Abstract
Background
Several studies have shown that Alaska Native people have higher smoking prevalence than non-Natives. However, no population-based studies have explored whether smoking-related knowledge, attitudes, and behaviours also differ among Alaska Native people and non-Natives.
Objective
We compared current smoking prevalence and smoking-related knowledge, attitudes, and behaviour of Alaska Native adults living in the state of Alaska with non-Natives.
Methods
We used Alaska Behavioral Risk Factor Surveillance System data for 1996 to 2010 to compare smoking prevalence, consumption, and cessation- and second-hand smoke-related knowledge, attitudes, and behaviours among self-identified Alaska Native people and non-Natives.
Results
Current smoking prevalence was 41% (95% CI: 37.9%–44.4%) among Alaska Native people compared with 17.1% (95% CI: 15.9%–18.4%) among non-Natives. Among current every day smokers, Alaska Natives were much more likely to smoke less than 10 cigarettes per day (OR=5.0, 95% CI: 2.6–9.6) than non-Natives. Compared with non-Native smokers, Alaska Native smokers were as likely to have made a past year quit attempt (OR=1.4, 95% CI: 0.9–2.1), but the attempt was less likely to be successful (OR=0.5, 95% CI: 0.2–0.9). Among current smokers, Alaska Natives were more likely to believe second-hand smoke (SHS) was very harmful (OR=4.5, 95% CI: 2.8–7.2), to believe that smoking should not be allowed in indoor work areas (OR=1.9, 95% CI: 1.1–3.1) or in restaurants (OR=4.2, 95% CI: 2.5–6.9), to have a home smoking ban (OR=2.5, 95% CI: 1.6–3.9), and to have no home exposure to SHS in the past 30 days (OR=2.3, 95% CI: 1.5–3.6) than non-Natives.
Conclusion
Although a disparity in current smoking exists, Alaska Native people have smoking-related knowledge, attitudes, and behaviours that are encouraging for reducing the burden of smoking in this population. Programs should support efforts to promote cessation, prevent relapse, and establish smoke-free environments.
Cigarette smoking is common among Alaska Native people: 41% of Alaska Native adults living in the state of Alaska are current smokers (Citation1), compared with 19% in the US adult population (Citation2). Studies of the disparity in adult smoking among racial and ethnic groups living in the United States typically combine Alaska Native and American Indian populations together (Citation3, Citation4). To our knowledge, only one published study has examined population-based data on the prevalence of tobacco use among all Alaska Native adults living in the state of Alaska (Citation5). Other studies of tobacco use among Alaska Native people have been focused on a subset of the Alaska Native population, such as pregnant women (Citation6, Citation7), youth (Citation8), those with children in the home (Citation9), or those in specific areas of the state (Citation10–Citation12).
The primary purpose of this study is to provide current population-based estimates of smoking prevalence among Alaska Native people living in Alaska and augment these data with a broad array of new information on smoking-related knowledge, attitudes, and behaviours. We are unaware of any population-based studies that have assessed this type of information in the state-wide Alaska Native population. It is important to assess knowledge, attitudes, and behaviours surrounding smoking in order to develop effective, culturally tailored interventions that are acceptable to Alaska Native people.
Method
Population
Alaska Native people refers to the original inhabitants of the land that is now the state of Alaska. There are more than 120,000 Alaska Native people who currently live in Alaska, and they comprise about 17% of the state's 720,000 residents.
Data source
We report on data from the Alaska Behavioural Risk Factor Surveillance System (BRFSS) from 1996 to 2010. The Alaska BRFSS is part of the national BRFSS, and it is a population-based, random-digit-dialed, cross-sectional survey stratified on geographic region. Eligible participants are non-institutionalized (i.e. nursing homes, dormitories), aged 18 years or over, who speak English (Citation13). In 1996–2010, the Council of American Survey Research Organizations (CASRO) response rate ranged from 47.7% (year 2000) to 67.5% (year 2005).
Alaska presently conducts 2 BRFSS surveys: the standard BRFSS and a supplemental Alaska BRFSS, which contains many tobacco questions adapted from the Center for Disease Control and Prevention's (CDC's) Adult Tobacco Survey. Both surveys are conducted throughout the year, and separate samples are drawn using the same methodology. At present, approximately 210 Alaska adults are interviewed each month for the standard BRFSS to reach an annual sample size of 2,500; the same number of adults are interviewed for the supplemental BRFSS, for a total of roughly 5,000 survey respondents per year for both surveys. The sample size varied each year, ranging from a low of 1,536 in 1996 to a high of 5,755 in 2005. When possible, we used a data set combining the standard and supplemental BRFSS surveys to provide the estimates contained in this report. In cases where questions appeared on only one of the surveys, we used that particular data set.
Study measures
Demographic measures
We asked all respondents to identify their race, ethnicity, age, gender, highest level of formal education achieved, and whether or not children were present in the home. Regarding race and ethnicity, the survey included a question about whether participants were Hispanic or Latino and a separate question about race. For participants who reported more than one race, we also asked about primary race, “Which one of these groups would you say best represents your race?” For this study, the Alaska Native category includes respondents who reported “Alaska Native/American Indian” as their primary or only race group, and the non-Native category includes all other respondents.
Smoking status and quit ratio
We asked all respondents whether they had smoked 100 cigarettes in their lifetimes. For those that responded “yes” (ever smokers) we then asked if they now smoke “every day, some days, or not at all.” Those who responded “every day” or “some days” are considered current smokers. Former smokers are those who had smoked 100 cigarettes, but answered that they now smoke “not at all.” This is a standard smoking measure used in several population-based surveys (Citation14, Citation15). We also assessed the quit ratio, defined as the proportion of former smokers among ever smokers.
Consumption
We asked current smokers “On days when you smoked during the past 30 days, about how many cigarettes did you smoke a day?” We then examined current some day and every day smokers who report smoking less than 10 cigarettes per day.
Stage of change
We defined the proportion of current smokers who want to quit smoking by those who answered “yes” to the question, “Would you like to quit smoking?” For those who responded “yes” we then asked if they were seriously considering quitting smoking in the next 6 months. If they responded “yes,” we then asked if they were considering quitting in the next 30 days. Those considering quitting in the next 30 days were considered in the preparation stage of the Stage of Change model (Citation16).
Advised to quit
We defined the proportion of smokers advised to quit by a health professional by those who answered “yes” to the question, “In the past 12 months, has a doctor, nurse, or other health professional advised you to quit smoking?” We asked this question only of those respondents who had seen a health professional for care in the past 12 months.
Awareness of tobacco quit line
We asked all respondents if they were aware of the Alaska Tobacco Quit Line, a free telephone service that can help people quit smoking. We assessed the proportion of current smokers aware of the service.
Past year quit behaviour
We combined former smokers who quit 1 year ago or less with all current smokers to examine patterns in past year quit attempts and success. We placed respondents into 3 categories: persons with no quit attempt in the past year, persons with an unsuccessful quit attempt in the past year, and persons with a successful quit attempt in the past year. To examine quit attempts (whether eventually successful or not), we compared the first category to the latter 2 categories combined. To examine quit success, we compared the latter 2 categories to each other.
Knowledge of the danger of second-hand smoke (SHS)
We asked all respondents how harmful they thought SHS is to one's health. We dichotomized this measure into very harmful versus all else.
Attitudes about clean indoor air policies
We asked all respondents “In indoor work areas do you think that smoking should be allowed in all areas, in some areas, or not allowed at all?” We dichotomized this measure into not allowed at all versus all else. We also asked the same question specifically about restaurants. This variable was also dichotomized into not allowed at all versus all else.
Smoking in the home
We asked all respondents, “Which statement best describes the rules about smoking inside your home: smoking is not allowed anywhere inside your home, smoking is allowed in some places or at some times, smoking is allowed anywhere inside your home?” We dichotomized this measure into smoking is not allowed anywhere inside home versus all else.
Exposure to SHS
We asked all respondents if anyone had smoked inside their home in the previous 30 days. We dichotomized this measure into zero days versus one or more days.
Smoking in the workplace
We asked respondents who reported working indoors most of the time about the official smoking policy at their workplace. We dichotomized this measure into smoking is not allowed in any indoor work area versus all else.
Analyses
We used data from 1996 to 2010 to examine trends in current smoking prevalence among Alaska Native people and non-Natives. For all other comparisons, we used combined data from 2008 to 2010 to provide the most current estimates of smoking-related knowledge, attitudes, and behaviour.
For all analyses, we used the 0.05 level of significance and procedures in Stata® that took into account complex sampling design. Data were weighted to adjust for differential sampling rates within each telephone bank and for the number of telephones and adults in the household, and to ensure that the age, gender, and geographic distribution of respondents matched that for all Alaskans based on the Claritas population estimates for a given year (Citation17). We tested for trends during 1996–2010 in current smoking prevalence with logistic regression. Using data from 2008 to 2010, a Pearson chi-square test with Rao and Scott second-order correction was used to determine whether age, gender, education, and presence of children in the home varied by race (Alaska Native people versus non-Native). Also using 2008–2010 data, we tested for associations between race and smoking-related measures using multiple logistic regression models adjusted for age, gender, and education.
Results
Demographics
Compared with non-Natives, Alaska Native people tended to be younger (p<0.001), had less formal education (p<0.001), and were more likely to have children living in the home (p<0.001) ().
Table I Characteristics of Alaska Native and non-Native adults, BRFSS 2008–2010 (N =12,948)
Smoking-related indicators
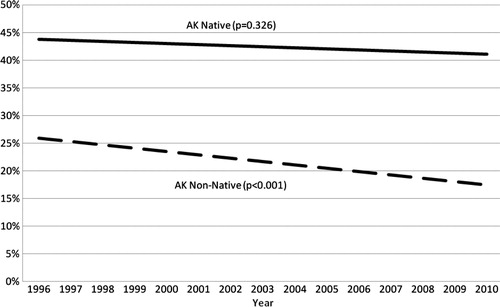
The current smoking prevalence among Alaska Native people was more than twice that of non-Natives (). Although smoking prevalence has declined among non-Natives (p<0.001), no significant decline has been observed among Alaska Native people (p=0.33) ().
Table II Prevalence of smoking and related indicators among Alaska Native and non-Native adults, BRFSS 2008–2010
The odds of having ever smoked were significantly higher for Alaska Native people than non-Natives (). Among ever smokers, the odds of being a former smoker (quit ratio) were significantly lower for Alaska Native people. Alaska Native current smokers were as likely to be every day smokers as non-Native current smokers. However, among every day smokers, Alaska Natives had 5 times the odds of smoking less than 10 cigarettes per day. Among some day smokers, Alaska Native and non-Native smokers had the same odds of smoking less than 10 cigarettes per day.
Cessation-related indicators
Alaska Native smokers had similar odds of wanting to quit smoking and planning to quit smoking in the next 30 days as non-Native smokers (). Alaska Native smokers had decreased odds of being advised by a health professional to quit smoking, although the estimate was not statistically significant (p=0.08). Alaska Native smokers were as likely as non-Native smokers to be aware of the Alaska Tobacco Quit Line. Compared with non-Natives, Alaska Native smokers were as likely to make a quit attempt but were significantly less likely to quit successfully.
Table III Cessation-related indicators among Alaska Native and non-Native adults, BRFSS 2008–2010
SHS-related indicators
Among smokers and non-smokers, Alaska Native people were significantly more likely to believe that SHS is very harmful (). Alaska Native smokers and non-smokers were also significantly more likely to agree that smoking should not be allowed at all in indoor work areas and in restaurants.
Table IV Second-hand smoke-related indicators among Alaska Native and non-Native adults, BRFSS 2008–2010
Alaska Native smokers and non-smokers were significantly more likely to have both a home smoking ban and no home exposure to SHS in the past 30 days as compared to non-Native smokers and non-smokers (). In the workplace, Alaska Native smokers were less likely to have a smoking ban, although this association did not reach statistical significance (p=0.12). Among non-smokers, there was no significant difference between Alaska Natives and non-Natives in the likelihood of having a workplace smoking ban.
Discussion
Although the disparity in smoking among Alaska Native people continues to persist—twice as many Alaska Native people smoke cigarettes compared with non-Natives—our results suggest that Alaska Native people have knowledge, attitudes, and behaviours that could support reductions in the burden of smoking. For example, Alaska Native every day smokers consume fewer cigarettes per day than non-Native smokers, potentially indicating lower addiction levels (Citation18). In addition, they are equally likely to want to quit, to be ready to quit, and to actually attempt to quit as non-Native smokers. However, Alaska Native smokers had half the odds of making a successful quit attempt compared to non-Natives. These findings contradict other evidence that lower addiction levels are associated with lower risks of relapse after a quit attempt (Citation19). Finding ways to address relapse triggers such as stress and depression, which are high in Alaska Native people (Citation20, Citation21), could be helpful.
In addition, awareness of the Alaska Tobacco Quit Line was high among Alaska Native smokers. In a separate study, Alaska Native users of the Quit Line had high quit rates (22%) and nearly all (90%) reported satisfaction with the service, but the service was underutilized by Alaska Native smokers (Citation22). Further outreach could be done to increase use of the Tobacco Quit Line or to explore alternative cessation interventions in the context of a public health approach.
Taken together, these findings provide important information about how to tailor cessation and relapse prevention efforts in this population. We found it encouraging that a much larger proportion of Alaska Native smokers had knowledge regarding the harms of SHS and very favourable attitudes regarding smoke-free environments in their communities compared with non-Native smokers. Further, Alaska Native smokers were more likely to have home smoking bans. This suggests that public health messages regarding the harms of SHS are reaching the Alaska Native population, and that social norms regarding tobacco may be changing in this population. However, we observed that Alaska Native smokers might be less likely to work in smoke-free environments. Because smoke-free environments support cessation (Citation23, Citation24), this is an area that should be specifically investigated.
Limitations
This study has several limitations. First, the BRFSS excludes individuals who live in homes without landline telephones, those who live in institutions, and those who do not speak English. As noted in a recent study of Alaska Native people, 8% of Alaska Native respondents spoke only native languages (Citation25). These Native people would not be captured in the Alaska BRFSS, which is given only in English, and their smoking related knowledge, attitudes, and behaviour may be different than those of Alaska Native people who speak English. Second, Alaska Native people might be reluctant to report behaviours and attitudes that others might not find acceptable (particularly over the telephone to a stranger). For example, in another study utilization rates of the Alaska Tobacco Quit Line were lower among Alaska Native smokers compared with non-Native smokers, suggesting that Alaska Natives may be uncomfortable revealing personal information over the telephone (Citation22). Future researchers may want to investigate this potential limitation by comparing results obtained through different data collection strategies.
Conclusions
Despite the large disparity in current smoking prevalence, Alaska Native people living in Alaska have smoking-related knowledge, attitudes, and behaviours that suggest they want to quit and strongly support smoke-free environments. Public health programs should continue to monitor and explore patterns in quit behaviours including relapse in this population. Additionally, in order to achieve smoking prevalence reductions, efforts should explore culturally appropriate ways to promote cessation and to prevent relapse among Alaska Native smokers, and to build upon the strong preference among Alaska Native people for smoke-free environments.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
This work was funded by the Alaska Tobacco Prevention and Control Program, Alaska Department of Health and Social Services. The program is supported through excise tax revenues and Master Settlement Agreement funds.
References
- Alaska Department of Health and Social Services. Alaska tobacco facts April 2012 update. [cited 2012 Nov 16]. Available from: http://www.dhss.alaska.gov/dph/chronic/documents/tobacco/pdf/2012_alaska_tobacco_facts.pdf.
- Centers for Disease Control and Prevention. Current cigarette smoking among adults—United States, 2011. Morbidity Mortality Weekly Rep. 2012; 61: 889–94.
- Caraballo RS, Yee SL, Gfoerer J, Mirza SA. Adult tobacco use among racial and ethnic groups living in the United States, 2002–2005. Prev Chronic Dis. 2008; 5: 1–9.
- Fagan P, Moolchan ER, Lawrence D, Fernander A, Ponder PK. Identifying health disparities across the tobacco continuum. Addiction. 2007; 102: 5–29.
- Kaplan SD, Lanier AP, Merritt RK, Siegel PZ. Prevalence of tobacco use among Alaska Natives: a review. Prev Med. 1997; 26: 460–5.
- Kim SY, England L, Dietz PM, Morrow B, Perham-Hester KA. Prenatal cigarette smoking and smokeless tobacco use among Alaska Native and white women in Alaska, 1996–2003. Matern Child Health J. 2009; 13: 652–9.
- Renner CC, Patten CA, Day GE, Enoch CC, Schroeder DR, Offord KP, etal. Tobacco use during pregnancy among Alaska Natives in western Alaska. Alaska Med. 2005; 47: 12–16.
- Angstman S, Patten CA, Renner CC, Simon A, Thomas JL, Hurt RD, etal. Tobacco and other substance use among Alaska Native youth in western Alaska. Am J Health Behav. 2007; 31: 249–60.
- Dent CW, Maher JE, Pizacani BA, Dowler DW, Rohde K, Peterson E. Second-hand smoke exposure in Alaskan households with children. Rural Remote Health. 2010; 10: 1564.
- Renner CC, Patten CA, Enoch C, Petraitis J, Offord KP, Angstman S, etal. Focus groups of Y-K Delta Alaska Natives: attitudes toward tobacco use and tobacco dependence interventions. Prev Med. 2004; 38: 421–31.
- Renner CC, Enoch E, Patten CA, Ebbert JO, Hurt RD, Moyer TP, etal. Iq'mik: a form of smokeless tobacco used among Alaska Natives. Am J Health Behav. 2005; 29: 588–94.
- Renner CC, Lanier AP, Lindgren B, Jensen J, Patten CA, Parascandola M, etal. Tobacco use among southwestern Alaska Native people. Nicotine Tob Res. 2013; 15: 401–6.
- Alaska Behavioral Risk Factor Surveillance Survey. [cited 2012 Nov 14]. Available from: http://www.dhss.alaska.gov/dph/chronic/pages/brfss/method.aspx.
- Centers for Disease Control and Prevention. National health interview survey. [cited 2013 Feb 26]. Available from: http://www.cdc.gov/nchs/nhis.htm.
- National Cancer Institute. Tobacco use supplement of the current population survey. [cited 2013 Feb 26]. Available from: http://riskfactor.cancer.gov/studies/tus-cps/.
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997; 12: 38–48.
- Nielsen Claritas Site Reports. [cited 2012 Nov 13]. Available from: http://www.claritas.com/sitereports/default.jsp.
- Chabrol H, Niezborala M, Chastan E, DeLeon J. Comparison of the heavy smoking index and of the Fagerstrom test for nicotine dependence in a sample of 749 cigarette smokers. Addict Behav. 2005; 30: 1474–7.
- Sweitzer MM, Denlinger RL, Donny EC. Dependence and withdrawal-induced craving predict abstinence in an incentive-based model of smoking relapse. Nicotine Tob Res. 2013; 15: 36–43.
- McKee SA, Sinha R, Weinberger AH, Sofuoglu M, Harrison EL, Lavery M, etal. Stress decreases the ability to resist smoking and potentiates smoking intensity and reward. J Psychopharmacol. 2011; 25: 490–502.
- Dillard DA, Smith JJ, Ferucci ED, Lanier AP. Depression prevalence and associated factors among Alaska Native people: the Alaska Education and Research Toward Health (EARTH) study. J Affect Disord. 2012; 136: 1088–97.
- Boles M, Rohde K, He H, Maher JE, Stark MJ, Fenaughty A, etal. Effectiveness of a tobacco quitline in an indigenous population: a comparison between Alaska Native people and other first-time quitline callers who set a quit date. Int J Circumpolar Health. 2009; 68: 170–81.
- U.S. Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General . 2006; Washington, DC: U.S. Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office of Smoking and Health.
- National Cancer Institute. Population based smoking cessation: proceedings of a conference on what works to influence cessation in the general population. Smoking and Tobacco Control Monograph No. 12 . 2000
- Schumacher MC, Slattery ML, Lanier AP, Ma KN, Edwards S, Ferucci ED, etal. Prevalence and predictors of cancer screening among American Indian and Alaska Native people: the EARTH study. Cancer Causes Control. 2008; 19: 725–37.