Abstract
Background : The WHO estimates that more than 80% of African populations attend traditional healers for health reasons and that 40%–60% of these have some kind of mental illness. However, little is known about the profiles and outcome of this traditional approach to treatment.
Objective : The purpose of this study was to describe the profiles and outcome of traditional healing practices for severe mental illnesses in Jinja and Iganga districts in the Busoga region of Eastern Uganda.
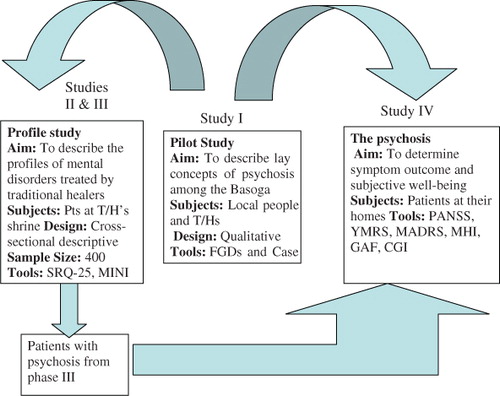
Methods : Four studies were conducted. Study I used focus group discussions (FGDs) with case vignettes with local community members and traditional healers to explore the lay concepts of psychosis. Studies II and III concerned a cross-sectional survey of patients above 18 years at the traditional healer's shrines and study IV was made on a prospective cohort of patients diagnosed with psychosis in study III. Manual content analysis was used in study I; quantitative data in studies II, III, and IV were analyzed at univariate, bivariate, and multivariate levels to determine the association between psychological distress and socio-demographic factors; for study IV, factors associated with outcome were analyzed. One-way ANOVA for independent samples was the analysis used in Study IV.
Results : The community gave indigenous names to psychoses (mania, schizophrenia, and psychotic depression) and had multiple explanatory models for them. Thus multiple solutions for these problems were sought. Of the 387 respondents, the prevalence of psychological distress was 65.1%, where 60.2% had diagnosable current mental illness, and 16.3% had had one disorder in their lifetime. Over 80% of patients with psychosis used both biomedical and traditional healing systems. Those who combined these two systems seemed to have a better outcome. All the symptom scales showed a percentage reduction of more than 20% at the 3- and 6-month follow-ups.
Conclusion : Traditional healers shoulder a large burden of care of patients with mental health problems. This calls for all those who share the goal of improving the mental health of individuals to engage with traditional healers.
Introduction:
Traditional Healing/Medicine
This article has been commented on by Vikram Patel. Please follow this link http://www.globalhealthaction.net/index.php/gha/article/view/7956 to read his commentary
Traditional healing/medicine is the sum total of knowledge, skills, and practices based on the theories, beliefs, and experiences indigenous to different cultures that are used to maintain health, as well as to prevent, diagnose, improve, or treat physical and mental illnesses Citation1. When traditional healing/medicine is adopted by other populations outside its indigenous culture, it is often termed complementary or alternative medicine Citation1. The rapid growth and acknowledgement of complementary and alternative medicine (CAM) is evident all over the world. In high income countries, an increasing number of patients are seeking out CAM practitioners for mental health care Citation1 Citation2. Studies done in these countries report that the use of CAM approaches among individuals who meet the Diagnostic and Statistical Manual Fourth Edition (DSM–IV) criteria for some psychiatric disorder is significantly greater than in the general population Citation1 Citation3. In Africa, traditional healing is part and parcel of African traditional beliefs Citation4 Citation5. People there have close relationships with traditional healers, who often share the same community and culture. A number of centers have assessed the role of traditional healers in mental health interventions. A common finding was that traditional healers could recognize symptoms of severe illness but that they expressed strong belief in supernatural factors as ultimate causes of mental illness and this influenced the treatments they gave Citation6. There is documented literature to the fact that traditional healers are effective in the milieu in which they operate Citation7 Citation8. Kleinman and Sung reported that 10 of the 12 cases treated by traditional healers rated themselves as cured. According to these researchers, similar belief systems about health and illness and the healers’ holistic approach explained the subjective improvement Citation9. Despite these positive reports, a number of arguments have been put forward against traditional healing. Some authors have dismissed traditional healing as unhealthy and dangerous, as belonging to precivilization and is open to a wide range of magical or mystical explanations Citation10 Citation11. For most western-trained practitioners, explanations of illness that fall outside the laws of natural science are pseudoscientific, primitive and simply wrong Citation11 Citation12. Claims such as these have created a lot of doubt in the minds of people about traditional healing. Indeed, it is often claimed that some of the practices can actually be harmful to the patients. The Ugandan News papers have often reported and brought into limelight some of the unethical dangerous behavior relating to treatment of patients by traditional healers Citation13. These stories may have contributed to a negative feeling about all traditional healers and all their healing practices. The church has also maligned traditional healers and often relegates traditional healing to Satanism – only fit to be condemned.
In Uganda, there is no law governing the operation of traditional healers. The only law (which is outdated) is the Witchcraft Act of 1964, which only stipulates penalties against intended acts of harm Citation14. The recent wave of ritual murders, including child sacrifice, has prompted Ugandan Parliamentarians to debate and plead with the government to enact a law regulating the activities and practices of traditional healers and herbalists. In this debate, they noted that there is no institutionalized framework for governing traditional healers Citation15.
A number of organizations register and represent traditional healers, though some traditional healers prefer not to be registered for various reasons, such as fear of taxation, etc. Recently, the Inspector General of Police of Uganda directed all traditional healers in the country to surrender their licenses for fresh registration, advising them to have one president of their association as opposed to the many at present Citation16. Assessing the exact number of traditional healers in Uganda and their utilization is challenging, as some healers are not registered and some of their clients visit them at night or clandestinely. However, it was recently estimated that there is at least one traditional healer for every village and four out of five Ugandans visit traditional healers, particularly in rural areas Citation17. The WHO estimates that 60%–80% of the population go to traditional healers for their health care needs Citation2, suggesting a massive consumer base. Many of these consultations are carried out at the same time as the patient may be receiving care from the modern health care system Citation6.
Studies investigating traditional healing as practiced in various indigenous African communities have been carried out. Most of them emphasize the psychological relevance of traditional healers in African communities Citation18–Citation20. However, hardly any comparable studies have focused on the effectiveness of traditional healing of serious mental illnesses. It is against this background that the aims and objectives of the present study have evolved.
Global burden of mental illness, treatment gap, and global mental health
Mental disorders contribute about 14% of the global burden of disease. Neuro-psychiatric conditions including disorders such as schizophrenia, mood disorders, substance abuse, and dementia are the number one contributor to the worldwide burden of non-communicable disease. In sub-Saharan Africa, mental disorders account for nearly 10% of the total burden of disease Citation21 Citation22.
In Uganda, the bulk of epidemiological research has focused on primary care settings, where most psychiatric disorders are non-psychotic Citation23. The reported prevalence rates vary widely from 10% to nearly half of all primary care attendees with a psychiatric problem with or without a co-existing physical problem with the commonest diagnoses being depression and anxiety Citation23. In a study of households in the Kabarole district in Uganda, Kasoro and coworkers found 30.7% of adults had psychiatric disorders Citation24. None of these Ugandan studies specifically addressed traditional healers’ practices, neither did they emphasize severe psychiatric illnesses (psychosis); they concentrated on common mental disorders. There is thus a paucity of literature on prevalence studies in mental health done in traditional healer centers/shrines.
Despite the staggering burden of mental illness, the treatment gap is wide. A large proportion of people with mental health problems do not receive treatment and care from a western health facility. A multicenter survey by World Health Organization (WHO) showed that 76%–85% of people with serious mental health problems had received no treatment in the previous 12 months and that for those who did receive treatment this was most often inadequate Citation25.
This gap in care is more pronounced in low- and middle-income countries, where fundamental resources are less accessible or unavailable Citation26. It is also increased by the inefficient appropriation of resources Citation26. Much of the research linking allocation of resources to outcomes of care has taken place in high-income countries. In developing countries including Uganda where 60%–80% of the population goes to traditional healers Citation2, hardly any resources are allocated to alternative providers of mental health care and there are yet no outcome studies.
Recommendations to strengthen mental health systems around the world were first mentioned in the World Health Report 2001, which focused on mental health Citation27. The current global mental health movement puts emphasis on evidence about cost-effective interventions to provide better mental health care in order to narrow or close the treatment gap Citation25 Citation26 Citation28.
The overall aim of the field of global mental health is to strengthen mental health all over the world by providing information about the mental health situation in all countries and identifying mental health needs in order to develop cost-effective interventions to meet those specific needs. The current global mental health documents make hardly any mention of traditional healing as a resource to close the treatment gap. This could have to do with the emphasis on evidence for interventions; such evidence is scarce for traditional healing.
Psychosis and traditional healers
Mainstream psychiatry considers psychosis to be a symptom of severe mental illness but not a diagnosis in itself. Psychosis is particularly associated with schizophrenia, bipolar disorder, and severe depression. This study took schizophrenia, mania, and psychotic depression as primary psychotic illnesses and defined psychosis in terms of delusions, hallucinations, and disorganized behavior Citation29.
A few studies have shown that some traditional healers in Africa, for example the Yoruba native healers, use both etiological and symptom logical concepts, mostly interchangeably, to describe psychotic illness. Their most common diagnostic label is ‘were,’ which refers to one who is chronically psychotic, careless in dressing, vagrant in behavior, talks irrationally, and suffers auditory and visual hallucinations. Most chronic cases, and perhaps individuals with symptoms of acute schizophrenia, would fall into this category Citation30. While ‘were’ denotes chronic psychosis in Yoruba, in Buganda the equivalent seems to be ‘akazoole’ and ‘eddalu’ violent madness Citation31. Okello and Musisi have demonstrated that psychotic depression is recognized and labeled as clan illness, translated as ‘ebyekika’ illness by the Baganda and their traditional healers Citation4. The implication here is that Africans and their traditional healers can identify specific mental illnesses and ascribe treatment to them. This is not dissimilar to western medicine.
The traditional healers treat psychosis with various methods that include herbs, appeasing the spirits and divination depending on the perceived cause. Prince identified Rauwolfia vomitoria as one of the psychoactive drugs used by Nigerian native healers in the treatment of psychosis Citation32.
Theoretical framework
This study explored lay concepts of psychosis among people in the study area and investigated the profiles and treatment outcomes of traditional healing practices for severe mental illnesses as measured by standard instruments. The study therefore drew ideas from various models of health care. Some of the models are explained next.
Kleinman's explanatory model of illness framework
Explanatory models of illness influence health seeking behavior and health service utilization Citation33. Kleinman asserts that healing cannot be talked about in the abstract; it must be anchored in particular social and cultural contexts. In each society, there are beliefs about illness, choices of treatment alternatives, sick and practitioner roles, and health care-related institutions organized as a cultural system Citation34.
The explanatory model has not been influential on routine psychiatric practice Citation35. Some anthropologists argue that given the incomplete understanding of mental illnesses by the scientific community, it is not clear whether the explanatory models alone are able to capture the complex mental health needs of patients across cultures Citation35.
Biopsychosocial model
The biopsychosocial model is a general model or approach that posits that biological, psychological (entailing thoughts, emotions, and behaviors), and social factors all play a significant role in human functioning in the context of disease or illness Citation36. Health is best understood in terms of a combination of biological, psychological, and social factors rather than purely in biological terms Citation36. According to the biopsychosocial model, factors that potentially influence any health outcome exist at many levels of organization, and scientific scrutiny is required at all those levels to detect which factors indeed play a significant role. The biopsychosocial model as described by Engel has been criticized by Richter Citation37 who argued that this model cannot depict the system of psychiatric care and its related problems faithfully. Although it is generally acknowledged that psychiatry should orientate toward the biopsychosocial paradigm, in practice, real changes toward this model cannot be found because the biological approach in etiology and treatment has become more and more important in recent decades Citation37.
Holistic model
This model combines many health modalities and models of health care with the goal of helping the patient or client achieve optimal physical, mental, emotional, social, and spiritual health Citation38. The ultimate goal of holistic medicine is to use all the available diagnostic and treatment modalities to optimize the health of the person on all levels of well-being, without doing harm to the person. The premise of holistic medicine is to attempt to treat the patient as opposed to the illness. Traditional healing and complementary and alternative medicine (CAM) use the holistic approach or model to health care. However, some critiques of this model argue that not all components of traditional healing and CAM are holistic Citation38. In this regard, no single model of health care is capable of meeting the entire range of human needs at the time of illness and disease Citation39. Hence the need for this thesis is to be based on all the three models in order to achieve a comprehensive view.
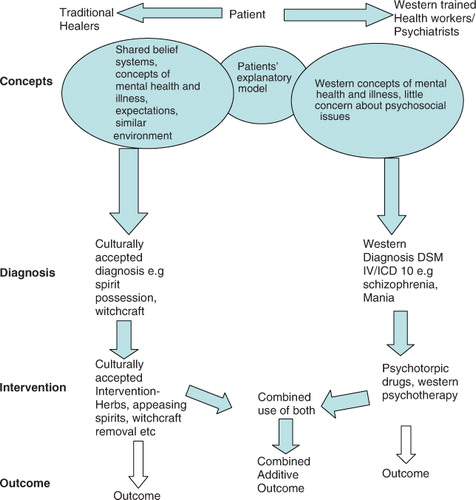
The objectives of these studies were to document the lay concepts of psychosis, describe the psychological distress and associated factors of the attendees of traditional healing practices; the prevalence and severity of mental disorders treated by traditional healers, and lastly evaluate naturalistic outcome of treatment of psychotic disorders by traditional healers in the Jinja and Iganga districts. describes the concepetual framework used in this study.
Study methods
Study area, context, and setting
These studies were carried out in two districts of Uganda, namely Jinja and Iganga. These districts are in the Busoga region, which is situated in the south-eastern part of Uganda with a population of three million and an area of 7,100 square miles Citation40. The Basoga are the eastern neighbors of the Baganda. The setting was the shrine. Traditional healers (T/H) have their place of practice within the community. It is usually separate from their place of abode but nearby or within the compound. This place of practice or shrine is often a grass-thatched hut (illustrated on the cover). It is in these huts that clients who are admitted are hospitalized. Inside the shrines, the floor is usually covered with mats (mikeeka). In one corner there may be containers of medicines in the form of dried leaves, roots, and bark of trees of varying texture, animal skins, dried animal meat, bark cloth, or animal or mineral matter such as certain clays or natural salts, and so on.
The healers usually sit on bark cloth or skin. In front of them are the ‘diagnostic’ tools, which included cowrie shells, beads, or sticks wrapped in bark cloth and put in a basket. Some shrines may have a curtain of bark cloth that separates the sleeping or resting area from the working area. The study area, context, and setting have been detailed in other papers Citation41 Citation42.
Health care services in the Jinja and Iganga districts
Jinja district has 36 government dispensaries (Health Centre II), 13 Health Centers III at county level, 4 Health Centers IV at sub-district level, and 1 hospital. In addition, there are 9 private/NGO (non-governmental organizations) dispensaries, 26 clinics and 3 Health Centers III, and 1 private hospital. Jinja Hospital has 443 beds and Kakira Hospital has 100 beds. In terms of mental health services, there is one psychiatrist and nine psychiatric clinical officers.
Iganga district has 43 government dispensaries (Health Centers II), 20 Health Centers III at county level, 4 Health Centers IV at sub-district level, and 1 hospital. In addition, there are 26 private/NGO dispensaries, 31 clinics, and 1 Health Center III. The Government District Hospital has 117 beds and the Uganda Catholic Medical Bureau-St Francis, Buluba has 164 beds. In terms of mental health services, there is one psychiatric clinical officer.
Data collection methods
summarises the study methods employed. Both qualitative and quantitative methods were used. To elicit lay concepts of psychosis in local community, focus group discussions using case vignettes were employed. For studies II and III, cross-sectional surveys were carried out to determine the magnitude of and factors associated with psychological distress and other mental illnesses. To determine the outcome of treatment of psychosis by traditional healers, a prospective cohort study was carried out. Details of the methods follow.
Focus group discussion
Focus group discussion was chosen as a useful tool for exploring topics connected with group norms and the group meanings that underlie those norms Citation43. Focus groups generate alternative views on an issue and the intention is not to reach consensus. Focus group discussion does not require formal training of moderators and observers but the literature does recommend interpersonal skills Citation43. An advantage of using the focus group discussion (FGD) to collect original data is the connection with oral traditions, which makes it preferable when participants have little or no educational background. Further, focus group discussion is relatively easy to arrange, inexpensive, and flexible in terms of format, types of question, and desired outcomes.
Surveys
In studies II and III, cross-sectional surveys were conducted in patients aged 18 years and above attending traditional healing practices. In these studies, patients who attended traditional healing practices in the Jinja and Iganga districts between January and March 2008 were consecutively recruited and screened using the Self-Reporting Questionnaire (SRQ-25). This was estimated with the Kish formula for single proportions for descriptive study Citation44. The sample size was determined assuming a prevalence of 48% for psychological distress at the traditional healer's facility Citation45. On the basis of this assumption, at a 95% confidence interval with a 5% level of precision, a total of 400 clients were consecutively recruited. The level of significance was set at p<0.05. Those who had a cutoff point of 6 and above for the first 20 questions and/or any ‘yes’ answer to any of the 4 questions that screen for psychosis were administered the diagnostic instrument, the Mini International Neuropsychiatric Interview (MINI plus) to make specific diagnosis.
In study IV, patients who had been screened using SRQ-25 and had been diagnosed using MINI as having psychosis (schizophrenia, mania, or psychotic depression) in study III were subjected to the respective instrument to measure severity (clinical outcome); that is, the positive and negative syndrome scale (PANSS) for schizophrenia, the Young Mania Rating Scale (YMRS) for mania, and the Montgomery-Asberg Depression Rating Scale (MADRS) for depression. In addition, the global assessment of functioning (GAF) was used to measure general severity (functional outcome).
Subjective well-being was also measured, using the COMPASS Mental Health Index. Objective improvement was assessed using the clinical global impression (CGI). Only patients diagnosed with psychosis were to be followed up and previous studies had estimated that about 60% of patients who go to traditional healers have psychosis Citation46. Thus it was estimated that 132 patients, including loss to follow-up, would be followed up. All the instruments were translated in the local language of Lusoga and back translated, modified accordingly, and adapted.
Sampling of traditional healers
All traditional healers who could be reached in the two districts were included in the study. The number of patients per traditional healer per district was worked out proportionately. According to the register, at the time of the study there were 180 traditional healers in Jinja district and 60 in Iganga district. This gave the following calculation:
Number of patients per traditional healer:
Therefore, at least two patients per traditional healer in each district were assessed.
Data collection procedure
The research assistants were psychiatric clinical officers who work in Jinja and Iganga district health units and the hospitals. They are clinical officers with sufficient knowledge and training to make a psychiatric diagnosis using the MINI plus. After making a diagnosis of psychosis, they administered the severity questionnaire, depending on the type of psychosis and detailed contact with the patient including telephone contact, and the Local Council Chaipersons at village level (L.C I) chairperson in the area. Appointments for follow-ups were then made for visits in the patient's home at 3 months and at 6 months.
Data management
Qualitative data for study I
Data were tape recorded and supplemented with field notes. Tape-recording allowed us to get details and accuracy that would not be available from either field notes or memory. Tape-recording also allowed more eye contact between the moderator and the respondent. Although tape-recording was important for us, it did not prevent us from getting the non-verbal communication that could not be tape-recorded Citation47.
Interviews were transcribed in accordance with guidelines for handling qualitative data Citation43. The whole interview was translated literally from Lusoga into English from the cassette recorder and then written down verbatim by a bilingual speaker. These transcriptions were checked, evaluated, and edited by another bilingual speaker. After transcription, the principal investigator read through the transcript several times and grouped the content by themes with the help of an experienced medical anthropologist. The original version was kept even after the transcription.
Quantitative data
Completed forms were checked for completeness, consistency and accuracy on a daily basis and before data entry into a computer. We used Epidata for data entry and the data analysis was performed using SPSS version 15.0 for Windows.
Data analysis
Manual content analysis
Analysis of data from focus group discussions followed steps described by Warden and Wong Citation48. The case vignettes had guiding questions to produce transcripts. A bilingual clinician transcribed the recorded discussions verbatim. The researcher then read through the transcripts several times to become familiar with the data. Coding (highlighting ideas, categories, or themes) of the data according to the questions discussed took place as the researcher read through the transcripts. This was done by placing expressions, lines, or paragraphs (sorting) that described similar codes on the left-hand side. Common themes or patterns that emerged were then placed together and interpreted.
Logistic regression
For study II, associations between socio-demographic factors and psychological distress were evaluated using an SRQ cutoff point of at least 6 of the first 20 items of SRQ. This level was based on reports from validation studies conducted in Kampala and elsewhere in Africa Citation49. Multivariate logistic regression was applied to produce odds ratios (OR) of associations between independent demographic variables and outcomes of cutoff points of SRQ, and adjusted to address the influence of other significant variables. Based upon the cutoff levels, the outcome of psychological distress was dichotomized into respondents exhibiting psychological distress (≥6 ‘yes’ answers) and those not exhibiting psychological distress (≤5 ‘yes’ answers).
Continuous independent variables were categorized for the analysis. All demographic data that were statistically significant (P<0.05) following a univariate analysis to test for the strength of association were included for the multivariate analysis.
For study III, the relationship between severity and the combined use of biomedical services and traditional healers was explored using Pearson's chi-square tests and odds ratios. For study IV, bivariate and multivariate analyses were used to determine factors associated with outcome. The level of statistical significance was set at 5% (i.e. P<0.05).
One-way ANOVA for independent samples
In study IV, outcome was determined by the mean scores of the scales at the three levels of follow-up (i.e. point of first contact as baseline and 3 and 6 months later). The mean scores were calculated using one-way ANOVA for independent samples. The Tukey HSD test was used for post-ANOVA comparisons.
Ethical clearances and considerations for the four studies
The study was approved by the local research ethics committee at Makerere University, the National Council of Science and Technology (HS 323), and the Research Committee (Forskningsutskottet), Ethical Council, at the Karolinska Institutet (Dnr 05/07). The Office of the Resident District Commissioner, Jinja and Iganga districts, and leaders of traditional healers also approved the study. Every participant gave informed verbal and written consent.
For paper I, ethical issues in qualitative research differ somewhat from other data collection methods in terms of consent, confidentiality, anonymity, privacy, and voluntary participation Citation56. What was important was the responsibility of the individual focus group's code of conduct regarding the above. The moderators accordingly had another set of ground rules to which everyone had to adhere. Focus group data were collective data and had to be treated as such. The ground rules and reciprocal trust were negotiated upfront for the shared protection of all participants Citation51. This was particularly crucial because the topic under investigation was sensitive. The other ethical issue in paper I concerned dealing with perceptions of mental illnesses from the biomedical point of view. During the collection of these data, it was clear that the perceptions of some participants differed from the biomedical view of the causation of mental illness and, therefore, its treatment. In addition, there was a demand from the participants for information about biomedical aspects of the cases under investigation. This could not be dealt with during data collection because that would have biased the whole process. The solution was to organize an open discussion after the FGDs to answer some of the questions. However, we did not attempt to impose the biomedical view of mental illness on the participants.
Studies II–IV were conducted at the traditional healers’ shrines; this raised special ethical concerns regarding traditional healer's clients who needed life-saving interventions. We dealt with this by discussing with the traditional healer the possibility of referring the patient to a health center. We did not collect any data from these patients.
Summary of results
Lay concepts of psychosis (I)
This was a pilot study to explore the lay concepts of psychosis among the local people in the study. The themes that emerged were categorized as follows:
Identification/classifying/naming of the illnesses
Perception of causation of the illnesses
Suggested treatment of the illnesses
Regarding causation and treatment, schizophrenia and psychotic depression were generally said to be caused by family/clan issues, including ancestral spirits and witchcraft, which called for the performance of rituals. Physical complaints (e.g. HIV and malaria) were mentioned as the cause of mania; referral to hospital was then mentioned as part of the treatment in addition to the traditional healer's herbal treatment. A few participants thought that the patient with mania was not ill but was exhibiting God's power or backsliding, faith healing was therefore mentioned as the appropriate treatment. Substance misuse came up as causes of the above illnesses, with a tone of condemnation. This may translate into the notion of moral failing and thus elicited blame and mistreatment rather than understanding and empathy during therapy.
Prevalence and associated factors of psychological distress (II) and mental illness (III)
Study II aimed to determine the magnitude and associated factors of psychological distress among persons who attend traditional healing. Of those attending traditional healing practices, 252 (65.1%) scored six or more on the SRQ 20. They were therefore classified as having psychological distress. In terms of gender, 70.4% of the males were distressed compared to 61.2% of the females but the difference was not statistically significant. The multivariate logistic regression analysis of the associations between demographic variables and the outcomes of psychological distress revealed that married females with co-wives were over three times more likely to be distressed than those who were the only wife (p=0.012; OR 3.62 [95% CI 1.38–10.98]). In contrast, married men with more than one wife seemed to be protected for psychological distress (p = 0.001; OR 0.20 [95% CI 0.06–0.63]), suggesting that polygamy is psychologically protecting for men but psychologically distressing to women.
Among other socio-economic indicators, persons who had lacked food at least once in the past month or who were in debt were twice as likely to be distressed; (p = 0.001; OR 2.52 [95% CI 1.25–4.72]) and (p = 0.002; OR 2.52 [95% CI 1.40–4.53]), respectively. Respondents who were attending the traditional healer's place both for treatment and for explanations for their illness were twice as more likely to be distressed (p=0.02; OR 2.17 [95% CI 1.33–3.34]) as those who wanted treatment only. On the other hand, those who stated they had visited a health centre as well as the traditional healer for the same problems were less likely to be distressed (p<0.001; OR 0.28 [95% CI 0.18–0.44]). shows the relationship between socio-demograghic variables and psychological distress of the respondents at traditional healers shrines.
Table 1. Relationship between some socio-demographic variables and psychological distress of the respondents at traditional healers’ shrines
In study III with 387 respondents, 233 (60.2%) had at least one current diagnosed disorder. There were 63 (16.3%) who had experienced at least one disorder in their lifetime, while 170 (44%) had had two or more episodes. Psychosis was most frequent occurring in 115 (29.7%) of the sample: 5.4% major depressive episode, 5.6% anxiety disorders, 3.6% mixed anxiety-depression, and 3.9% suicidality. In terms of severity, 37.7% of the current mental illnesses were severe, 35.1% moderate, and 13.2% mild.
The exploration of the relationship between GAF scores, number of episodes, combined use of traditional healing practices, and a positive family history revealed that patients with GAF scores in the moderate and severe range were more likely to have a family history of mental illness (p<0.0001), to have had two or more episodes previously (p = 0.06 and 0.03, respectively), and to have sought help from traditional healers and biomedical services for the same problems (p<0.0001). shows the prevalence of (current) DSM -IV disorders of the attendees of traditional healing in Jinja and Iganga districts.
Table 2. Prevalence of (current) DSM–IV disorders of the attendees of traditional healing in Jinja and Iganga districts
Outcome of treatment (IV)
This study was a follow-up of a cohort of patients with severe mental illness attending traditional healers. There was a general trend for symptom scales to show a reduction at the 3- and 6-month follow-ups. The percentage reduction was greatest for PANSS (30%, 40%), followed by YMRS (21%, 28%), and MADRS (29%, 20%). However, in terms of patients’ cutoff points for diagnosis, the general improvement at 3 months was greatest in patients with mania (54.0%), less so with psychotic depression (42.0%), and least with schizophrenia (14.8%). At 6 months, the percentage of patients who showed an improvement was as follows: mania (58.3%), psychotic depression (46.4%), and schizophrenia (30.7%). One-way ANOVA for independent samples analysis showed that the differences between the mean scores of the scales were all significant (P < 0.0001). The Tukey HSD tests were also all significant at P<0.01 except for MADRS, where severity of depression did not differ significantly between 3 and 6 months.
Traditional healing and biomedical services were used concurrently by over 80% of the subjects, of whom the majority were patients with mania. Concurrent use was greatest in the first 3 months of follow-up. At the bivariate level of analysis, poor economic status, early age of onset, longer duration of symptoms, previous episodes, positive family history, current illness severity, and comorbidity were factors significantly associated with poor outcome. In multivariate analysis, only two variables – combined use of biomedical services and traditional healing, and socio-economic status (represented here by being in worrisome debt) – remained significant at both the 3- and the 6-month follow-up. Those who combined treatment were less likely to be cases at the 3-month follow-up (P=0.002; OR 0.26 [0.15–0.58]) but more likely at the 6-month follow-up (P=0.020; OR 2.05 [1.10–3.19]). Being in worrisome debt was associated with caseness at both 3 and 6 months, P<0.001; OR 11.21 [6.58–17.26]) and P=0.01; OR = 2.23[1.41–3.53], respectively. shows results of bivariate analysis associated with caseness at three and six months follow up.
Table 3. Results of bivariate analysis of factors associated with caseness
Discussion
Main findings
The local people in this study had indigenous names for different types of psychoses and multiple explanatory models for them. More than half of the attendees of traditional healing practices had psychological distress. Associated factors included poverty, number of children, polygamy, reason for visiting the healer,and use of both traditional healing and biomedical services. In addition, a considerable number have DSM–IV diagnosable mental disorders, the majority with moderate to severe symptoms. The follow-up study of patients with psychosis suggests that combining biomedical services and traditional healing may have some positive effects for patients.
Burden of care of mental illness on traditional healers
These four studies suggest that when people need psychological help, they look for it wherever it can be found. Thus a traditional healer, present in every village, bears the burden of the community's mental illnesses.
The care of people with mental and brain disorders is a growing public health concern. These disorders are highly prevalent and exert a high emotional toll on individuals, families, and society. Worldwide, community-based epidemiological studies have estimated rates of lifetime prevalence of mental disorders among adults ranging from 12.2% to 48.6%, and 12-month prevalence rates ranging from 8.4% to 29.1% Citation52. These rates do not include neurological conditions affecting the brain. The WHO has estimated that in their lifetime, approximately 450 million individuals worldwide suffer from neuropsychiatric disorders Citation27. The WHO has reported that the treatment gap for serious disorders is 76 to 85% for low- and middle-income countries and also states that shortages of health care professionals have been shown to be the main factor that limits the delivery of mental health care in most of these countries Citation25. Evidence-based data are needed on the effectiveness of treatment by traditional healers to help us understand their role in reducing the burden of mental illnesses.
Use of biomedical health care and traditional healing: a holistic approach
Holistic medicine is a system of health care that fosters a cooperative relationship among all those involved, leading toward optimal attainment of the physical, mental emotional, social, and spiritual aspects of health Citation38. It emphasizes the need to look at the whole person, including analysis of physical, nutritional, environmental, emotional, social, and spiritual and lifestyle values. Health cannot be achieved without achieving a balance in life with others and with the environment. Beliefs, values, and attitudes affect health and must be part of the cure Citation38.
The current health system tends to place overt emphasis on a commitment to the biomedical model; too much is invested in this model, yet it tends to avoid the personal dimension Citation36. This inherent weakness of the biomedical model is reflected in the negative attitude of biomedical health workers including western trained psychiatrists. According to the holistic integrated model of health and healing, we exist in five different dimensions simultaneously and our patients need care on every level of existence. Papers II and IV provide evidence that the patient who uses both biomedical services and traditional healing fair better than those who do not combine these forms of care. Findings from these four studies indicate hardly any interaction between the traditional healers and the biomedical health workers although patients utilize the two health providers’ services simultaneously.
In Uganda, the current mental health care system can be characterized as fragmented and disintegrated. Fragmentation is to be found within psychiatric services. The hospitals and health units have a small range of mental health professions, if any. In addition, professional competence is bound by tradition. Medical core competence is still seen as somatic diagnosis and therapy, particularly in psychopharmacology. Efforts at professional integration face many barriers. Another form of fragmentation may be far more serious for patients. It is the fragmentation of the professional health care providers. There are virtually non-existent contacts between hospital professionals and health workers at community level. The patients’ daily world and its related problems are scarcely present inside the hospital. The very few mental health professionals are unable to know their patients’ homes. Basic skills for coping with daily life and basic social and communicative techniques that could make life easier for the mentally ill remain a distant prospect Citation37.
The current mental health care system and its fragmentation would not cause concern if there were a recognized facilitated integrating body that could adequately unite all forces for the patient's comprehensive needs. But, at least in Uganda, this does not exist – mental health professionals and traditional healers operate separately
It became clear to the WHO 30 years ago and it should be clearer now to the global health movement that timely joint efforts are the main component of an optimized mental health care system. A range of options has been suggested Citation11. They range from banning traditional healers and hunting them down so that their practices are stopped, through options such as the retention of the status quo (with western health care in the formal sector and traditional healing in the informal sector) with pockets of cooperation, to alternatives in which the state actively intervenes to achieve collaborative, incorporative, or integrative programs Citation11. Within the fragmented and disintegrated system of today's psychiatric care in Uganda, it may be impossible to meet patients’ needs, at least in the near future.
The next section discusses methodological considerations, focusing on validity issues in transcultural psychiatry and levels of the quality of evidence. Although this thesis is about outcome and not healing mechanisms, the author feels that some discussion of those mechanisms is relevant. This is also included in the next session.
Methodological considerations
Validity issues in transcultural epidemiology
Transcultural epidemiology researchers are more likely to encounter problems of validity. Transcultural epidemiology is defined as when the views, concepts, or measures of the investigator extend beyond the scope of one cultural unit to another Citation53. The context of research affects research validity. Realistic and effective methods for reducing uncertainty in findings of transcultural studies are available and were used in this thesis. We achieved diagnostic validity by first exploring the lay understanding of psychosis (Paper I), which gave us ideas about local concepts and phrases used to describe symptoms, syndromes, course, and clinical features of psychosis. This gave us evidence that psychosis exists in this community in forms similar to those cultures from which the standardized instruments came.
Literal translation can reduce content validity, which is the extent to which a measure's content represents the concept to be assessed Citation53. To maintain content validity, locally meaningful equivalent terms were substituted.
Regarding criterion-related validity, which is the strength of the relationship between the measure and the measurable external criterion (the ideal external criterion is considered to be the diagnosis by independent clinicians who are trained in using semi-structured diagnostic instruments that have evidence for measurement validity and reliability), we used clinicians who are trained to make psychiatric diagnosis and trained them in the use of a semi-structured diagnostic instrument, the MINI plus.
Users of epidemiological data, such as policy-makers, need to know to what extent findings have external validity, i.e. generalizability to the target population, or other populations and across time and place. Generalizability to the target population depends on the ability to randomly draw a representative sample from the entire population of relevant persons Citation54. The ability to do so requires the availability of reliable registers with contact information for the entire target population. In our studies, we used the registers of traditional healers in the two districts. However, for various reasons, not all traditional healers are registered. Generalizability to the target population also depends on the study's participation rate, i.e. the percentage of sampled people who are willing to participate in the study. In our study, no participant refused to take part, which enhanced out external validity.
The extent to which findings from one cultural unit can be generalized to other populations is still a matter for debate. Not much is known about the generalizability of epidemiological findings across populations Citation54.
In a qualitative study, one potential bias is researcher bias (i.e. searching for and finding or confirming only what you want or expect to find). Two strategies that were used to reduce researcher bias were reflexivity, i.e. constantly thinking about our potential biases and how we can minimize their effects and negative case sampling (attempting to locate and examine cases that disconfirm your expectations). We used the following strategies to promote the qualitative aspect of the study.
Verbatims (i.e. direct quotations) as low-inference descriptors; focus groups consisting of men and women of varying ages; local people and traditional healers served for data triangulation; and multidisciplinary researchers for collecting, analysis, and interpretation of data (investigator triangulation). In addition, we had feedback and a discussion of our interpretations and conclusions with the actual participants and other members of the participant community for verification and insight. A discussion of our findings with other peers included one person who is disinterested in our research; peers who are familiar with the research helped to provide useful challenges and insights.
Outcome measures in psychiatry and levels of evidence
Mental health care increasingly faces a challenge to be ‘evidence-based.’ Mental health professionals are encouraged to practice only evidence-based care. Researchers are supposed to provide the evidence on which mental health care is to be based. However, this raises the questions of what constitutes evidence and to what extend we agree on what is regarded as evidence. There are large variations in the quality of scientific evidence that may exist in support of medical diagnoses and treatment Citation55. Lawrence has stratified the quality of evidence from best to worst with systemic reviews and meta-analysis in the best positions while expert opinion, anecdotes, and clinical experience are in the worst positions. Prospective, masked randomized controlled clinical trials; cohort and case-control studies; cross-sectional surveys; case reports; and series fall in between Citation56.
The third phase of the study was basically at the level of an uncontrolled cohort study, where patients were enrolled who were receiving traditional healing treatment from the shrines but there was no control group. A study protocol specified the characteristics of subjects, treatment, and outcome measures. Because there was no control group, the results of this particular study should be interpreted with caution as number factors could have biased the results. Some of these factors include: the Hawthorne effect, defined as the tendency of subjects to do better solely because they are being studied Citation56. This may involve subjects’ expectations but can also be a result of non-specific effects of the study situation such as increased attention. The Pygmalion effect and co-interventions, also called the experimenter expectancy effect is where experimenters’ expectations of effects of treatment may result in differential attention to or interaction with some subjects and thereby lead to a change in subjects’ behavior toward the experimenter's hypothesis Citation57. A related effect is that of a clinician involved in the study providing additional care (e.g. time, support) to patients in the study group. This effect is known as performance bias Citation56.
The third non-specific effect is the placebo effect. In this effect, it is the subject's expectation of an improvement, combined with other non-specific psychotherapeutic effects that leads to improvement Citation58,Citation59. The magnitude of the placebo response varies between disorders. It is greater in depression and anxiety than in schizophrenia and mania.
The final important source of bias is observer, detection, or ascertainment bias Citation60. If an interviewer or rater knows which treatment a patient is receiving, he or she may differentially inquire about certain systems or see an improvement where none exists. In our study, this was minimized because the raters did not know what the traditional healers were giving the patient.
Despite the above sources of bias, we nevertheless believe that the results of the outcome study may provide a stepping stone for future research in this area. Although methods vary in the strength of the evidence they produce, every method, when used appropriately, can lead to valuable conclusions Citation61. All these study designs have merits and all can produce useful findings Citation61. Indeed, new medical knowledge is most often obtained through observational means, whether through a complex prospective cohort study or through a simple case series. This is typically an important first step in understanding an effect on the particular outcome of a previously unconsidered factor as is the case with this study.
The main conclusions from these studies:
The local people in this study had indigenous names for different types of psychoses and multiple explanatory models for them. Schizophrenia (eddalu or ilalu) was viewed as a more serious illness, with the possibility of not recovering, mania (kazoole), as less serious mental illness, with normality between episodes. Psychotic depression was seen as illness caused by too much thinking. Clan/family/cultural issues were mentioned as causing schizophrenia and psychotic depression, while physical causes and a failed relationship with God were mentioned for mania. Other causes were witchcraft, genetics, and substance misuse Citation41. Thus multiple solutions were sought for these problems (Paper 1).
About 65% of the attendees of traditional healing practices in Jinja and Iganga districts had psychological distress, 60% had at least one diagnosable current mental illness and 16.3% had at least one disorder in their lifetime thus traditional healers bear a high burden of care of patients with mental health problems.
An overwhelming majority of Ugandans with severe mental illness in the Jinja and Iganga districts use both biomedical services and traditional healing systems.
For patients with psychosis, the use of both biomedical services and traditional healing practices seems to confer some benefits.
Implications for policy-makers, clinicians, researchers, and medical educators
In Uganda, the enormous existing and planned investment in biomedical services alone strongly favors approaches to the care of patients that emphasize the biomedical model of care. Planning for systems of medical care and their financing is excessively influenced by the availability of evidence of effectiveness, which is often used as the criterion on which policy decisions are based. Clearly, the gap to be closed is between biomedical health workers ready to carry out research in traditional healing and policy-makers eager to change policies for the benefit of the patient. For clinicians, there is a need to know about potential dangers including toxicity and drug interaction with herbs. This calls for acquiring knowledge about traditional healing and being positive toward the patient's use of this alternative method.
Furthermore, the ability to deal with uncertainty in clinical practice is essential in clinical decision making. These same skills are needed to assess all therapies regardless of their nature or attributes. Practitioners of biomedicine and traditional healing must both draw on diverse knowledge bases with varying levels of certainty and different ways of knowing and practicing. It would be a good development if both practitioners had open, respectful discussions of their different ways of doing things. Exploring this in the context of the medical school curriculum would enrich the dialogue between current practitioners and help develop an open-minded generation of physicians better able to assess the therapies that might help individual patients. Thus, a growing interest in diversity and training in traditional healing may increase cultural competence.
The decision by mental health professionals to support, encourage, or counsel against traditional healing practices used by their patients heavily depends on the available evidence. Thus, research identifying effective and ineffective traditional healing practices in mental health may contribute to evidence-based medicine and could improve medical care.
Furthermore, as the world moves toward personalized care, and given the widespread use of traditional healing, sound research findings will help consumers make more informed personal health care choices. In addition, research may be the only means to reveal the mechanisms of action of effective traditional healing therapies. The research findings will also have the potential to enhance understanding and treatment of mental illnesses.
Finally, research on traditional healing practices may lead to the discovery of new ways of dealing with the prevalent mental health problems; for example, perhaps the combination of traditional healing practices and modern medicine could be an answer.
Conflict of interest and funding
This study was sponsord by Sida&fslash;SAREC and additionally supported by Astra Zeneca/American Psychiatric Association.
Acknowledgements
My gratitude to all the traditional healers, respondents, the community members of the Busoga region; my supervisors: Solvig Ekblad, Paul Waako, and Elialilia Okello; The Head and Staff of the Department of Psychiatry and Butabika Hospital. This project would not have been possible without the sponsorship of Sida/SAREC. Additional support came from the APA/ASTRAZENECA Young Minds International Award 2005.
References
- WHO. WHO policy perspective on medicines – traditional medicine – growing needs and potentials. Geneva: Author. 2002.
- Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M, et al.. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998; 280: 1569–75. 10.3402/gha.v4i0.7117.
- Unutzer J, Klap R, Sturm R, Young AS, Marmon T, Shatkin J, et al.. Mental disorders and the use of alternative medicine: results from a national survey. Am J Psychiatry. 2000; 157: 1851–7. 10.3402/gha.v4i0.7117.
- Okello E, Musisi S. Depression as a clan illness (eByekika): an indigenous model of psychotic depression among the Baganda of Uganda. J World Cultural Psychiatry Res Rev. 2006; 1: 60–73.
- Patel V. Explanatory models of mental illness in Sub-Saharan Africa. Soc Sci Med. 1995; 40: 1291–8. 10.3402/gha.v4i0.7117.
- Abbo C. Traditional healers and management of mental health problems in Uganda. LAP Lambert Academic Publishing. Saarbrueken, 2010
- Kapur RL. Mental health care in rural India: a study of existing patterns and their implications for future policy. Br J Psychiatry. 1979; 127: 286–93. 10.3402/gha.v4i0.7117.
- Incayawar M. Efficacy of Quichua healers as psychiatric diagnosticians. Br J Psychiatry. 2008; 192: 290–391. 10.3402/gha.v4i0.7117.
- Kleinman A, Sung L. Why do indigenous healers successfully heal?. Soc Sci Med Part B: Med Anthropol. 1979; 13: 7–26. 10.3402/gha.v4i0.7117.
- Green EC, Makhubu L. Traditional healers in Swaziland: toward improved cooperation between the traditional and modern health sectors. Soc Sci Med. 1984; 18: 1071–9. 10.3402/gha.v4i0.7117.
- Freeman M, Motsei M. Planning health care in South Africa – is there a role for traditional healers?. Soc Sci Med. 1992; 34: 1183–90. 10.3402/gha.v4i0.7117.
- Shaughnessy AF. Alternative views on alternative medicine. Ann Intern Med. 1999; 131: 229a.
- Opobo T. Involve traditional healers in the fight against child murder. The Monitor Newspaper. Kampala, 2009
- The Witchcraft Act. In the laws of the Republic of Uganda. Uganda:1964.
- Ranny I. Legislators demand end to child sacrifice.. 2009. Available from: http://www.Allafrica.com.
- Kirunda A. Police chief orders traditional healers to register afresh. The Monitor Newspaper. Kampala, 2009
- THETA. Contributions of traditional medicine to health care deliveries in Uganda. Kampala: Ministry of Health, Public and Private Partnership Office. 2001.
- Good CM, Kamani VM. Urban traditional medicine. East Afr Med J. 1980; 57: 301–17.
- Baingana F. The use of modern and traditional psychiatric services. Department of Psychiatry, Makerere University. Kampala, 1994
- Kale R. Traditional healers in South Africa: a parallel health care system. BMJ. 1995; 310: 1182–5.
- Stein DJ, Seedat S. From research methods to clinical practice in psychiatry: challenges and opportunities in the developing world. Int Rev Psychiatry. 2007; 19: 573–81. 10.3402/gha.v4i0.7117.
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. Plos Med. 2006; 3: e344.10.3402/gha.v4i0.7117.
- Muhwezi W, Agren H, Neema S, Maganda AK, Musisi S. Life events associated with major depression in Ugandan Primary Healthcare Care (PHC) patients: issues of cultural specificity. Int J Soc Psychiatry. 2008; 54: 144–63. 10.3402/gha.v4i0.7117.
- Kasoro S, Sebudde S, Kabagambe-Rugamba G, Ovuga E, Boardman A. Mental illness in one district in Uganda. Int Soc Psychiatry. 2002; 48: 29–37. 10.3402/gha.v4i0.7117.
- Chisholm D, Flisher A, Lund C, Patel V, Saxena S, Thorncroft G, et al.. Scaling up services for mental health disorders. Lancet. 2007; 370: 1241–52. 10.3402/gha.v4i0.7117.
- Saxena S, Throncroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity and inefficiency. Lancet. 2007; 370: 878–89. 10.3402/gha.v4i0.7117.
- WHO. (2001): Mental health: new understanding new hope. The World Health Report.. Geneva: Author..
- Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, et al.. Barriers to improvement of mental health services in low and middle income countries. Lancet. 2007; 370: 991–1005. 10.3402/gha.v4i0.7117.
- APA. Diagnostic and statistical manual of mental disorders. 5th ed.WashingtonDC: American Psychiatric Association. 1994.
- Lambo T. Neuropsychiatric observations in the Western Region of Nigeria. BMJ. 1956; 2: 826–33. 10.3402/gha.v4i0.7117.
- Orley J. Culture and mental illness: a study from Uganda. East Africa Publishing House. Nairobi, 1970
- Prince R. The use of rauwolfia for treatment of psychosis by Nigerian native doctors. AJP. 1960; 117: 147.
- Okello E, Neema S. Explanatory models and help seeking behaviour: pathways to psychiatric care among patients admitted for depression in Mulago Hospital, Kampala, Uganda. Qual Health Res. 2007; 17: 14–25. 10.3402/gha.v4i0.7117.
- Kleinman A, Eisenberg L, Good B. Culture, illness and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978; 88: 251–8.
- Saravanan B. Explanatory models in psychiatry. Br J Psychiatry. 2002; 181: 351.10.3402/gha.v4i0.7117.
- Engel L. The need for a new medical model: a challenge to biomedicine. Science. 1977; 196: 129–36. 10.3402/gha.v4i0.7117.
- Richter D. Chronic mental illness and the limits of the biopsychosocial model. Med Health Philosophy. 1999; 2: 21–30. 10.3402/gha.v4i0.7117.
- Klinghardt D. The five levels of healing. Explore. 2005; 14: 1–5.
- Sewell R. Holism – remembering what it is to be human. Complement Ther Clin Pract. 2008; 14: 75–76. 10.3402/gha.v4i0.7117.
- UBOS. 2002. Uganda population and housing census. Kampala: Uganda Ministry of Finance and Economic Planning. 2005.
- Abbo C, Okello ES, Ekblad S, Waako P, Musisi S. Lay concepts of psychosis in Busoga, Eastern Uganda: a pilot study. WCPRR. 2008; 3: 132–45.
- Abbo C, Ekblad S, Waako P, Okello E, Muhwezi W, Musisi S. Psychological distress and associated factors among the attendees of traditional healing practices in Jinja and Iganga districts, Eastern Uganda: a cross-sectional study. Int J Ment Health Syst. 2008; 2: 16.10.3402/gha.v4i0.7117.
- Baarnhielm S, Ekblad S. Qualitative research, culture and ethics: a case discussion. Transcultural Psychiatry. 2002; 39: 469–83. 10.3402/gha.v4i0.7117.
- Kish L. Survey sampling. Wiley Interscience Publication. New York, 1965
- Ngoma MC, Prince M, Mann A. Common mental disorders among those attending primary health clinics and traditional healers in urban Tanzania. Br J Psychiatry. 2003; 183: 349–55. 10.3402/gha.v4i0.7117.
- Okello ES, Abbo C, Tusaba C, Musisi S. Incorporating traditional healers in primary health care in Uganda. Makerere Univ Res J. 2006; 1: 139–48.
- Merton RK, Fiske M, Kendall PL. The focused interview: a manual of problems and procedures. Collier MacMillan. London, 1990
- Warden BA, Wong S. Introduction to qualitative data analysis. Constella Group. New York, 2007
- Tafari S, Aboud FA, Larson CP. Determinants of mental illness in rural Ethiopian adult population. Soc Sci Med. 1991; 32: 197–201. 10.3402/gha.v4i0.7117.
- Richards HM, Schwartz LJ. Ethical issues in qualitative research: Are there special issues for health services research?. Family Practice. 2002; 19: 135–139. 10.3402/gha.v4i0.7117.
- Smit B. Understanding implicit texts in focus groups from systems psychodynamic perspective. Qualitative Report. 2006; 11: 302–316.
- Gureje O, Lasebikan VO, Kola L, Makanjuola VA. Lifetime and 12-month prevalence of mental disorders in the Nigerian Survey of Mental Health and Well-Being. Br J Psychiatry. 2006; 188: 465–71. 10.3402/gha.v4i0.7117.
- Van Ommeren M. Validity issues in transcultural psychiatry. Br J Psychiatry. 2003; 182: 376–8. 10.3402/gha.v4i0.7117.
- Lundberg GD. Scientific evidence-based medical practice: where are we now?. Hong Kong Med J. 1998; 4: 103–8.
- Lawrence RS, Mickalide AD. Preventive services in clinical practice: designing the periodic health examination. JAMA. 1987; 257: 2205–2207. 10.3402/gha.v4i0.7117.
- Sith-Amorn C, Poshyachinda V. Bias. Lancet. 1993; 342: 286–8. 10.3402/gha.v4i0.7117.
- Holden J. Hawthorne effects and research into professional practice. J Eval Clin Pract. 2001; 7: 65–70. 10.3402/gha.v4i0.7117.
- Crow R, Gage H, Hampson S. The placebo effect: methodological implications of a structure interview. Advanced handbook of methods in evidence based health care. Stevens AJ, Abrams KR, Brazier J, FitsPatrick R, Lilford RJ.Sage. London, 2001
- Laporte J.-R. Placebo effects in psychiatry. Lancet. 1994; 344: 1206–9. 10.3402/gha.v4i0.7117.
- Moses LE. Measuring effects without randomised trials?: options, problems and challenges. Med Care. 1995; 33: AS8.
- Hennekens CH, Buring JE. Epidemiology in medicine. MA: Little, Brown & Co. Boston, 1987