Abstract
Background
The integration of mental and neurologic services in healthcare is a global priority. The universal Social Security of Costa Rica aspires to develop national screening of neurodegenerative disorders among the elderly, as part of the non-communicable disease agenda.
Objective
This study assessed the feasibility of routine screening for Parkinson's disease (PD) and Alzheimer's disease (AD) within the public healthcare system of Costa Rica.
Design
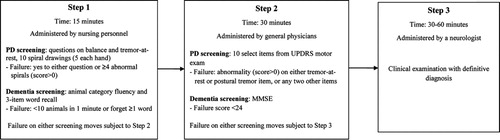
The population (aged ≥65) in the catchment areas of two primary healthcare clinics was targeted for motor and cognitive screening during routine annual health check-ups. The screening followed a tiered three-step approach, with increasing specificity. Step 1 involved a two-symptom questionnaire (tremor-at-rest; balance) and a spiral drawing test for motor assessment, as well as a three-word recall and animal category fluency test for cognitive assessment. Step 2 (for those failing Step 1) was a 10-item version of the Unified Parkinson Disease Rating Scale and the Mini-Mental State Examination. Step 3 (for those failing Step 2) was a comprehensive neurologic exam with definitive diagnosis of PD, AD, mild cognitive impairment (MCI), other disorders, or subjects who were healthy. Screening parameters and disease prevalence were calculated.
Results
Of the 401 screened subjects (80% of target population), 370 (92%), 163 (45%), and 81 (56%) failed in Step 1, Step 2, and Step 3, respectively. Thirty-three, 20, and 35 patients were diagnosed with PD, AD, and MCI, respectively (7 were PD with MCI/AD); 90% were new cases. Step 1 sensitivities of motor and cognitive assessments regarding Step 2 were both 93%, and Step 2 sensitivities regarding definitive diagnosis 100 and 96%, respectively. Specificities for Step 1 motor and cognitive tests were low (23% and 29%, respectively) and for Step 2 tests acceptable (76%, 94%). Based on international data, PD prevalence was 3.7 times higher than expected; AD prevalence was as expected.
Conclusion
Proposed protocol adjustments will increase test specificity and reduce administration time. A routine screening program is feasible within the public healthcare system of Costa Rica.
Mental health and neurological disorders are among the global priorities of the World Health Organization (WHO) (Citation1, Citation2). Neurodegenerative diseases are incurable conditions that result in progressive degeneration and death of nerve cells leading to problems with motor or mental functioning. Parkinson's disease (PD) and Alzheimer's disease (AD) are major concerns considering the world's aging populations, with the largest increases expected to happen in countries in transition (Citation3). Data on prevalence and incidence are scarce, especially in developing countries, but AD (and other dementias) and PD are listed among the 14 most important causes of disease burden caused by mental illness (Citation3). Mental, neurologic, and substance abuse (MNS) disorders account for an estimated 13% of net global burden of disease, with the greatest weight carried by low- and middle-income countries (LMICs) where these pathologies are widely neglected (Citation1–(Citation3)). The Disability Adjusted Life-Years (DALYs) for LMICs were recently estimated in 6.8 million for AD and other dementias and 1 million for PD (Citation3).
Despite the public health importance of AD and PD, clinicians in developing countries have insufficient means to adequately diagnose and treat such neurodegenerative disorders. The clinical management of Parkinson's and Alzheimer's patients gets even more complicated with the presence of other chronic diseases common with aging. The physical and cognitive disabilities also affect the quality of life and economic productivity of family members on whom these patients depend for care. Caretakers in developing countries most often lack guidance or professional support. WHO aims at scaling up services for MNS disorders in LMICs (Citation1, Citation2). This need has also been identified by the Grand Challenges to Global Mental Health (GCGMH) initiative, which includes among its aims to integrate mental health (or MNS disorders) into research, policy, and practice; to integrate care into the non-communicable disease agenda; and to integrate services into priority healthcare platforms (Citation4, Citation5).
Costa Rica is a medium income developing country in Central America. Life expectancy is high, 79 years in 2011 (Citation6). According to the census of 2011, 7.3% of the 4.5 million population was aged ≥65, and it is estimated that by 2050, this number will have tripled and exceeded the group under age 15 (Citation7). The public health system in Costa Rica has an almost universal coverage. By 2009, 88% of the population was insured by the Social Security of Costa Rica (CCSS) (Citation8). About 80% of the population aged ≥65 uses the services of CCSS (Citation9). Costa Rican health authorities are committed to tackle chronic non-communicable diseases, including neurodegenerative diseases related to aging.
The organizational basis of CCSS consists of approximately 1,000 primary healthcare units with catchment populations of about 4,000, called ‘Basic Teams for Integrated Health Assistance’ (EBAIS), including a physician and a nurse. The CCSS has a routine annual wellness evaluation program for the population aged ≥65 with 65% participation nationwide (Vilma García, CCSS, personal communication). The CCSS anticipates monitoring chronic diseases through this special program, including PD and AD.
This collaborative study aimed to assess the feasibility of a government screening program for neurodegenerative diseases among the elderly in Costa Rica integrated into the universal primary healthcare system, as a platform for improved services, research and evidence-based interventions. The partners were investigators from CCSS and Universidad Nacional in Costa Rica, and Emory University in Atlanta, USA.
Methods
Study site and study population
We selected two primary healthcare centers (EBAIS) such that: 1) each would have at least a population of 250 persons aged ≥65; 2) at least 80% of this group would use the CCSS services; and 3) the leading staff would be committed to organizational support. The centers were the urban (formerly rural) EBAIS of Santo Tomás, and the rural EBAIS of Los Ángeles. Both EBAIS refer to the Clinic of Santo Domingo de Heredia and are close to the capital San José. The goal was to screen 500 patients. Subjects were recruited between January 2010 and January 2011.
Ethical considerations
The ethical committees of the Universidad Nacional, CCSS, and Emory University approved the study. After the attending nurse explained the study, verbal consent was obtained since the screening was conducted as part of the routine annual health check-up and comprised only non-invasive methods. There were no refusals.
Screening methods
The screening protocol involved a tiered three-step approach, using tests of proven validity. Each tier had progressively higher specificity. Since the application of the protocol added to the routine work of the staff, time was a prime consideration. The protocol is outlined in .
Step 1
Step 1 screening was administered to all participants and designed to take approximately 15 min. It included a 5-min questionnaire, two motor-symptom questions, one motor test, and two cognitive tests. The questionnaire inquired demographic data (age, sex, most common occupation, education, and district of residence) and contained a few questions to explore an association between pesticides and Parkinson disease (Citation10), specifically smoking status, history of work in agriculture and, if positive, years of occupational exposure to pesticides.
The ‘yes/no’ motor-symptom questions addressed tremor-at-rest and balance: 1) ‘During the last year, have you had tremors in one or both hands when at rest?’ and 2) ‘During the last year, has it become difficult for you to maintain your balance when walking?’. The motor test was a spiral drawing test commonly used in the assessment of Parkinsonian motor signs (Citation11–(Citation13)), consisting of drawing 10 spirals with each hand on paper sheets placed on top of a digitizing tablet, the results of which were fed into a laptop computer. Due to computer unfamiliarity, both nurses and patients perceived the computerized spiral tests as stressful. Therefore, after screening about 20% of the targeted patients (n=107), the protocol was changed to manual drawing of five spirals with each hand to reduce administration time to less than 5 min. Spirals were scored by the nurses as normal (score 0) and abnormal (score 1–4), based on the familiarity with multiple examples of normal spirals.
The two cognitive tests took only a few minutes: a word-recall test after distraction (the patient was asked to remember the words ‘house, shoe, paper’, and then to repeat them after answering the symptom questions), and a category fluency test naming as many animals as possible in 1 min.
Screening positive in Step 1 for potential PD was defined as answering positively to any of the two-symptom questions OR scoring ≥1 on at least four spirals in either hand. Screening positive in Step 1 for potential AD was defined as failing ≥1 word in the word-recall test OR naming <10 animals in 1 min.
Step 2
Step 2 was administered to those failing Step 1 by general practitioners working at the two EBAIS, the majority by a single physician (IQ). Step 2 was designed to distinguish between less specific motor and cognitive indicators and more specific early signs of PD and AD. The tests were an abbreviated version of the Unified Parkinson Disease Rating Scale (UPDRS) examination and the Mini-Mental State Examination (MMSE) questionnaire, validated scales commonly used in the screening of motor and cognitive signs, respectively.
The UPDRS version we used was a modified form of the 10-item motor subscale proposed by Louis et al. (Citation14). Tremor-at-rest was hypothesized a priori as the most sensitive item for detection of PD. Other items in the scale include speech (hypophonia), facial expressivity, axial and appendicular rigidity, bradykinesia, and abnormalities of posture and gait. In an attempt to also capture atypical presentations of PD (estimated at 20%), we also included items of postural tremor of the hands and finger tapping as a test of fine motor dexterity. By including postural tremor, we avoided excluding PD subjects who may present with essential (typically postural) tremor that later develops to PD, or patients with Lewy Body disease presenting with motor symptoms before developing dementia. Finger tapping is part of the original UPDRS and it was meant to capture characteristic abnormalities of fine motor dexterity in PD in patients without tremor (i.e. akinetic-rigid subtype). All items were scored from 0 to 2. A score of 1 indicated mild abnormality, and a score of 2 abnormality of moderate or greater severity. The application of this abbreviated UPDRS version took approximately 10 min.
The MMSE is a 10-item questionnaire that evaluates cognitive domains of orientation, registration, concentration, memory, language, and praxis. The scores range between 0 and 30 points, and the cutoff for abnormality is <24. It has been validated in Spanish (Citation15), and it is widely used in Latin America in clinical practice (Citation16, Citation17), including in the CCSS. The administration of the MMSE took about 15 min but longer in patients with cognitive deficits.
Screening positive in Step 2 for potential PD was defined as any abnormality (score >0) on the tremor-at-rest or postural tremor items of the UPDRS, OR a score >0 on at least two other items. Screening positive in Step 2 for potential AD was defined as a MMSE score <24, without adjustment for age, gender, or education.
Step 3
Step 3 of the screening protocol involved a clinical evaluation of those failing Step 2 by a neurologist specialized in aging disorders (NR). The diagnostic criteria for PD were based on the UK Brain Bank criteria (Citation18), defined as bradykinesia plus tremor-at-rest and/or cogwheel rigidity. For AD and mild cognitive impairment (MCI), diagnoses were made in agreement with current guidelines (Citation19–(Citation21)). The neurologist classified subjects as either possible/probable PD (possible PD patients presented with typical Parkinson's features including bradykinesia but without tremor), possible/probable AD, or MCI. Subjects who did not fall in these categories were considered normal or were diagnosed with other neurologic, rheumatologic, or orthopedic problems common in the elderly. The Step 3 motor examination took about 15 min and the cognitive examination about 30 min.
Training, communication, and feedback
The nursing personnel were thoroughly trained in the administration of the questionnaire and cognitive tests of Step 1. The neurologists (JJ and NR) trained the nurses and the general practitioners in the administration of the Step 1 spiral drawing test and the Step 2 UPDRS and MMSE tests, respectively. A trained field manager monitored the nurses in charge of Step 1 screening. Consistency in Step 2 assessments was reinforced and monitored by one neurologist (NR). During data collection, meetings and workshops were organized with the leading staff and those who conducted the screening, to evaluate progress and make adjustments as needed. At the end, an open-ended evaluation questionnaire was applied to all collaborating health personnel.
Statistical analyses
Analyses consisted of descriptive statistics of the demographics of the study subjects and test results. Sensitivity, specificity, and positive predictive values (PPV) were calculated for specific screening tests and for the overall failure criteria in relation to the next step as established in the protocol, assuming that those who had tested negative in the previous step were healthy.
The prevalence of PD, AD, and MCI in the study population was calculated. The expected number of PD cases in our study population was nine, derived from age-specific prevalence (0.5% ages 60–69, 1.5% ages 70–79, 3% ages ≥80) based on an international review of nine population-based studies in Europe and Asia (Citation22). The expected number for AD cases in our study population was 21, derived from age-specific prevalence (2% ages 70–79, 20% ages ≥80) based on US estimates (Citation23). For MCI no expected numbers could be calculated, due to scarcity of reliable population prevalence data. The numbers of observed PD and AD cases were compared to the expected numbers.
Results
The 401 screened subjects represented about 80% of the population aged ≥65 living in the catchment areas of the two EBAIS. A few individuals aged 60–64 were also inadvertently screened (2%). describes the study population. More women than men were tested (60 vs. 40%), almost a third was aged <70, 72% had primary education or less, and about 60% had worked in agriculture.
Table 1 Demographic characteristics of the study participants
summarizes the flow of screened subjects from Step 1 to the definitive diagnosis in Step 3. In Step 1, 370 (92%) subjects failed: 329 (82%) failed motor testing (primarily the spiral drawing test) and 297 (74%) failed cognitive testing (primarily the three-word-recall test), with 256 (64%) failing both motor and cognitive testing; only 31 (8%) of the patients passed all of the tests.
Table 2 Patient flow in a three-step screening procedure for Parkinson's disease (PD), Alzheimer's disease (AD), or mild cognitive impairment (MCI)
In Step 2, further screening tests were applied to 364 patients and, of these, 163 (45%) failed: 130 (36%) failed the UPDRS motor evaluation and 84 (23%) the MMSE cognitive evaluation, with 51 (14%) failing both motor and cognitive tests; 201 (55%) subjects passed both tests.
In Step 3, 145 of the 163 subjects who failed Step 2 underwent a neurologic examination. Of the 21 who were not examined, four had died and 17 could not be contacted or were unable to attend. Eighty-one (56%) subjects were diagnosed with a neurodegenerative disease: 33 with possible/probable PD, 20 with possible/probable AD, and 35 with MCI, with seven of these cases having a combined diagnosis of PD with MCI or AD. Of the remaining patients, 24 did not have a specific disorder and 40 had other diagnoses that explained motor or cognitive failure in Step 2, including psychiatric and mood disorders, disorders of the peripheral nervous system, and musculoskeletal disorders. Tremor-related pathologies were present in 34 of these patients (19 essential, 11 drug-induced and four cerebellar tremors).
Step 1 overall motor and cognitive failure criteria had a high sensitivity to predict failure on the UPDRS and MMSE of Step 2 (both 93%) but a low specificity (23 and 29%, respectively) (). The results for the motor subtests of Step 1 varied, with the self-reported symptom of tremor-at-rest having a higher PPV than the balance symptom and spiral drawing test. Regarding the cognitive subtests, the animal fluency test was less sensitive but more specific and had a higher PPV than the word-recall test. The sensitivity and specificity of Step 2 UPDRS for PD were, respectively, 100 and 76%, and of MMSE for AD/MCI were 96 and 94%.
Table 3 Sensitivity, specificity, and positive predictive value (PPV) for tests used in the screening for Parkinson's disease (PD) and for Alzheimer's disease (AD) or mild cognitive impairment (MCI)a
Only four of the 33 patients with possible/probable PD had a previous diagnosis of PD, and two of the 35 MCI patients and two of the 20 AD patients had a previous diagnosis of memory problems. Overall, 90% of the cases detected in this screening pilot were new. The prevalence in the study population (with untested patients in Step 2 and Step 3 in the denominator) was 8% for PD, 5% for AD, and 9% for MCI, with no differences between men and women. The observed number of PD cases (n=33) was 3.7 times higher than the nine expected cases. The number of observed AD cases (n=20) was similar to the expected number of 21.
Annex 1 contains detailed results for the screening parameters of all tests of cognition and motor control used in this study in relation to the final diagnosis, according to different cutoff points and failure criteria.
In the final qualitative evaluation, all health personnel valued an early detection system for neurodegenerative diseases as important and feasible. The extra workload was a concern, which sometimes affected motivation, in particular among the nurses. Due to the low specificity of the Step 1 tests, the workload was much higher than anticipated for the general physicians participating in Step 2. The customary time allocated per patient was insufficient to administer the MMSE and UPDRS in addition to other routine medical tests. In addition, the only on-site neurologist participating in the project (NR) had to make a considerable effort to examine the 145 patients who passed to Step 3, a much higher number than expected. Nonetheless, these obstacles can be addressed with improvements in the screening protocol (see discussion) and the central health authorities in San José are keen to extend this pilot experience.
Discussion
This study assessed the feasibility of an early detection system of neurodegenerative disease among the elderly in the Costa Rican public health system. Development of such a system would have significant public health implications and is in line with the goals of WHO and the GCGMH (Citation1–(Citation5)).
The tiered three-step approach allowed evaluation of a number of simple tests for a future governmental screening program in this field. We used broad criteria for failure in Step 1 to try to avoid false negatives and to be able to reasonably estimate the prevalence of neurodegenerative diseases in this population during Step 3. The overall motor and cognitive failure criteria at this first screening level lacked specificity (respectively 23% and 29% only), which resulted in too many patients passing on to Step 2 to be manageable on a larger scale.
The main problem in Step 2 was the time required for even the abbreviated UPDRS test and the MMSE test. We needed to double the allotted time to examine the elderly. Although the sensitivities and specificities of the UPDRS and MMSE were acceptable to good, the large number of patients examined in Step 2 and the low PPV of the UPDRS caused more patients than expected to pass on to Step 3. This passage rate would overwhelm the neurologist's service in a large-scale endeavor.
Considering these results, we examined different cutoff points that would increase the specificity without lowering the sensitivity of Step 1 tests too much, and assessed the possibility of simplification of the Step 2 tests to shorten administration time. With regard to the motor component of Step 1, although changes in cutoff points for subtests and overall failure criteria considerably improved the specificity (data not shown), a more effective solution is to eliminate Step 1 motor tests altogether and, instead, administer the UPDRS as Step 1 and Step 2. Moreover, our results show that when using just the two tremor items (tremor-at-rest and postural tremor), there was only a minimal loss of sensitivity from 100 to 97%, whereas the specificity slightly increased from 76 to 78% (). It seems feasible to train nurses and general physicians in the routine administration of these rather simple test items to all elderly patients attending the CCSS health centers. However, the PPV will still be only 30%, implying that a large number of false positives will be referred for neurological evaluation. The development of an intermediate screening test for tremor-positive patients may therefore be desirable. However, from a public health perspective, based on the results of this study, most of the ‘false positives’ in Step 3 would have other significant and treatable pathologies, in many cases not previously diagnosed.
Table 4 Recommended changes in screening protocol, with parameters of sensitivity, specificity, and positive predictive value (PPV) for new failure criteria in each step, and with an estimated improvement in screening efficiency as compared to the current protocol
With regard to the cognitive component of Step 1, allowing the patients to forget one word in the recall test (as opposed to none in the current study) and maintaining the category fluency test unchanged, the specificity of the overall cognitive failure criteria of Step 1 increased from 29 to 59%, preventing more than 100 false positives from continuing to Step 2 as compared to the current criteria (). On the downside, 19 abnormal MMSE would be missed, with five MCI (14%) and one AD (5%) cases among them. For Step 2, the sensitivity and specificity of MMSE are good and few false positives continued to Step 3. Although age and education significantly predicted the MMSE score in our data, little was gained in prediction by setting a lower failure cutoff point (score <23) for patients over age 80 or with low literacy.
Not all patients who entered Step 1 had a Step 2 test or a final Step 3 diagnosis, limiting our ability to estimate true sensitivity and specificity for one step regarding the next. This is inevitable in a real-world situation where time is of the essence and medical staff cannot evaluate in a later step those who were negative in a previous one. In calculating sensitivity and specificity, we have included in the denominator of Step 2 and Step 3 the patients who had scored negatively in Step 1 and Step 2 (24 and 199, respectively), under the assumption that they were healthy. Although reasonable, this implies some inevitable misclassification of impaired persons as healthy.
With the high sensitivities for Step 1 and Step 2 failures and the likely low number of missed cases, the project allowed the estimation of the prevalence of neurodegenerative disorders in the study population, which was considerably higher than expected for PD and about as expected for AD. The number of PD cases detected was almost double the cases of AD, although AD is a more common disease than PD (Citation24). Likewise, essential tremor was less prevalent than PD in the examined population. Prevalence depends on the quality of the diagnosis, but the diagnoses were made on the basis of established criteria. It is possible that AD may have been more present in the 20% of the target population that never came to the health center, or among the 33 patients lost to follow-up in Step 2 and Step 3. The association in our study between pesticide exposure and PD (Citation10) could partially explain our findings of a high prevalence of PD.
The CCSS aspires to address chronic neurodegenerative diseases through a national screening program linked to an existing priority program on non-communicable diseases within the primary healthcare system, as advocated by WHO and the GCGMH initiative (Citation1–(Citation5)). Such a system will be linked to interventions and research. CCSS, in fact, is dedicating considerable resources to reach these goals. The patients diagnosed with a neurodegenerative disease in this study are now part of an intervention program. Furthermore, since this project was conducted, two national dementia associations have been established and Costa Rican clinicians at CCSS have joined the 10/66 Dementia Research Group of Alzheimer's Disease International (http://www.alz.co.uk/1066/research.php), the latter not only addressing patients’ needs but also that of caretakers. We conclude that a routine screening program in the public health system of Costa Rica is feasible and can lead to improved care, research, and preventive actions. To our best knowledge, such a screening program would be the first worldwide.
Conflict of interest and funding
The project was supported by Award Number P01ES016731 from the National Institute of Environmental Health Sciences. The content is solely the responsibility of the authors and does not necessarily represent the of ficial views of the National Institute of Environmental Health Sciences or the National Institutes of Health.
Acknowledgements
The authors are grateful for the support and work of the staff at the Social Security of Costa Rica (CCSS), Drs. Marco Salazar Rivera, José Miguel Rojas Hidalgo, and Alexander Parajeles; the physicians, nurses, and medical registrars at the EBAIS of Santo Tomás and Los Ángeles. We thank Rebeca Alvarado, Angie Vargas, and Raquel Acuña for their assistance in data collection and administrative matters, and Dr. Seth Pullman for his guidance in the computerized spiral drawings. We thank the patients of the EBAIS of Santo Tomás and Los Ángeles who participated in the testing.
References
- World Health Organization. Neurological disorders: public health challenges. 2006; Geneva: WHO Press. ISBN 92 4 156336 2 (NLM classification: WL 140), ISBN 978 92 4 156336 9..
- World Health Organization. Alzheimer's Disease International. Dementia. A public health priority. 2012; Geneva: WHO Press. ISBN 978 92 4 156445 8.
- Collins PY , Patel V , Joestl SS , March D , Insel TR , Daar AS , etal. Grand challenges in global mental health. Nature. 2011; 475: 27–30.
- Collins PY , Insel TR , Chockalingam A , Daar A , Maddox YT . Grand challenges in global mental health: integration in research, policy, and practice. PLoS Med. 2013; 10: 1001434.
- Kristiansen C. Mental health must be integrated into care delivery. Fogarty International Center, National Institutes of Health, Department of Health and Human Services, Global Health Matters 2013. 6–9. Available from: http://www.fic.nih.gov/News/GlobalHealthMatters/july-august-2013/Documents/fogarty-nih-global-health-matters-newsletter-july-august-2013.pdf [cited 1 October 2013]..
- World Health Organization. Global health observatory data repository: life expectancy. 2013. Available from: http://apps.who.int/gho/data/view.main.680?lang=en [cited 15 August 2013]..
- Instituto Nacional de Estadísticas y Censos. Estimaciones y proyecciones de población por sexo y edad, 1950–2050 [Population estimates and projections by sex and age, 1950–2050]. 2013; San José, Costa Rica: INEC.
- Sáenz Mdel R , Acosta M , Muiser MJ , Bermúdez JL . Sistema de salud de Costa Rica [The health system of Costa Rica]. Salud Publica Mex. 2011; 53(Suppl 2): S156–67.
- ESPAM. I Informe del estado de la situación de la persona adulto mayor en Costa Rica. Capítulo 7, Uso y acceso a los servicios de salud [Ist Report on the state of the situation of the elderly in Costa Rica. Chapter 7, Use and access to the health services]. 2008; San José, Costa Rica: Proyecto Estado de la Situación de la Persona Adulto Mayor (ESPAM).
- Steenland K , Wesseling C , Román N , Quirós I , Juncos JJ . Occupational pesticide exposure and screening tests for neurodegenerative disease among an elderly population in Costa Rica. Environ Res. 2013; 120: 96–101.
- Pullman SL . Spiral analysis: a new technique for measuring tremor using a digitizing tablet. Mov Disord. 1998; 13: 85–9.
- Saunders-Pullman R , Derby C , Stanley K , Floyd A , Bressman S , Lipton RB , etal. Validity of spiral analysis in early Parkinson's disease. Mov Disord. 2008; 23: 531–7.
- Clinical Motor Physiology Laboratory. Diagnostic tests of motor function. Spiral drawing. 2006. Available from: www.cmpl.columbia.edu/diagnostic.html [cited 15 August 2013]. Department of Neurology, Medical Center, Colombia University.
- Louis ED , Tang MX , Mayeux R . Factor structure of Parkinsonian signs in the community-dwelling elderly. Mov Disord. 2004; 19: 268–72.
- Blesa R , Pujol M , Aguilar M , Santacruz P , Bertran-Serra I , Hernández G , etal. for the NORMACODEM Group. NORMAlisation of Cognitive and Functional Instruments for DEMentia. Clinical validity of the ‘mini-mental state’ for Spanish-speaking communities. Neuropsychologia. 2001; 39: 1150–7.
- Llibre Jde J , Fernández Y , Marcheco B , Contreras N , López AM , Otero M , etal. Prevalence of dementia and Alzheimer's disease in a Havana municipality: a community-based study among elderly residents. MEDICC Rev. 2009; 11: 29–35.
- Lopes MA , Ferrioli E , Nakano EY , Litvoc J , Bottino CM . High prevalence of dementia in a community-based survey of older people from Brazil: association with intellectual activity rather than education. J Alzheimers Dis. 2012; 32: 307–16.
- Hughes AJ , Daniel SE , Kilford L , Lees AJ . Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992; 55: 181–4.
- McKhann GM , Knopman DS , Chertkow H , Hyman BT , Jack CRJR , Kawas CH Jr , etal. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011; 7: 263–9.
- Woodruff BK . Disorders of cognition. Semin Neurol. 2011; 31: 18–28.
- Albert MS , DeKosky ST , Dickson D , Dubois B , Feldman HH , Fox NC , etal. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011; 7: 270–9.
- de Lau M , Breteler M . Epidemiology of Parkinson's disease. Lancet Neurol. 2006; 5: 525–35.
- Brookmeyer R , Evans DA , Hebert L , Langa KM , Heeringa SG , Plassman BL , etal. National estimates of the prevalence of Alzheimer's disease in the United States. Alzheimers Dement. 2011; 7: 61–73.
- Nussbaum RL , Ellis CR . Alzheimer's disease and Parkinson's disease. N Engl J Med. 2003; 348: 1356–64.
Annex 1
Screening parameters according to different failure criteria and cutoffs for tests of cognition and motor control used in Step 1 and Step 2 of the screening protocol in relation to final diagnosis of Alzheimer's disease (AD), mild cognitive impairment (MCI), or Parkinson's disease (PD): sensitivity (sens), specificity (spec), positive predictive value (PPV), negative predictive value (NPV), false positive rate (FPRate), and false negative rate (FNRate)