Abstract
Despite a growing awareness of Africans’ vulnerability to climate change, there is relatively little empirical evidence published about the effects of climate on population health in Africa. This review brings together some of the generalised predictions about the potential continent-wide effects of climate change with examples of the relatively few locally documented population studies in which climate change and health interact. Although ecologically determined diseases such as malaria are obvious candidates for susceptibility to climate change, wider health effects also need to be considered, particularly among populations where adequacy of food and water supplies may already be marginal.
Introduction
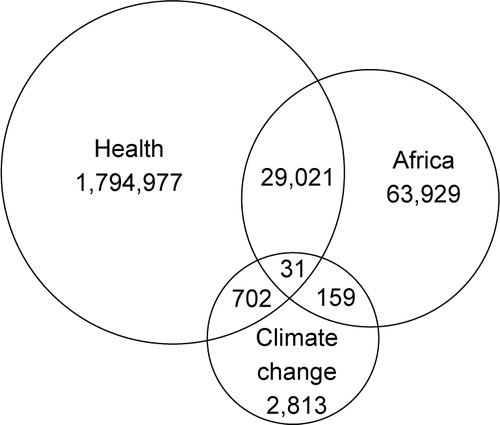
Despite increasing media coverage around the theme of African peoples’ potential vulnerability to actual and predicted changes in climate at the global level, detailed scientific evidence remains scanty. Much existing work has looked at the effects of climate on specific diseases, without making clear connections to overall changes in population health. A simple search of the PubMed database, undertaken on 26 June 2009, using the keywords ‘health’, ‘Africa’ and ‘climate change’, revealed the number of hits shown in . Despite almost two million scientific citations matching one or another of these terms, the intersection between all three contained a mere 31 citations (0.002%), some of which were brief comments or related to veterinary health. Even though this was a somewhat simplistic search, deliberately intended not to include disease-specific studies which did not explore more general implications for population health, the paucity of results in the intersection is striking. Nevertheless, the oldest of these 31 citations was published as far back as 1991 Citation1 and one therefore has to ask questions about what has or has not happened in terms of progressing the scientific understanding of climate change and population health in Africa over the past two decades.
Figure 1. Results of a PubMed search for ‘health’, ‘Africa’ and ‘climate change’ (26 June 2009) showing the intersections between the three terms (total citations 1,891,632).
The aim of this review article is to highlight some of the important points that emerge from the relatively scant literature on climate change and health in Africa, with a view to both identifying some of the key issues that have been documented and revealing some of the possible gaps where further scientific research is urgently needed.
The literature on climate change and health in Africa
Ramin and McMichael Citation2, acknowledging the paucity of evidence-based results, present five hypothetical case studies illustrating what they believe to be the major issues. These are concerned with the interaction between HIV and rain-fed food production capacity; impact of drought on child nutrition; disease impact of floods; changing patterns of malaria transmission; and the impact of natural disasters. However, these but serve as examples of scenarios which are all too rarely documented in detail with a basis in reliable data.
Much more attention has been given to global and regional estimates, using multiple data sources and models, of possible changes in climate and, in some cases, their potential health consequences. The Stern Report Citation3 paints a gloomy picture for Africa, concluding that ‘The poorest will be hit earliest and most severely. In many developing countries, even small amounts of warming will lead to declines in agricultural production because crops are already close to critical temperature thresholds. The human consequences will be most serious and widespread in sub-Saharan Africa, where millions more will die from malnutrition, diarrhoea, malaria and dengue fever, unless effective control measures are in place’. This is also reflected in the recent UCL Lancet Commission report Citation4, which suggests that the highest regional burden of climate change is likely to be borne by sub-Saharan Africa, with 34% of the global disability adjusted life years (DALYs) attributable to climate change located there. Since sub-Saharan Africa only contains 11% of the world's population Citation5, this reflects a three-fold population-based risk for adverse effects of climate change among Africans compared with the global population.
A review of likely impacts of climate change on food insecurity Citation6 concludes that current estimates of climate change will probably lead to greater risk of hunger, particularly in Africa, but without going on to consider the likely population health impacts of such hunger. Changes in land use, either forced by climate change or in response to environmental pressures, may also impact on food security Citation7. Infectious diseases tend to be considered first when contemplating the effects of climate change on health Citation1, but these may not be the only or even the major factor; impacts such as the physiological effects of heat may be equally important Citation8, particularly on the African continent where large proportions of people are regularly exposed to extremes of high temperature.
A review of cholera seasonality globally from 1974 to 2005 Citation9 suggests that climate change may well lead to less predictable patterns of cholera outbreaks; within Africa this is likely to be seen more in northern and western areas rather than in the equatorial zone. Detailed analyses of diarrhoeal disease patterns in Benin Citation10 have established expected relationships between risks of diarrhoea and lack of good-quality water supplies. These authors go on to suggest that the consequences of future climate change scenarios, leading to large-scale population displacements, may be predicated on resource considerations, such as water supply, at migratory destinations.
Whilst changes in climate may have impacts on distributions of vector-borne diseases as a direct consequence of ecological pressure on vectors, it is also important to take into account changes in host factors, such as exposure and immunity, in considering health consequences Citation11. Furthermore, the disease manifestations of longer-term epidemiological changes driven by climate may be masked by adaptational mechanisms in human populations Citation12.
Malaria is probably the most documented single disease in relation to climate change. Part of this seems to derive from concerns that the global range of malaria may be extended as territories outside current endemic zones become wetter and warmer, rather than concerns about Africa per se, even if these concerns may in some cases have been overstated Citation13. Detailed climatic analyses suggest that patterns of malaria transmission in Africa may well change as a result of climate changes Citation14. These changes are modulated by altitude, and the interactions between climate, altitude and vector behaviour Citation15. The general notion that climate is changing, alongside observations of changes in malaria disease patterns, do not, however, necessarily constitute a cause and effect relationship between climate change and malaria Citation16. The importance of carrying through climate modelling into vector dynamics modelling has been stressed Citation17. Some predictions suggest that the main effect of climate change on malaria in Africa will be geographic shifts of transmission within the continent, rather than overall changes Citation18.
Examples of local impacts on overall population health in Africa as a consequence of climate change are relatively rare, not least because of the relative scarcity of detailed health data from the African continent in the first place Citation19. After a series of debilitating rainfall failures in northern Ethiopia, a microdam construction programme was initiated in the 1990s to harvest rain water. As well as being a response to climate variability, these new reservoirs generated their own microclimates, often including nearby villages and one consequence was a seven-fold increase in childhood malaria incidence near the dams Citation20. In one district of Burkina Faso, detailed connections have been made between temperature, rainfall, mosquitoes and malaria, resulting in a local-level model relating climate to malaria transmission Citation21. In central Ethiopia, links have been made between erratic seasonal patterns of rainfall and disease epidemics which gave rise to a 2.5-fold increase in local overall population mortality over a two-year period Citation22.
Discussion
Scientific evidence connecting climate change and population health in Africa remains scanty, both because of the lack of clear understanding of the progress and nature of climate change, and the widespread lack of community-based health data. By contrast, the heatwave experienced in western Europe in 2003 was immediately identified as an unusual meteorological event and shortly afterwards analyses of resultant excess mortality were available, using data from routine systems Citation23.
Although the dominance of malaria in the literature linking climate change and health in Africa might lead one to suppose that it is the major issue, in fact other effects that are relatively under-documented may turn out to have numerically greater impacts as time passes. It may simply be the case that malaria has been the most researched issue in relation to climate thus far. However, if predictions of changing epidemic patterns of malaria within Africa are borne out Citation18, then the effects of new or increased endemicity among relatively less-immune populations could be severe, affecting all sectors within populations.
Apart from situations where interventions for other purposes facilitate the investigation of climate impacts (such as the Ethiopian microdams Citation20), most research into the effects of climate change on population health has to essentially follow a process of making retrospective connections between meteorological data and health outcomes. Population groups cannot be randomised to different kinds of natural climate change, and hence drawing causal inferences between observed climatic variations and disease patterns is difficult to achieve with certainty. Settings where prospective longitudinal population surveillance is in place, such as Indepth Network sites Citation24, are likely to be particularly valuable for analysing the population effects of climate change in Africa, since it is usually too late to collect health outcome data once a particular climate phenomenon has been observed. Routine collection of meteorological data at such sites should be regarded as normative in the current era of climate change, as well as routinely geo-referencing population health data in order to make connections with external meteorological data Citation25. Even within such surveillance sites, prompt routine review procedures for incoming data are very important if major health-related events at the population level that might be climate-linked are to be spotted promptly Citation26.
Perhaps the lack of potential for experimental study design in relating climate change to health in Africa, as well as the practical difficulties of obtaining the necessary data, have led to the relative lack of detailed scientific output in the intersection between health and climate change in Africa. The relatively weak research infrastructure in many African settings is a contributory problem, but, more importantly, cross-disciplinary work (between climatology and health in this instance) is not common in Africa and needs to be actively promoted. Expertise in applying global climate models regionally is very scarce in Africa Citation27, against the inevitable background of the world's most sophisticated climatological research centres being northern-based. Thus stronger links and capacity-building collaborations need to be forged between these global resources in the North and African health and climate research groups, if meaningful and useful scientific connections are going be made between climate change and health in Africa.
Despite the dearth of research on the ground in Africa so far, it seems clear from major global-level considerations of climate change and their possible effects on population health Citation3Citation4 that, yet again, Africa and her people stand to come out worst from the likely changes in the world's weather patterns. This has to be seen against a background of food and water security which is already at marginal levels in many places. This therefore constitutes a major challenge to governments in terms of future policy-making, and hence to universities and other research centres for generating the necessary evidence base. Thus there are compelling reasons to promote and facilitate good quality and detailed research on climate change and population health in Africa, in much larger quantities than heretofore.
Conflict of interest and funding
The author has not received any funding or benefits from industry to conduct this study.
Acknowledgements
This work was undertaken at the Umeå Centre for Global Health Research, funded by FAS, the Swedish Council for Working Life and Social Research (Grant No. 2006-1512).
References
- Shope R. Global climate change and infectious diseases. Environ Health Perspect. 1991; 96: 171–4.
- Ramin BM, McMichael AJ. Climate change and health in sub-Saharan Africa: a case-based perspective. EcoHealth. 2009. DOI: 10.1007/s10393-009-0222-4.
- Stern N. The economics of climate change. CambridgeUK: Cambridge University Press. Available from: http://www.hm-treasury.gov.uk/independent_reviews/stern_review_economics_climate_change/sternreview_index.cfm; 2007. [cited 1 August 2009].
- Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al.. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet. 2009; 373: 1693–733.
- Unicef. The state of the world's children 2007. New York: Unicef. Available from: http://www.unicef.org/publications/files/The_State_of_the_Worlds__Children__2007_e.pdf; 2006. [cited 1 August 2009].
- Parry M, Rosenzweig C, Livermore M. Climate change, global food supply and risk of hunger. Philos Trans R Soc B. 2005; 360: 2125–38.
- Patz JA, Olson SH, Uejio C, Gibbs HK. Disease emergence from global climate and land use change. Med Clin North Am. 2008; 92: 1473–91.
- Kjellstrom T. Climate change, direct heat exposure, health and well-being in low and middle-income countries. Global Health Action. 2009. DOI: 10.3402/gha.v2i0.1958.
- Emch M, Feldacker C, Islam MS, Ali M. Seasonality of cholera from 1974 to 2005: a review of global patterns. Int J Health Geogr. 2009; 7: 31.
- Pande S, Keyzer M, Arouna A, Sonneveld BJGS. Addressing diarrhea prevalence in the West African middle belt: social and geographic dimensions in a case study for Benin. Int J Health Geogr. 2008; 7: 17.
- Patz JA, Reisen WK. Immunology, climate change and vector-borne diseases. Trends Immunol. 2001; 22: 171–2.
- Githeko AK, Lindsay SW, Confalonieri UE, Patz JA. Climate change and vector-borne diseases: a regional analysis. Bull World Health Organ. 2000; 78: 1136–47.
- Rogers DJ, Randolph SE. The global spread of malaria in a future, warmer world. Science. 2000; 289: 1763–6.
- Tanser FC, Sharp B, le Sueur D. Potential effect of climate change on malaria transmission in Africa. Lancet. 2003; 362: 1792–8.
- Lindsay SW, Martens WJM. Malaria in the African highlands: past, present and future. Bull World Health Organ. 1996; 76: 33–45.
- Hay SI, Cox J, Rogers DJ, Randolph SE, Stern DI, Shanks GD, et al.. Climate change and the resurgence of malaria in the East African highlands. Nature. 2002; 415: 905–9.
- Pascual M, Ahumuda JA, Chaves LF, Rodo X, Bouma M. Malaria resurgence in the East African highlands: temperature trends revisited. Proc Natl Acad Sci. 2006; 103: 5829–34.
- Peterson AT. Shifting suitability for malaria vectors across Africa with warming climates. BMC Infect Dis. 2009; 9: 59.
- Byass P. The unequal world of health data. PLoS Med2009. , in press.
- Ghebreyesus TA, Haile M, Witten KH, Getachew A, Yohannes AM, Yohannes M, et al.. Incidence of malaria among children living near dams in northern Ethiopia: community-based incidence survey. BMJ. 1999; 319: 663–6.
- Yé Y, Sankoh OA, Kouyaté B, Sauerborn R. Environmental factors and malaria transmission risk: modelling the risk in a holoendemic area of Burkina Faso. Ashgate. SurreyUK, 2008
- Emmelin A, Fantahun M, Berhane Y, Wall S, Byass P. Vulnerability to episodes of extreme weather: Butajira, Ethiopia, 1998–1999. Global Health Action. 2008. DOI: 10.3402/gha.v1i0.1829.
- Conti S, Meli P, Minelli G, Solimini R, Toccaceli V, Vichi M, et al.. Epidemiologic study of mortality during the summer 2003 heat wave in Italy. Environ Res. 2005; 98: 390–99.
- Evans T, AbouZahr C. INDEPTH @ 10: celebrate the past and illuminate the future. Global Health Action. 2008. DOI: 10.3402/gha.v1i0.1899.
- Aron JL. Barriers to use of geospatial data for adaptation to climate change and variability: case studies in public health. Geosp Health. 2006; 1: 11–6.
- Fottrell E, Byass P. Identifying humanitarian crises in population surveillance field sites: simple procedures and ethical imperatives. Public Health. 2009; 123: 151–5.
- Pierce DW, Barnett TP, Santer BD, Glecker PJ. Selecting global climate models for regional climate change studies. Proc Natl Acad Sci. 2009; 106: 8441–6.