well and will help in dispelling the myth that these diseases are confined to wealthy countries and wealthy people within those countries.
Because of the fact that HDSS represent different socio-cultural and national identities, they can help develop and test/validate standard tools and protocols for measurement of different NCD risk factors as has been done with physical activity and diet Citation22.
HDSS sites can be used as places for research and training of public health experts. HDSS sites attract professionals from diverse backgrounds. Highly qualified demographers, epidemiologists, sociologists, clinicians and economists enable a continuum of research and a multi-faceted examination of health problems and provide an ideal environment for training of research professionals.
HDSS sites can also spearhead involvement in planning, implementing and evaluating intervention against NCDs. Many of these sites are involved in doing the same for communicable diseases and reproductive health issues. It is only logical to take this forward to include non-communicable issues.
However, the role of HDSS sites will keep evolving as they move ahead on the road of translational research. For example, the Ballabgarh HDSS site now needs to focus on issues of quality of care/intervention and evaluation. The activities would include process evaluation of community-based intervention to economic evaluation of different interventions, assessing quality of different activities like counselling, training, etc.
5 The way forward
In order to carry out this agenda, the HDSS sites would need to address issues at multiple levels.
Sites need to strengthen their capacity to conduct research in NCDs and develop leadership skills. Currently, the capacity varies widely between the sites. While some have strength in social sciences, others have more expertise in epidemiology. Each site will have to look at the role it can play depending upon its own current strengths and limitations while working on a longer term strategy for strengthening its capacity. The network needs to identify partners who can support such capacity-building initiatives.
Secondly, in order for sites to influence policy and help translate research to action at national level, they need to improve links to national ministries of health. They need to be able to demonstrate leadership to the local and national health authorities so that national governments will be encouraged to support and invest in HDSS Citation34.
The sites also need to engage more closely with the health care delivery system of the population under surveillance.
Finally, as a part of a network, these sites can develop cross-site activities, including research proposals which build on the strengths of the network. This also takes care of capacity weaknesses at site level as one site's weakness in an area can be compensated by other site's strengths in that area. The international research agenda is shifting to large-scale multicentre studies. INDEPTH HDSS have the potential to support such research by demonstrating versatility, fresh ideas and new approaches Citation35.
6 Conclusions
In the past, HDSS sites have made significant contributions to national efforts in dealing with infectious diseases such as HIV/AIDS, malaria and maternal child health issues. These need to be expanded to cater for emerging health problems such as NCD and the risk factors which predict them. They are uniquely positioned to elucidate issues related to measuring shifts in population distribution of risk factors and measuring effectiveness of prevention programmes. They need to leverage their strengths to influence policy makers and programme managers in their own countries so as to translate the current knowledge into actions that can benefit the health of people.
7 Conflict of interest
The authors have declared no conflict of interest.
Acknowledgements
The activities carried out at Ballabgarh HDSS are as a result of active collaboration with Indian Council of Medical Research (ICMR, New Delhi and WHO Country Office and South-east Asian Regional Office and WHO, Geneva. We would like to place on record our gratitude to Dr. Bela Shah and her team in ICMR, Dr. Cherian Varghese (WHO India Office), Dr. Jerzy Leowski (WHO/SEARO) and Prof. Ruth Bonita (Auckland, New Zealand).
References
- World Health Organization. World report on knowledge for better health: strengthening health system. Geneva: World Health Organization. 2004.
- van Kammen J, de Savigny D, Sewankambo N. Using knowledge brokering to promote evidence-based policy-making: the need for support structures. Bull World Health Organ. 2006; 84: 608–12.
- Block M. Bridging the implementation gap in health systems research. Bull World Health Organ. 2004; 82: 732.
- INDEPTH Network. INDEPTH Network. Available from: www.indepth-network.org; 2009. [cited 30 July 2009].
- Aaby P, Jensen TG, Hansen HL, Kristiansen H, Tharup J, Poulsen A, et al.. Trial of high-dose Edmonston-Zagreb measles vaccine in Guinea-Bissau: protective efficacy. Lancet. 1988; 2: 809–11.
- Shahidullah M. The sisterhood method of estimating maternal mortality: the Matlab experience. Stud Fam Plann. 1995; 26: 101–6.
- Snow RW, McCabe E, Mbogo CN, Molyneux CS, Some ES, Mung'ala VO, et al.. The effect of delivery mechanisms on the uptake of bed net re-impregnation in Kilifi District, Kenya. Health Policy Plan. 1999; 14: 18–25.
- Kahn K, Tollman SM, Garenne M, Gear JSS. Validation and application of verbal autopsies in a rural area of South Africa. Trop Med Int Health. 2000; 5: 824–31.
- Krishnan A, Yadav K, Kaur M, Kumar R. Translational research: from epidemiology to pubic health intervention in preventing cardio-vascular diseases. Indian J Med Res. 2009. (in press).
- Ng N, Minh HV, Juvekar S, Razzaque A, Bich TH, Kanungsukkasem U, et al. Using the INDEPTH HDSS to build capacity for chronic non-communicable disease risk factor surveillance in low and middle-income countries. Global Health Action. Supplement 1, 2009. DOI: 10.3402/gha.v2i0.1984.
- Ng N, Hakimi M, Minh HV, Juvekar S, Razzaque A, Ashraf A, et al. Prevalence of physical inactivity in nine rural INDEPTH rural Health and Demographic Surveillance Systems in five Asian countries. Global Health Action. Supplement 1, 2009. DOI: 10.3402/gha.v2i0.1985.
- Ashraf A, Quaiyum MA, Ng N, Minh HV, Razzaque A, Ahmed SM, et al. Self-reported use of tobacco products in nine rural INDEPTH Health and Demographic Surveillance Systems in Asia. Global Health Action. Supplement 1, 2009. DOI: 10.3402/gha.v2i0.1997.
- Kanungsukkasem U, Ng N, Minh HV, Razzaque A, Ashraf A, Juvekar S, et al. Fruit and vegetable consumption in rural adults population in INDEPTH HDSS sites in Asia. Global Health Action. Supplement 1, 2009. DOI: 10.3402/gha.v2i0.1988.
- Minh HV, Soonthornthada K, Ng N, Juvekar S, Razzaque A, Ashraf A, et al. Blood pressure in adult rural INDEPTH population in Asia. Global Health Action. Supplement 1, 2009. DOI: 10.3402/gha.v2i0.2010.
- Bich TH, Nga PTQ, Quang LN, Minh HV, Ng N, Juvekar S, et al. Patterns of alcohol consumption in diverse rural populations in the Asian region. Global Health Action. Supplement 1, 2009. DOI: 10.3402/gha.v2i0.2017.
- Ahmed SM, Hadi A, Razzaque A, Ashraf A, Juvekar S, Ng N, et al. Clustering of chronic non-communicable disease risk factors among selected Asian populations: levels and determinants. Global Health Action. Supplement 1, 2009. DOI: 10.3402/gha.v2i0.1986.
- Razzaque A, Nahar L, Minh HV, Ng N, Juvekar S, Ashraf A, et al. Social factors and overweight: evidence from nine Asian INDEPTH network sites. Global Health Action Supplement 1, 2009. DOI: 10.3402/gha.v2i0.1991.
- Leowski J, Krishnan A. Capacity to control noncommunicable diseases in the countries of South-East Asia. Health Policy. 2009; 92: 43–8.
- World Health Organization. Preventing chronic diseases – a vital investment. Geneva: World Health Organization. 2005.
- Alving P. The road map ahead for clinical and translational science. Available from: http//nihroadmap.nih.gov/clinicalresearch/B10_2006_Alving.ppt; 2009. [cited 29 February 2009].
- Zerhouni EA, Alving B. Clinical and translational science awards: a framework for a national research agenda. Transl Res. 2006; 148: 4–5.
- Bull FC, Maslin T. Final report on reliability and validity of the Global Physical Activity Questionnaire (GPAQ v1). World Health Organization. Geneva, 2006
- WHO India-Indian Council of Medical Research. Report of the surveillance risk factors of non-communicable diseases (STEPS 1 and 2) from 5 centres in India. New Delhi: WHO India-Indian Council of Medical Research. 2004.
- WHO India-Indian Council of Medical Research. Sentinel health monitoring centres in India: report of the biochemical risk factor survey for non-communicable diseases. New Delhi: WHO India-Indian Council of Medical Research. 2006.
- Anand K, Shah B, Lal V, Shukla DK, Paul E, Kapoor SK. Prevalence of risk factors for non-communicable disease in a rural area of Faridabad district of Haryana. Indian J Public Health. 2008; 52: 117–24.
- Anand K, Shah B, Gupta V, Khaparde K, Pau E, Menon GR, et al.. Risk factors for non-communicable disease in urban Haryana: a study using the STEPS approach. Indian Heart J. 2008; 60: 9–18.
- Anand K, Shah B, Yadav K, Singh R, Mathur P, Paul E, et al.. Are the urban poor vulnerable to non-communicable diseases? A survey of risk factors for non-communicable diseases in urban slums of Faridabad. Natl Med J India. 2007; 20: 115–20.
- Nongkynrih B, Acharya A, Ramakrishnan L, Ritvik A, Anand K, Shah B. Profile of biochemical risk factors for non communicable diseases in urban, rural and periurban Haryana, India. J Assoc Physicians India. 2008; 56: 165–70.
- Anand K, Pandav CS, Kapoor SK, Leowski J. Integrated community based intervention against the risk factors for NCDs – early lessons from the demonstration project undertaken at Ballabgarh, India. Regional Health Forum WHO SEAR. 2006; 10: 11–21.
- Patra S, Baridalyne N, Anand K. Managing noncommunicable diseases at a secondary level. J Assoc Physicians India. 2009; 57: 83.
- Nongkynrih B, Krishnan A, Pandav CS, Kapoor SK. Feasibility and validity of introducing regular behavioural surveillance into the health system in India. Natl Med J India. 2009. (in press).
- Ng N, Minh HV, Tesfaye F, Bonita R, Byass P, Stenlund H, et al.. Combining risk factors and demographic surveillance: potentials of WHO STEPS and INDEPTH methodologies for assessing epidemiological transition. Scand J Public Health. 2006; 34: 199–208.
- Ngom P, Binka FN, Phillips JF, Pence B, Macleod B. Demographic surveillance and health equity in sub-Saharan Africa. Health Policy Plan. 2001; 16: 337–44.
- Chandramohan D, Shibuya K, Setel P, Cairncross S, Lopez AD, Murray CJ, et al.. Should data from demographic surveillance systems be made more widely available to researchers?. PLoS Med. 2008; 5: e57.
- Baiden F, Hodgson A, Binka FN. Demographic surveillance sites and emerging challenges in international health. Bull World Health Organ. 2006; 84: 163.