Abstract
Background
Most low- and middle- income countries are facing a rise of the burden of non-communicable diseases (NCDs) alongside the persistent burden of infectious diseases. This narrative review aims to provide an inventory of how the existing policy environment, health system, and communities are addressing the NCDs situation in Tanzania and identify gaps for advancing the NCD research and policy agenda.
Methodology
A literature search was performed on PubMed and Google scholar with full text retrieval from HINARI of English language articles published between 2000 and 2012. Documents were read to extract information on what Tanzanian actors were doing that contributed to NCDs prevention, treatment, and control, and a narration was written out of these. Reference lists of all retrieved articles were searched for additional relevant articles. Websites of organizations active in the field of NCDs including the Government of Tanzania and WHO were searched for reports and grey literature.
Results
Lack of a specific and overarching NCD policy has slowed and fragmented the implementation of existing strategies to prevent and control NCDs and their determinants. The health system is not prepared to deal with the rising NCD burden although there are random initiatives to improve this situation. How the community is responding to these emerging conditions is still unknown, and the current health-seeking behavior and perceptions on the risk factors may not favor control of NCDs and their risk factors.Footnote
Conclusion and recommendation
There is limited information on the burden and determinants of NCDs to inform the design of an integrative and multisectorial policy. Evidence on effective interventions for NCD services in primary care levels and on community perceptions on NCDs and their care seeking is virtually absent. Research and public health interventions must be anchored in the policy, health system, and community platforms for a holistic response.
Responsible Editors: Nawi Ng, Umeå University, Sweden; Barthélémy Kuate Defo, University of Montreal, Canada.
This paper is part of the Special Issue: Epidemiological Transitions – Beyond Omran’s Theory. More papers from this issue can be found at http://www.globalhealthaction.net
Tanzania%26apos%3Bs population of 44.9 million in 2012 is more than three times the 12.3 million estimated in 1967 (Citation1). The population growth rate is estimated at 2.7% annually with a crude birth rate of 12.9 per 1,000 inhabitants. The fertility rate at 5.4 children per woman in 2012 is a drop from the 6.5 and 6.3 children per woman estimated in 1988 and 2002 respectively, but is still very high and contributes to the rapid increase in population (Citation1). The Tanzanian demographic profile, like that of other low- and middle-income countries, is largely young, with 42.5% of the population being younger than 15 years, 51.9% between 15 and 59 years, and 5.6% aged 60 years or older (Citation1). The increasing life expectancy at birth from 50 years in 1988 to 55 years in 2010 (Citation2) is, however, changing this picture by slowly increasing the middle-aged and older populations. This improved survival has been attributed to improved health standards and hence reduced mortality (Citation3). Eighty percent of Tanzania%26apos%3Bs population lives in rural areas (Citation1), and the adult literacy level was 71% in 2010 (Citation4). Tanzania%26apos%3Bs gross national income per capita was USD 551 in 2010 (Citation4), making it one of the poorest countries worldwide. Health sector spending amounted to 7% of the national gross domestic product in 2011 (Citation5), with the government contributing to 53% of all health expenditure in 2010/11 fiscal year (Citation6).
Tanzania has for decades struggled with the burden of infectious and deficiency disorders along with poor maternal and child health indicators. Successes have been documented in the form of a steady decline of the maternal mortality ratio from 529 deaths in 1996 to 452 deaths per 100,000 live births in 2010 (Citation4); and the under-5 mortality ratio from 137 in 1978 to 81 deaths per 1,000 live births in 2010 (Citation4). Malaria attributable child mortality decreased from 53 in 1999 to 36 in 2007%26ndash%3B2008 (Citation7, Citation8), a reduction in HIV prevalence among persons aged 15 to 49 years was seen from 7% in 2003%26ndash%3B2004 to 5.1% in 2012 (Citation9, Citation10), and evidence of the impact of antiretroviral treatment on population mortality has been documented (Citation11). Although these efforts are ongoing amidst resource constraints (Citation2), the rising prevalence of degenerative non-communicable diseases (NCDs) is exerting further strains on the meager resources.
In 2010, NCDs were responsible for 27% of all deaths in Tanzania (Citation12), a figure that is comparable to that of neighboring countries like Mozambique (Citation13). As in the rest of the world, cardiovascular diseases, cancers, diabetes, and chronic obstructive respiratory diseases (CORDs) have been highlighted as main contributors to premature mortality (Citation14). In 2012, the prevalence of hypertension in Tanzanian adults of 25%26ndash%3B64 years of age was 26% and that of raised fasting blood glucose in the same population was 9.1% (Citation15). Findings of a study conducted in selected rural and urban communities in Tanzania in 2003 found that crude yearly stroke incidences were 95 per 100,000 and 107.9 per 100,000, respectively (Citation16). Despite this shrinking rural%26ndash%3Burban difference in burden, it has been found that the availability of NCD diagnostic and management services is twice as much in urban compared to rural areas (Citation17). National representative data on heart diseases, cancers, and CORDs could not be obtained. These NCDs are reported to share four main risk factors: poor dietary habits, excessive alcohol use, tobacco use, and lack of physical exercise (Citation18).
The health system is anchored on 5,416 health facilities, at an average ratio of 1.5 facilities per 10,000 persons, with dispensaries being the point of first contact for the majority of the population. Two-thirds of facilities are government-owned, and 236 of the facilities are of hospital level and above (Citation19). The provider to population ratio in 2012 was 7.1 per 10,000 population including only professional health workers. Efforts to tackle infectious diseases have been targeting the health system, policies, and the community, which are important constituents of any health sector response. This paper is an inventory of how the policy environment, health system, and communities are addressing the NCDs situation. It highlights the ways to adapt these platforms for responses to the increasing burden of NCDs and identifies the knowledge gaps for advancing the research and policy agendas for NCDs in Tanzania.
Methodology
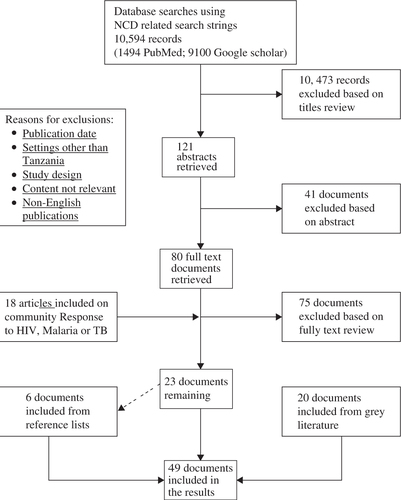
A literature search was performed using a set of comprehensive topic-related search terms. Inclusion criteria were English-written articles on original work conducted in Tanzania. We excluded systematic or narrative reviews, opinion papers, documents including expectant women as participants, and articles on drug evaluations and diagnostics. The search was restricted to publications between 1 January 2000 and 31 December 2012 to ensure that the retrieved articles reflected the current situation and most recent responses. The search was performed on PubMed and Google scholar, with full text articles retrieved from HINARI. We also undertook targeted grey literature search, focusing on large institutions including WHO, NCD interest groups in Tanzania, and documents and reports of the government of Tanzania. Articles selected included primary research articles, evaluation, and situation analyses reports. The references of retrieved articles were manually searched for additional material. The search terms were based on key terms aligned to policy, health care system, and community, the important constituents of a health sector response (Citation20). The terms were combined by Boolean operators %26lsquo%3BAND%26rsquo%3B to narrow the search appropriately and %26lsquo%3BOR%26rsquo%3B to expand it with similar terms. The search strategy included the following strings: %26lsquo%3Bnon-communicable diseases%26rsquo%3B OR %26lsquo%3Bnon communicable diseases%26rsquo%3B OR %26lsquo%3BNCDs%26rsquo%3B AND Tanzania; %26lsquo%3Bnon-communicable diseases%26rsquo%3B OR %26lsquo%3Bnon communicable diseases%26rsquo%3B OR %26lsquo%3BNCDs%26rsquo%3B AND health services OR health care AND Tanzania; %26lsquo%3Bnon-communicable diseases%26rsquo%3B OR %26lsquo%3Bnon communicable diseases%26rsquo%3B OR %26lsquo%3BNCDs%26rsquo%3B AND health seeking OR health-seeking AND Tanzania; %26lsquo%3Bnon-communicable diseases%26rsquo%3B OR %26lsquo%3Bnon communicable diseases%26rsquo%3B OR %26lsquo%3BNCDs%26rsquo%3B AND policy AND Tanzania. The search resulted in 10,594 articles as depicted in . Ten thousand, four hundred and seventy-three of these were excluded for reasons including title not focused on NCDs, language other than English, or publication date was out of target. One hundred and twenty-one titles were found to be relevant to our subject area and their abstracts were retrieved and screened to determine if they matched our criteria. Forty-one abstracts were excluded based on content relevance to our topic and study design. From this step, 80 abstracts were identified to be relevant and their full text versions were retrieved from HINARI. Bibliographies of retrieved documents were also searched for relevant papers. Six documents were identified this way, three of which were peer-reviewed articles, and the other three were reports. When our initial search yielded only two papers on community responses to NCD, we expanded our inclusion criteria to include articles on health seeking for HIV, TB, or malaria. We obtained 18 relevant publications based on this expansion.
Analysis was done based on pre-determined themes on NCD policy prevention and control, health system financing, NCD health services, and human recourses of health regarding NCD services and community health-seeking behavior and practices. These themes were pre-determined taking into account the review objectives and focused on the main health sector response constituents. Documents were handled manually in that no data management software was used during the analysis. They were read to extract information on what Tanzanian actors were doing that contributed to NCDs prevention, treatment, and control, and a narration was written out of these responses. There were discussions among the first four authors on content of the results and in case of disagreements resolution was by consensus.
Results
This review included 49 documents that were comprised of 26 peer-reviewed articles which were mainly cross-sectional studies published between 2006 and 2012. Three of the 26 articles are included in the policy section, one in the health systems section, and 22 in the community section. The other 23 documents were grey literature mainly from the Tanzanian government and WHO sources, published between 2001 and 2012. Six of these documents were reviewed for the policy section, 17 for the health system, and none was reviewed for the community section. Three of the six documents obtained through searching the reference lists of retrieved articles were peer-reviewed articles, the remaining were grey literature. In these results the NCD-related policy environment is described first and then the preparedness of the health system for the rising NCD burden. This will be followed by an inventory of community responses to NCDs.
Policies and strategies on NCDs and their determinants in Tanzania
The government has established a unit at the Ministry of Health and Social Welfare (MoHSW) to steer formulation of NCD policies and guidelines (Citation21). It has also included prevention and control of NCDs as strategic objectives of the health sector (Citation7). This National Strategy for NCDs 2008%26ndash%3B2013 identifies primary, secondary, and tertiary prevention as important components in addressing NCDs (Citation7). The strategy is integrated and generic and addresses NCDs only from the health sector perspective (Citation7, Citation12). There was neither an overarching national NCD policy nor evidence of harnessing of non-health sectorial policies in the current response to NCDs despite the multifaceted etiologies of these diseases. Regarding addressing of the four main risk factors of NCDs, by 2011, Tanzania had integrated strategies for alcohol; smoking; physical inactivity; and unhealthy diets, overweight, and obesity (Citation12).
The government signed (in 2004) and approved for implementation (in 2007) the WHO%26apos%3Bs Framework Convention for Tobacco Control (FCTC) (Citation22). This convention clearly presents both demand and supply reduction provisions for controlling exposure to tobacco, among other provisions (Citation23). Fortunately, some of its demand%26ndash%3Breduction provisions such as the introduction of excise taxation on tobacco were already in place (Citation24), but still more actions are needed considering that smoking tobacco costs the nation more than 30 million dollars annually in treatment of tobacco-related cancers (Citation25). In 2011, it was reported by WHO that Tanzania had implemented none of the five tobacco (m)POWER measures to the highest level of achievement (Citation12). Concerning control of the use of alcohol, Tanzania%26apos%3Bs alcohol policy includes excise taxes on alcohol, a minimum drinking age of 18, a zero tolerance policy for drinking and driving, regulations on alcohol advertising and sponsorships, and restrictions for on- and off-premise sales of alcoholic beverages (Citation26).
The scope of the current Tanzania National Nutrition Strategy states: the strategy seeks to ensure the nutritional status of all citizens of Tanzania throughout their life cycle (Citation27). However, the strategy focuses more on women of reproductive age and children under 5 years of age with special emphasize on children less than 2 years of age because malnutrition%26apos%3Bs most serious and lasting damage occurs during pregnancy and the first two years of life. None of the targets set are related to NCDs or their dietary risk factors.
There was no policy on physical exercise that was found other than a reference to a policy on physical education in schools (Citation28).
Health systems and the response to NCDs in Tanzania
In Tanzania, health services for NCDs are mostly provided from district hospitals to higher level health facilities (Citation29). In 2010, the public health system had only two out of eight NCD-related screening and diagnostic tests nationwide (cervical cancer screening and breast cancer screening) at primary level facilities (Citation21).
In regards to medications, by 2009, the problem of stock-outs for all drugs including for NCDs was persistent and was associated with poor health outcomes, especially for those who could not access services in the private facilities (Citation30). In 2010, 15 out of 17 NCD-related drugs were available in public health system (Citation21).
The Human Resource for Health (HRH) deficit in Tanzania stood at 65% in 2008 (Citation7, Citation19). With the projected increase of the NCD burden, the government is re-thinking its HRH management strategies (Citation7, Citation19). The immediate strategy involves capacity building of HRH for NCD care in the form of in-service trainings offered by various disease-interest groups (Citation29, Citation31) such as the Tanzania Diabetes Association which has trained staff from even lower level facilities in the Lake Region (Zachariah Ngoma, personal communication, 26 March 2013). The introduction of NCD prevention and control modules into courses in local training institutions (Citation32) is availing the training to a wider pre-service trainee population, which may help to build the HRH pool of different cadres for the future. The Association of Private Health Facilities in Tanzania (APHFTA) has conducted in-service trainings for diabetes and hypertension care in 18 out of 27 regions of Tanzania (Citation33). In the public health system, comprehensive clinical guidelines have been developed only for diabetes and hypertension (Citation21) but evidence for their distribution, training, and utilization is limited.
Currently, both health facility and population-based information systems reflect limited measurement of NCD-related variables (Citation34, Citation35). The standards of Health Management Information System (HMIS) in Tanzania are slowly improving with efforts underway to minimize the existing challenges in quality and utilization of health information and to expand information sources such as the cancer registry (Citation36). For population-based NCD information to inform policy and other interventions, the MoHSW resorted to search for evidence on NCDs and their risk factors through projects. The National Institute for Medical Research conducted WHO STEP wise approach to chronic disease risk factor surveillance (WHO STEPs survey), to quantify the risk factors and burden for NCDs (Citation15) nationally. Variables for NCD risk factors have been included in the Tanzania demographic health surveys (DHS) tool (Citation34) and into the MZIMA adult health community cohort (Citation37). There is lack of literature on utilization of even wider existing platforms such as the sentinel Panel of Districts (SPD) (Citation38).
Underfunding of health services is a persistent challenge contributing to a myriad of other malfunctions in the system (Citation39). As a signatory of the Abuja declaration 2001 which required Governments to allocate at least 15% of its annual budget to health sector, Tanzania allocated 8.9% for the 2011%26ndash%3B2012 fiscal year (Citation40). Financing of health care is through, among others, health insurance mechanisms including community health funds that are being rolled out, though uptake is reported to be low (Citation41). Integration of services is one way to deal with NCDs proposed in the Health Sector Strategic Plan III and provides a cost-efficient means of quality service delivery (Citation7). The government has collaborated with other stakeholders in a private hospital in Dar es Salaam whereby NCD services were introduced in the HIV clinic and staff trained in management of co-morbidities. In 2011, this initiative was evaluated and results showed that 15% of its 3,400 patients on antiretroviral therapies had co-morbidities including hypertension, hyperlipidemia, diabetes, and other metabolic disorders (Citation42). Other NCD-related programs that attest to advantages of private%26ndash%3Bpublic partnership include the Ocean Road Cancer Institute, and the APHFTA (Citation33, Citation43).
Communities in preventive health and health care seeking
In public health, community involvement is key to achieving the goals of preventive and promotional health programs (Citation44). In Tanzania the importance of involving communities in effective disease control interventions for various infectious diseases has been well documented (Citation45). This practice was associated with increased access and acceptance of palliative services (Citation46), effectiveness and efficiency of disease control interventions (Citation47), as well as equity, sustainability, and communities%26rsquo%3B self-reliance (Citation48). Private facility initiatives such as those under APHFTA through their NCD program, involved primary schools and communities around health facilities reached by their program in healthy lifestyle teachings including healthy eating and physical activities (Citation33). The impact of these interventions however, is not yet known.
Factors contributing to development of NCDs include social determinants which are highly linked to complex sociocultural practices and beliefs, making it challenging to effect lifestyle changes (Citation49). For example, fatness was associated with beauty and economic prosperity of the household (Citation50); and excessive alcohol intake was fuelled by cheaply available local brew, and the need for entertainment and relaxation on the part of users (Citation51).
Literature suggests that where illness symptoms were thought to have spiritual etiology, traditional healers became the preferred source of treatment (Citation52, Citation53) (Citation54) , because they were perceived to have %26lsquo%3Bappropriate skills%26rsquo%3B for managing diseases considered as out of order (Citation55).
Socioeconomic determinants have been shown to influence the timeliness of peoples%26rsquo%3B responses to the utilization of emergency and in-patient services (Citation56) and the initiation and continuation of treatments for chronic illnesses (Citation55), all of which influence patient outcomes (Citation57). Studies revealed that services at health care facilities are only sought when chronic illness symptoms persist or worsen, after using over-the-counter medicines (Citation58, Citation59). In addition, accessibility to health facilities has been shown to facilitate prompt care seeking (Citation60) and continuity of care for chronic illnesses (Citation61).
Several factors influence adherence to treatments to infectious disease in Tanzania including; people%26apos%3Bs perceptions of the illness and quality of medicines (Citation62), fear of side effects (Citation63), patient%26ndash%3Bprovider relationships, cultural pressure, cost and availability of medicines (Citation61), and the patient%26apos%3Bs understanding of the medication schedule (Citation64). Others include poor access of re-filling prescriptions, inadequate nutrition especially for medicines perceived to increase hunger (Citation63), and long hours of absence from home (Citation65). Adherence to medications was reported to also be influenced by gender (Citation65).
Discussion
Our findings have shown that there is no existing NCD policy in Tanzania. For clarity of vision and purpose and coherence of interventions, a national policy is important (Citation66, Citation67). Reasons for lack of a policy include the lack of evidence to inform such a policy (Citation67). There are several opportunities in available guidelines and strategies for controlling exposure to the major NCD risk factors, implementation of which is partly hampered by lack of an NCD policy. Being multifaceted in their etiology, NCD policies being designed must as well be multisectorial. In Tanzania, there was no evidence of including other sectors such as education and agriculture in policy development for NCD prevention and control. The country could learn from experiences shaping the HIV response where multisectoral approaches have been adopted in prevention and communication activities (Citation68). Regarding prevention of exposure to NCD risk factors, the adoption and implementation of FCTC is a positive step towards tobacco control. However, more effort is needed towards fully implementing the convention through the mPOWER measures.
Although some aspects of alcohol policy are in place, implementation of these, especially in rural areas where local brew is mostly produced and consumed, will be a challenge (Citation68). Addressing diet-related NCDs in the national nutrition strategy without setting targets related to NCDs or their dietary risk factors indicates that overnutrition is not yet prioritized. Whereas there are still no policies focusing on physical activity, it has been proposed that the policies will have to address activity at work places, leisure activities, and means of transport (Citation69). Physical activity policies should also be sensitive to sociocultural differences across Tanzania.
As policies are being developed to tackle the rising NCD burden, the health system in Tanzania must gear up for roles in primary, secondary, and tertiary prevention of NCDs. Concentration of the NCD services at higher level health facilities leads to late diagnosis and delayed access to appropriate treatments, especially in rural areas (Citation70). Accessibility of NCD services also entails availability of diagnostic and treatment services at the primary level facilities. Lack of screening and diagnostic tests at primary level facilities creates a challenge for NCD care, especially the long-term patient monitoring and management. Whereas the WHO observatory indicates that NCD medication availability was impressive, it is the consistent medical supply of affordable medicines that contributes to favorable health outcomes. A recent national survey in Tanzania showed that, only 9% of rural and 20% of the urban health facilities provided diabetes diagnosis and management services and only half of these had the staff, drugs, diagnostics, and guidelines to actually provide the service on the day of the survey (Citation17). Generally the health care system is not prepared to tackle the rising burden of NCDs (Citation17, Citation71). The HRH crisis hinders quality preventive, diagnostic, and treatment service provision for NCDs close to the community and requires creative thinking on how to more efficiently use the existing HRH. The pre-service and in-service training efforts, though prudent, do not completely address the shortage of competent cadres in lower level facilities in the country. Creativity including task shifting where lower cadres of HRH are prepared for NCD prevention and management could ease this crisis as has been done elsewhere (Citation72). Availing tools such as clinical guidelines has facilitated task shifting and could be adopted in Tanzania%26apos%3Bs primary care facilities (Citation72).
The rising burden of NCDs will increase the financial strain on the health system because of their chronic nature; hence, new approaches to minimize costs of interventions must be embraced. Integration ensures that, %26lsquo%3Bclients receive a continuum of preventive and curative services, according to their needs over time and across different levels of the health system%26rsquo%3B (Citation73).Various integration models are possible, but little has been documented on pilot projects. The benefits of integration of services that have been observed in the Tanzanian example have been demonstrated in other settings where chronic diseases clinics have been piloted (Citation74). This idea of chronic disease clinics could be replicated in primary care settings where HIV prevention, care, and treatment services are offered.
Improvement of HMIS would positively influence quality of care for NCD patients and overall health system functioning (Citation75). Systematic information concerning public awareness and practices regarding NCD risky behaviors as well as factors that shape risky lifestyle is still limited. Existing population survey platforms such as the demographic surveillance system and SPD could be adapted to fit chronic disease surveillance by introducing outcome measures that realistically measure morbidity burden of NCDs. Mortality outcomes may not capture true burden of NCDs whose onset and course is insidious.
The financial strains caused by NCDs are also experienced by patients and their families. Ensuring effective implementation of the policy on health care fee waivers which exempts patients with chronic diseases from user fee charges will improve accessibility and equity in utilization of NCD services. However, this has implications to the government resources and may necessitate government%26apos%3Bs re-allocation of its financial resources to the health sector.
Considering that NCDs are insidious in their onset, slow in their progression, and long-term, communities have to be involved in their prevention and control (Citation76). Community involvement has been shown to be effective in other chronic diseases prevention and control efforts (Citation77, Citation78). This involvement has also been recommended in the Tanzania HSSP III as an objective in the NCD control strategy (Citation7). Since community responses, including lifestyle changes, are shaped by sociocultural aspects and health system factors, effective mitigation of NCDs will therefore have to integrate community-based and individually targeted interventions (Citation79) that are sensitive to variations in gender and cultural norms, for them to be acceptable (Citation80).
Knowing that health services are commonly sought when illnesses persist or worsen after failure of self-medication, interventions to promote prompt health care seeking must be designed. Self-medication may present a challenge when it comes to NCDs, most of which are initially asymptomatic and symptoms indicate worsening of disease intensity. Information is lacking on NCD self-treatment patterns and their motivations, which may hinder the possibility of addressing any undesirable patterns in the community.
As NCD medication use is long-term, it is important to understand how sociocultural aspects shape people%26apos%3Bs sustained compliance to medicines. Compliance to long-term medication has been studied for infectious chronic diseases (Citation81, Citation82); however, community perceptions towards infectious disease and NCDs may not be the same. Therefore application of the findings from these studies to NCDs medication may not be valid. Exploration of the aspects that might shape sustained compliance to long-term NCDs medication would inform designing of strategies that foster compliance to long-term treatments.
The knowledge gaps for both research and policy agendas regarding responses to the rising NCDs burden in Tanzania include inadequate information on the epidemiological patterns of NCDs and their determinants across Tanzania and the limited awareness of the local context to inform the design of an integrative and multisectorial policy. Apart from better understanding the epidemiological pattern of NCDs, it will be important to project the implications of the current dual burden on population life expectancy, taking into account not just the health systems and policy environment, but also the wider demographic and development indicators. There is limited evidence on effective interventions for NCD services in primary care levels and information on community perceptions on NCDs and their care seeking is virtually absent.
Limitations and strength of the review
This review included mainly published documents and thus omitted insights from non-published developments. Through the inclusion of only English language documents we might have missed relevant results published in Kiswahili. However, a Kiswahili language research journal does not exist in Tanzania and English is one of the country%26apos%3Bs official languages. We therefore think that this has not resulted in non-inclusion of formal government- produced documents nor of research publications. The search terms did not include %26lsquo%3Bchronic disease%26rsquo%3B because not all chronic diseases are NCDs. We thus may have missed articles that used only %26lsquo%3Bchronic disease%26rsquo%3B as a term to describe NCDs. Nevertheless, the holistic nature of the information reviewed provides a broader view of the NCDs situation and the responses in Tanzania. The narrative review approach was chosen rather than a systematic review because it is well suited to present a broad perspective on a newly emerging problem (Citation83, Citation84).
Conclusions and recommendations
NCDs and their risk factors are largely lifestyle related, making multisectorial responses unavoidable. These conditions are posing a critical challenge to the government, health system, and communities that have to face both communicable and NCDs. There is limited context-relevant information on the burden and determinants of NCDs which may hamper the design of effective interventions, especially for prevention. The existing research platforms such as the health and demographic surveillance system (HDSS), DHS, and SPD can be leveraged to address these NCD knowledge gaps.
Current efforts to address NCDs in Tanzania are fragmented due to lack of a NCD policy. The success of NCD prevention and control requires such a clearly defined NCD policy to provide a roadmap for implementation of multisectoral strategies and plans. For effective interventions targeting NCDs risk factors at local level, empowerment of local government authorities tasked with implementation of existing policies in the country is needed.
The country%26apos%3Bs health system is not adequately prepared to accommodate the requirements of NCDs. There is an urgent need to design and evaluate low-tech, low-cost interventions for prevention, diagnosis, treatment, and continuity of care that can be scaled up at primary care levels. This may necessitate the adoption of an integrated health care model to address both NCDs and other chronic communicable diseases as a strategy to address the HRH and financing challenges. Also, supporting informed decision making for NCDs at clinical and policy levels requires accurate clinical record keeping and diseases registry maintenance for NCDs and their risk factors.
Information on community awareness and practices in prevention and health care seeking regarding NCDs is limited. The role of the community in NCD development, prevention, and management must be explored by understanding the motivations for health-seeking, self-medication practices, and aspects shaping continuity of care in their particular contexts.
Main findings
There is limited context-relevant information on the epidemiological patterns of non-communicable diseases (NCDs) and their determinants across Tanzania; this may hamper the design of effective interventions, especially prevention.
Current efforts to address NCDs in Tanzania are fragmented due to a lack of a NCD policy.
The county’s health system is not adequately prepared to accommodate the requirements of NCDs and the information on community awareness, practices in prevention and health care seeking regarding NCDs is limited.
Key messages for action
The existing research platforms such as the health and demographic surveillance system (HDSS), demographic health surveys (DHS) and the sentinel panel of districts (SPD) should be leveraged to address the knowledge gaps in epidemiological patterns, in best practices in health care and in community roles in prevention and management of NCDs in Tanzania.
Considering the multifaceted nature of NCD risk factors and causation, there is a need to formulate a clear, multi-dimensional policy on NCDs prevention and management.
There is an urgent need to design and evaluate low-tech, low-cost interventions for prevention, diagnosis, treatment and continuity of care that can be scaled up at primary care levels. This may include the adoption of an integrated health care model to address both NCDs and other chronic communicable diseases as a strategy to address the HRH and financing challenges.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
Acknowledgements
This review was supported by grants from the Netherlands Organization for International Co-operation in Higher Education and the Ifakara Health Institute, Tanzania.
Notes
Responsible Editors: Nawi Ng, Umeå University, Sweden; Barthélémy Kuate Defo, University of Montreal, Canada.
This paper is part of the Special Issue: Epidemiological Transitions – Beyond Omran’s Theory. More papers from this issue can be found at http://www.globalhealthaction.net
EM, BM, MM, and DJN claim equal authorship.
References
- NBS, OCGS. Population and Housing Census Report. Population Distribution by Administrative Units; Key Findings. 2013; Dar es Salaam: NBS and OCGS.
- URT. Tanzania Country Report on Millennium Development Goals 2010. 2011; Dar es Salaam: Tanzania Printers.
- REPOA. Delivery of Social Services on Mainland Tanzania. Are people satisfied? AFROBAROMETER Briefing Paper 34. Available from: http://www.repoa.or.tz/documents/AfrobriefNo34.pdf [cited 5 March 2014].
- NBS. National Bureau of statistics, Ministry of Finance, June 2011. 2011; Dar es Salaam: NBS. %26ldquo%3BTanzania in figures 2010.%26rdquo%3B.
- The World Bank. Working for a world free poverty. Available from: http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS [cited 19 November 2013].
- HSER. Directorate of policy and planning, Ministry of Health and Social Welfare, July 2012. %26ldquo%3BHealth Sector Expenditure Review, 2010/11.%26rdquo%3B Dar es Salaam: Tanzania and health systems 20/20 project, Abt Associates Inc; 2010/11.
- MoHSW. Health sector strategic plan III for 2009%26ndash%3B2015: partnerships for delivering MDGs. 2008; Dar es Salaam, Tanzania: M. o. H. S. Welfare.
- Masanja H, de Savigny D, Smithson P, Schellenberg J, John T, Mbuya C, etal. Child survival gains in Tanzania: analysis of data from demographic and health surveys. Lancet. 2008; 371: 1276–83.
- THMIS. Tanzania HIV/AIDs and Malaria Indicator Survey 2011%26ndash%3B12. 2012; Dar es Salaam, Tanzania: NBS.
- Hallett TB, Aberle-Grasse J, Bello G, Boulos L, Cayemittes M, Cheluget B. Declines in HIV prevalence can be associated with changing sexual behaviour in Uganda, urban Kenya, Zimbabwe, and urban Haiti. Sex Trans Infect. 2006; 82: i1–i8.
- Marston M, Michael D, Wringe A, Isingo R, Clark BD, Jonas A, etal. The impact of antiretroviral therapy on adult mortality in rural Tanzania. Trop Med Int Health. 2012; 17: e58–e65.
- WHO. United Republic of Tanzania: NCD country profile 2011. Available from: http://www.who.int/nmh/countries/tza_en.pdf [cited 7 July 2012].
- Silva-Matos C, Beran D. Non-communicable diseases in Mozambique: risk factors, burden, response and outcomes to date. Glob Health. 2012; 8: 37.
- Atun R, Jaffar S, Nishtar S, Knaul F, Lima Barreto M, Nyirenda M. Improving responsiveness of health systems to non-communicable diseases. Lancet. 2013; 20132: 64–71.
- WHO. WHO Tanzania STEPS Survey-2012 Fact sheet. Available from: http://www.who.int/chp/steps/UR_Tanzania_FactSheet_2012.pdf [cited 12 August 2012].
- Walker R, Whiting D, Unwin N, Mugusi F, Swai M, Aris E, etal. Stroke incidence in rural and urban Tanzania: a prospective, community-based study. Lancet Neurol. 2010; 9: 786–92.
- MoHSW. Tanzania service availability and readiness assessment (SARA) 2012. 2013. Dar es Salaam. Dar es Salaam, Tanzania: Ifakara Health Institute.
- Nigatu T. Integration of HIV and noncommunicable diseases in health care delivery in low-and middle-income countries. Prev Chronic Dis. 2012; 9: 1–3.
- MoHSW. Human resource for health strategic plan 2008%26ndash%3B2013. 2008; Dar es Salaam: MoHSW.
- Pruitt S, Annandale S, Epping-Jordan J, Femandez Diaz JM, Khan M, Kisa A. Innovative care for chronic conditions. 2002; Geneva, Switzerland: WHO. Building blocks for action.
- Health systems response and capacity. Global Health Observatory. Available from: http://apps.who.int/ghodata/ [cited 19August 2012].
- WHO. Report card on the WHO framework convention on tobacco control. 2010; Geneva: WHO.
- WHO. Framework convention on tobacco control. 2003; Geneva: World Health Organization, Tobacco Free Initiative.
- Osoro N, Mpango P, Mwinyimvua H. An analysis of excise taxation in Tanzania. 2001; Alexandria, Viginia: EAGER Publications/BHM.
- Kagaruki LK. Community-based advocacy opportunities for tobacco control: experience from Tanzania. Glob Health Promot. 2010; 17: 41–4.
- United Republic of Tanzania (the) Socio economic context. Available from: http://www.who.int/substance_abuse/publications/global_alcohol_report/profiles/tza.pdf?ua=1 [cited 22 June 2012].
- National Nutrition Working Group. National Nutrition Strategy: July 2011/12%26ndash%3BJune 2015/16. Available from: http://scalingupnutrition.org/wp-content/Tanzania_National-Nutrition-Strategy.pdf [cited 13 November 2012].
- Mafuniko FM, Pangani IN. Physical education in Tanzanian secondary schools: perceptions towards physical education as an academic discipline. NUE J Int Educ Coop. 2008; 3: 51–61.
- Ramaiya K. Setting up diabetes clinics in Tanzania. Pract Diabetes Int. 2006; 23: 339–40.
- MoHSW: Ministry of Health %26amp%3B Social welfare TZ. In-depth assessment of the medicines supply system in Tanzania. 2009; Dar es Salaam: MoHSW.
- WHO. WHO country cooperation strategy 2010%26ndash%3B2015, Tanzania. 2009; Brazzaville, Republic of Congo: WHO Regional Office for Africa.
- Diabetes Management Course. Available from: http://www.muhas.ac.tz/Advertisements/short courses/Diabetes course advertisment AUGUST 2012.pdf [cited 15 November 2012].
- Association of Private Health Facilities in Tanzania. Non communicable diseases programme. 2011. Available from: http://www.aphfta.org/index.php?option=com_content%26amp%3Bview=article%26amp%3Bid=115%26amp%3BItemid=154 [cited 25 September 2012].
- TDHS. National Bureau of Statistics (NBS) [Tanzania] and ICF Macro. 2011.Tanzania Demographic and Health Survey 2010. 2010; Dar es Salaam, Tanzania: NBS and ICF Macro.
- TFNC. National nutrition strategy JULY 2011/12 %26ndash%3B JUNE 2015/16. ed. M. o. H. a. S. 2010. Welfare. Dar es Salaam, Tanzania.
- Mwakigonja AR, Loon KV. Proposal to strengthen health information system. 2008. ed. M. o. H. a. S. Welfare. Dar es Salaam: Ifakara Health Research %26amp%3B Development Center, UDSM, MoH%26amp%3BSW, UiO.
- Eveline Geubbels. The Ifakara MZIMA cohort. An open adult health community cohort on chronic diseases. Available from: http://www.ihi.or.tz/a/ihi.or.tz/ihi-main-site/projects/mzima [cited 22 November 2012].
- Sentinel Panel of Districts. A new platform for health monitoring and evaluation in Tanzania Spotlight. Issue 8, October 2011. Available from: http://ihi.eprints.org/1831/1/IHI_Spotlight_-_SPD_Final_Vol_8.pdf [cited 5 March 2012].
- HERA. District health services delivery in Tanzania: where are we in terms of quantity and quality of health care provision?. 2006; Belgium: HERA.
- MOF. Government Budget for Financial year 2011/2012 Citizens Budget Edition. Available from: http://www.opengov.go.tz/files/publications/attachments/CITIZEN_ENGLISH_2011_12_FINAL_en_sw.pdf [cited 24 September 2012].
- Musau S, Chee G, Patsika R, Malangalila E, Chitama D, Praag EV, Bethesda M. Tanzania health system assessment 2010. 2011; Bethesda, Maryland: Health systems 20/20 project. 1–110.
- MSH. Non-communicable and chronic ciseases: a health systems approach. Available from: http://projects.msh.org/resource-center/fact-sheets/upload/NCD-factsheet.pdf [cited 2 June 2012].
- Ocean Road Cancer Institute. Available from: http://www.uicc.org/membership/ocean-road-cancer-institute [cited 6 October 2012].
- Mlozi M, Shayo E, Senkoro K, Mayala B, Rumisha S, Mutayoba B, etal. Participatory involvement of farming communities and public sectors in determining malaria control strategies in Mvomero District, Tanzania. Tanzan Health Res Bull. 2006; 8: 134–40.
- Egwaga S, Mkopi A, Range N, Haag-Arbenz V, Baraka A, Grewal P, etal. Patient-centred tuberculosis treatment delivery under programmatic conditions in Tanzania: a cohort study. BMC Med. 2009; 7: 80.
- Nanney E, Smith S, Hartwig K, Mmbando P. Scaling up palliative care services in rural Tanzania. J Pain Symptom Manage. 2010; 40: 15–18.
- Kisinza W, Kisoka W, Mutalemwa P, Njau J, Tenu F, Nkya T, etal. Community directed interventions for malaria, tuberculosis and vitamin A in onchocerciasis endemic districts of Tanzania. Tanzan J Health Res. 2008; 10: 232–9.
- Mkumbo K, Schaalma H, Kaaya S, Leerlooijer J, Mbwambo J, Kilonzo G. The application of Intervention Mapping in developing and implementing school-based sexuality and HIV/AIDS education in a developing country context: The case of Tanzania. Scand J Public Health. 2009; 37: 28–36.
- Shayo GA, Mugusi FM. Prevalence of obesity and associated risk factors among adults in Kinondoni municipal district, Dar es Salaam Tanzania. BMC Public Health. 2011; 11: 365.
- Maletnlema T. A Tanzanian perspective on the nutrition transition and its implications for health. Public Health Nutr. 2002; 5: 163–8.
- Mbatia J, Jenkins R, Singleton N, White B. Prevalence of alcohol consumption and hazardous drinking, tobacco and drug use in urban Tanzania, and their associated risk factors. Int J Environ Res Public Health. 2009; 6: 1991–2006.
- Kamat VR. Dying under the bird%26apos%3Bs shadow: narrative representations of Degedege and child survival among the Zaramo of Tanzania. Med Anthropol Q. 2008; 22: 67–93.
- Foster D, Vilendrer S. Two treatments, one disease: childhood malaria management in Tanga, Tanzania. Malar J. 2009; 8: 240.
- Comoro C, Nsimba S, Warsame M, Tomson G. Local understanding, perceptions and reported practices of mothers/guardians and health workers on childhood malaria in a Tanzanian district%26mdash%3Bimplications for malaria control. Acta Tropica. 2003; 87: 305–13.
- Simpson K. Diabetes in Tanzania: insulin supply and availability. J R Coll Physicians Edinb. 2003; 33: 181–201.
- Ferry GA, Dickson SR, Mbaruku G, Freedman LP, Kruk ME. Equity of inpatient health care in rural Tanzania: a population-and facility-based survey. Int J Equity Health. 2012; 11: 7.
- Simba DO, Kakoko DC, Warsame M, Premji Z, Gomes MF, Tomson G. Research understanding caretakers%26rsquo%3B dilemma in deciding whether or not to adhere with referral advice after pre-referral treatment with rectal artesunate. Malaria Journal. 2010; 9: 1–9.
- Mangesho P, Shayo E, Makunde W, Keto G, Mandara C, Kamugisha M, etal. Community knowledge, attitudes and practices towards tuberculosis and its treatment in Mpwapwa District, central Tanzania. Tanzan J Health Res. 2007; 9: 38–43.
- Haram L. Assessment of health-care seeking behaviour: the case of co-infection of TB and HIV/AIDS in Temeke, Tanzania. 2008; Trondheim, Norway: Nowegiean University of Science and Technology (NTNU).
- Obrist B, Iteba N, Lengeler C, Makemba A, Mshana C, Nathan R, etal. Access to health care in contexts of livelihood insecurity: a framework for analysis and action. PLoS Med. 2007; 4: e308.
- Kolling M, Winkley K, von Deden M. Research %26ldquo%3BFor someone who%26apos%3Bs rich, it%26apos%3Bs not a problem.%26rdquo%3B Insights from Tanzania on diabetes health-seeking and medical pluralism among Dar es Salaam%26apos%3Bs urban poor. Globalization and Health. 2010; 6: 8.
- Dillip A, Hetzel M, Gosoniu D, Kessy F, Lengeler C, Mayumana I, etal. Socio-cultural factors explaining timely and appropriate use of health facilities for degedege in south-eastern Tanzania. Malar J. 2009; 8: 144.
- Roura M, Busza J, Wringe A, Mbata D, Urassa M, Zaba B. Barriers to sustaining antiretroviral treatment in Kisesa, Tanzania: a follow-up study to understand attrition from the antiretroviral program. AIDS Patient Care STDs. 2009; 23: 203–10.
- Kabanywanyi AM, Lengeler C, Kasim P, King%26apos%3Beng%26apos%3Bena S, Schlienger R, Mulure N, etal. Adherence to and acceptability of artemether-lumefantrine as first-line anti-malarial treatment: evidence from a rural community in Tanzania. Malar J. 2010; 9: 48.
- Watt MH, Maman S, Earp JA, Eng E, Setel PW, Golin CE, etal. %26ldquo%3BIt%26apos%3Bs all the time in my mind%26rdquo%3B: facilitators of adherence to antiretroviral therapy in a Tanzanian setting. Soc Sci Med. 2009; 68: 1793–800.
- Mendis S, Fuster V. National policies and strategies for noncommunicable diseases. Nat Rev Cardiol. 2009; 6: 723–7.
- Mfinanga SG, Kivuyo SL, Ezekiel L, Ngadaya E, Mghamba J, Ramaiya K. Public health concern along side with global initiative on the priority action for %26ldquo%3Bsilent uprising epidemic%26rdquo%3B on non-communicable diseases in Tanzania. Tanzan J Health Res. 2012; 13: 1–6.
- National Multi-sectoral HIV Prevention Strategy-NACP. Available from: http://www.nacp.go.tz/documents/PreventionStrategy.pdf [cited 24 January 2014].
- Armstrong T, Bull F. Development of the world health organization global physical activity questionnaire (GPAQ). J Public Health. 2006; 14: 66–70.
- Ramaiya K. Personal view: Tanzania and diabetes%26mdash%3Ba model for developing countries?. Br Med J. 2005; 330: 679.
- Mbanya JCN, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010; 375: 2254–66.
- Lekoubou A, Awah P, Fezeu L, Sobngwi E, Kengne AP. Hypertension, diabetes mellitus and task shifting in their management in sub-Saharan Africa. Int J Environ Res Public Health. 2010; 7: 353–63.
- WHO: World Health Organization. Integrated health services %26ndash%3B what and why. 2008; Geneva: WHO. Technical Brief.
- Janssens B, Van Damme W, Raleigh B, Gupta J, Khem S, Soy Ty K, etal. Offering integrated care for HIV/AIDS, diabetes and hypertension within chronic disease clinics in Cambodia. Bull World Health Organ. 2007; 85: 880–5.
- Epping-Jordan J, Pruitt S, Bengoa R, Wagner E. Improving the quality of health care for chronic conditions. Qual Saf Health Care. 2004; 13: 299–305.
- Nissinen A, Berrios X, Puska P. Community-based noncommunicable disease interventions: lessons from developed countries for developing ones. Bull World Health Organ. 2001; 79: 963–70.
- Dawad S, Jobson G. Community-based rehabilitation programme as a model for task-shifting. Disabil Rehabil. 2011; 33: 1997–2005.
- Hatcher A, de Wet J, Bonell CP, Strange V, Phetla G, Proynk PM, etal. Promoting critical consciousness and social mobilization in HIV/AIDS programmes: lessons and curricular tools from a South African intervention. Health Educ Res. 2011; 26: 542–55.
- Krishnan A, Ekowati R, Baridalyne N, Kusumawardani N, Kapoor S, Leowski J. Evaluation of community-based interventions for non-communicable diseases: experiences from India and Indonesia. Health Promot Int. 2011; 26: 276–89.
- Jagoe K, Edwards R, Mugusi F, Whiting D, Unwin N. Tobacco smoking in Tanzania, East Africa: population based smoking prevalence using expired alveolar carbon monoxide as a validation tool. Tob Control. 2002; 11: 210–14.
- Gonzalez JS, Penedo FJ, Antoni MH, Dur%26aacute%3Bn RE, McPherson-Baker S, Ironson G, etal. Social support, positive states of mind, and HIV treatment adherence in men and women living with HIV/AIDS. Health Psychol. 2004; 23: 413.
- Munro SA, Lewin SA, Smith HJ, Engel ME, Fretheim A, Volmink J. Patient adherence to tuberculosis treatment: a systematic review of qualitative research. PLoS Med. 2007; 4: e238.
- Murphy CM. Writing an effective review article. J Med Toxicol. 2012; 8: 89–90.
- Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006; 5: 101–17.