Abstract
Background
Changing Directions, Changing Lives, the Mental Health Strategy for Canada, prioritizes the development of coordinated continuums of care in mental health that will bridge the gap in services for Inuit populations.
Objective
In order to target ways of improving the services provided in these contexts to individuals in Nunavik with depression or anxiety disorders, this research examines delays and disruptions in the continuum of care and clinical, individual and organizational characteristics possibly associated with their occurrences.
Design
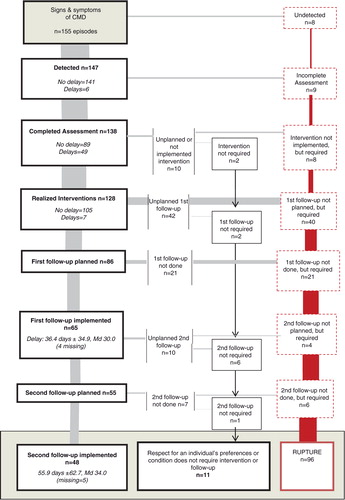
A total of 155 episodes of care involving a common mental disorder (CMD), incident or recurring, were documented using the clinical records of 79 frontline health and social services (FHSSs) users, aged 14 years and older, living in a community in Nunavik. Each episode of care was divided into 7 stages: (a) detection; (b) assessment; (c) intervention; (d) planning the first follow-up visit; (e) implementation of the first follow-up visit; (f) planning a second follow-up visit; (g) implementation of the second follow-up visit. Sequential analysis of these stages established delays for each one and helped identify when breaks occurred in the continuum of care. Logistic and linear regression analysis determined whether clinical, individual or organizational characteristics influenced the breaks and delays.
Results
More than half (62%) the episodes of care were interrupted before the second follow-up. These breaks mostly occurred when planning and completing the first follow-up visit. Episodes of care were more likely to end early when they involved anxiety disorders or symptoms, limited FHSS teams and individuals over 21 years of age. The median delay for the first follow-up visit (30 days) exceeded guideline recommendations significantly (1–2 weeks).
Conclusion
Clinical primary care approaches for CMDs in Nunavik are currently more reactive than preventive. This suggests that recovery services for those affected are suboptimal.
Over the past 20 years, mental health problems and psychological distress have increased among the populations of Inuit Nunangat (homeland of the Canadian Inuit) (Citation1–Citation3). Given the potential impact on those affected, their loved ones and individuals living in northern communities (Citation4, Citation5), it is important to act on multiple determinants such as access to quality local healthcare (Citation1).
Healthcare services in remote regions face several geographical, organizational and cultural constraints that can bring about inconsistencies in mental health clinical approaches (Citation1, Citation2) (Citation6–Citation8). Therefore, to bridge critical gaps in the provision of services for Canada's Inuit, national mental health action plans make the development of coordinated continuums of care a priority (Citation1, Citation6). However, implementation of adapted and sustainable solutions must be determined by contextualized information.
This article presents the results of research that documented the continuum of care for individuals with common mental disorders (CMDs) living in northern communities. The disorders referred to are depression and anxiety. Because CMDs are so often underdiagnosed, few reliable data are available on the epidemiology of these disorders in Inuit Nunangat (Citation4, Citation5) (Citation9, Citation10). Nevertheless, based on measured levels of psychological distress and the presence of numerous mental health risk factors, it is generally agreed that there is high prevalence (Citation2, Citation3) (Citation9, Citation10).
Current clinical guidelines for CMDs
CMDs are often associated with increased suicide risk and significant functional impairment at professional, academic, social and family levels (Citation11). Due to the high risk of relapse, these disorders are increasingly regarded as chronic conditions. Current general guidelines encourage frontline health and social services (FHSSs) to manage most affected individuals, while reserving specialized services for more complex cases (Citation12, Citation13). For FHSSs to contribute effectively to an individual's recovery on the psychosocial, emotional and community level, the least that is expected is (Citation13–Citation15):
improved accessibility
rapid detection and adequate assessment of CMDs
early intervention to limit functional impairment, that takes into account the individual's condition, treatment and medical history, risk factors and preference
long-term follow-ups to ensure continuous monitoring of the individual's status, so that treatment can be adjusted and also to encourage adherence to the treatment plan.
FHSSs in Inuit Nunangat
FHSSs are generally described as the first level of universally accessible services that promote health, prevent diseases and provide diagnostic, curative, rehabilitative, support and palliative services (Citation16). Their design depends on where they are developed (Citation17). In Inuit Nunangat, as in other remote regions, FHSS teams are multidisciplinary and healthcare providers generally play a major role in meeting the population's essential healthcare needs. General practitioners support nurses and social workers locally or remotely. In communities with no permanent doctors, medical visits can be organized and access to specialized mental health resources is usually dependent upon service agreements with health facilities in urban areas in the south.
Objectives
This research aims to document the continuum of care for individuals with a CMD who consult FHSSs in Nunavik, one of Inuit Nunangat's 4 regions. The authors have addressed the continuum of care in terms of continuity of contact, that is, the maintenance of care over time to create a continuum of services that satisfy the individual's needs (Citation18). Our objectives were to identify: (a) delays and disruptions in the continuum of care; and (b) clinical, individual and organizational factors possibly associated with such occurrences.
Study setting
Nunavik is a 505,000 km2 region located north of the 55th parallel in Quebec province. In 2006, 91% of the region's 10,784 inhabitants self-identified as Inuit (Citation19). The population is spread among 14 communities on the shores of Hudson Bay and Ungava Bay. These communities are fly-in villages. They have no road connection to each other or to Quebec's road network. The main method of transportation is by plane and this is very costly and time-consuming.
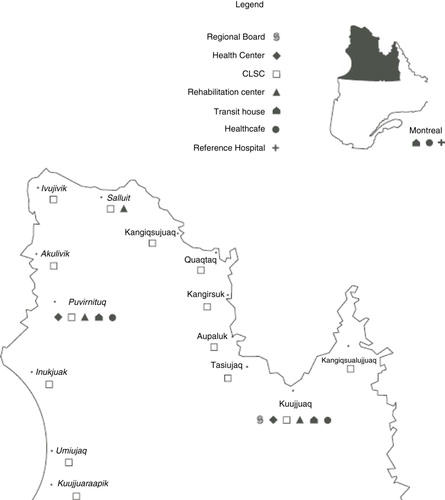
Nunavik's health infrastructure has been part of Quebec's healthcare system since 1975 (Citation20). The Nunavik Regional Board of Health and Social Services organizes health and social services programs and coordinates budget allocations for 2 sub-regional healthcare centres that offer general hospital services to the populations of Ungava Bay and Hudson Bay. Primary nursing care and social services are available at the local health centre in each community, referred to locally as the nursing station. Local centres are linked administratively to one of the larger healthcare centres, either Tulattavik Health Centre (Ungava Bay) or Inuulitsivik Health Centre (Hudson Bay) (). For mental health, service agreements with specialized facilities in Montreal enable FHSS teams to organize regular visits by psychiatrists and child and adolescent psychiatrists in the region; provide remote support to FHSS teams; and guarantee access to hospital beds. During this study, the region had only one adult psychologist working at the Tulattavik (Ungava Bay) healthcare centre. Since 1999, Nunavik has implemented infrastructure dedicated in whole or in part to individuals with mental health problems (crisis centre, reintegration centre for individuals with severe mental disorders, homes for troubled youth, supervised apartments and drug treatment centres).
Methods
Study design
This study is based on a descriptive correlational design where the continuum of care is studied for time-limited episodes. These episodes refer only to the occurrence of a CMD or relapse. Each episode begins at the first sign and symptom of a CMD and ends after the second follow-up visit.
Population and sample
The study population comprised FHSS users in Nunavik, aged 14 years and older who experienced at least one CMD-associated episode of care (occurrence or relapse) during an observation period.
Data source
Researchers documented episodes of care extracted from 79 clinical records of FHSS users in Nunavik, who were aged 14 years or older on 1 January 2007 and who had depression or an anxiety disorder. Data were collected in 2009 in 10 Nunavik communities as part of a research program on the quality of mental healthcare (Citation21). The data were recorded in an Access database and described all the consultations of individuals presenting with suspected or confirmed CMDs over a 2-year observation period. This period was established by using the last mental health consultation in 2007 as point of reference and then adding the previous and the following 12 months. The presence of a CMD was confirmed after considering the diagnoses documented during the observation period or, in their absence, by establishing research diagnoses from signs and symptoms presented by the individual during this period. The data collection process, developed tools and data preparation were validated using a rigorous iterative approach. This data collection process is detailed in another article (Citation22).
Examining episodes of care
A total of 155 episodes of care were reconstructed. Each episode of care was divided into 7 stages: (a) detection; (b) assessment; (c) intervention; (d) planning the first follow-up visit; (e) implementation of the first follow-up visit; (f) planning a second follow-up visit; (g) implementation of the second follow-up visit. The delay to carry out each stage and identify interruptions in the continuum of care was based on the sequential examination of the stages. Table shows the conditions for success, the delays and the interruptions for each stage.
Table I. Conditions for success, delays and interruptions at each stage of an episode of care
All interruptions that occurred during detection and assessment were deemed breaks in the continuum of care. For stages related to interventions and the 2 follow-up visits, the interruption was not viewed as a break if the individual did not want to be treated or monitored, or if their condition did not require it. According to CMD guidelines (Citation13, Citation15), the need to treat or monitor an individual is associated with the presence of 1 of 3 conditions:
a moderate to severe CMD diagnosis
symptoms of CMD in patients with a history of CMD, an alcohol or drug problem or a chronic or serious physical illness
symptoms of CMD in patients with significant functional impairment.
When this information was not available, the Global Assessment of Functioning scale (GAF) was used to establish a functioning score that took into account medical history plus the type, duration and intensity of the reported symptoms (Citation11). A score of ≤61 meant that function was deemed altered. These scores were established as necessary following interventions and implementation of the first follow-up.
Influence of clinical, organizational and individual characteristics
Dependent variables
Dependent variables correspond to (a) breaks occurring at each stage in the continuum of care and overall and (b) delays assessed for each stage. Success, interruptions, detection delays, assessment and interventions are dichotomous categorical variables. Delays in conducting first and second follow-up visits are continuous variables calculated in number of days.
Independent variables
Independent variables correspond to clinical characteristics of episodes of care and to individual and organizational characteristics that can influence the use and provision of services for individuals presenting with CMDs (Citation13, Citation15). These variables are dichotomous.
Episodes of care were first categorized as depression and anxiety based on diagnosis. Where no diagnosis was available, prevalence of signs and symptoms was used. Episodes with both anxiety and depressive components were classed as depression since guidelines recommend treating depression first (Citation13). Episodes were then categorized as incident or relapse, depending on CMD history. The history could have been documented previously or during the observation period. Finally, diagnoses made during episodes of care were categorized as precise or imprecise. A precise diagnosis was (a) made by a person qualified to assess mental disorders (in Quebec province, a physician or psychologist) and (b) not accompanied by other potential diagnoses. Diagnostic accuracy was determined from the assessment stage.
Individuals’ characteristics included age, sex, ethnicity, presence of chronic or severe physical illness and problems associated with alcohol or substance abuse (Citation13). There were 2 age groups (14–20 years and 21 and over) to ascertain whether there were differences between youth and adult services. Ethnicity was based on whether or not the individual was Inuk, which was determined by surname and medical history (anamnesis). Physical illnesses had to have been present during the observation period and related to certain conditions: diabetes, cardiac or chronic respiratory problems, rheumatoid arthritis, chronic pain, cancer, severe sensory limitations, epilepsy, thyroid imbalances and other conditions causing significant distress. The presence of at least one note during the observation period that reported regular use or abuse of alcohol or illicit drugs established alcohol or drug-related problems (Citation23).
Organizational characteristics refer to the Tulattavik Health Centre (Ungava Bay) and the Inuulitsivik Health Centre (Hudson Bay), as well as the FHSS teams. Teams were classed as limited or expanded according to whether or not a permanent doctor was available on-site.
Statistical analysis
Descriptive statistics were used to highlight delays, interruptions and breaks at each stage in the continuum of care. The impact of the independent variables on breaks and delays was then examined using comparative analysis. First, bivariate analysis was carried out. Analyses involving clinical characteristics of episodes of care used chi-square tests for the categorical dependent variables and t-tests for continuous dependent variables. Logistic and linear regression models were used for individual and organizational characteristics. Since a single individual could have more than 1 episode of care (Citation24), the models were adjusted using a generalized estimating equation approach (GEE) to take into account data correlations (Citation25). To ensure the validity of multivariate logistic regression models, a rule recommending a minimum of 10 occurrences per independent variable was applied (Citation26). In addition, only variables in the bivariate analysis with p-values less than ≤0.25 were retained in the multivariate regression models. Analyses were performed using SPSS 22 software and results are considered significant at ≤0.05.
Ethical approvals
This research received administrative approval from the participating healthcare centres as well as ethical certification from the Agence de la santé et des services sociaux in Montreal and Université Laval's research ethics committee.
Results
Sample characteristics
Table presents the individual and organizational characteristics of the sample (79 individuals). For the episodes, the number of individuals per file varies from 1 to 9 (x=2.1, SD=1.6; md= 2.0) and their characteristics are shown in Table .
Table II. Individual and organizational characteristics of sample (n=79)
Table III. Clinical characteristics of care episodes (n = 155)
Women make up almost two-thirds of the sample. This is consistent with the distribution of CMDs found in the general population (Citation27). More than half the sample population had a serious or chronic physical illness (51%) or alcohol and drug problems (56%). However, this rate is lower than that measured in the population of Nunavik in 2004, where 90% of those 15 and over reported having had at least one alcohol abuse episode and 60% had used illicit drugs during the previous 12 months (Citation23). Nevertheless, this variable was retained for subsequent analysis based on the presumption that recording information on an individual's consumption might be associated with functional impairment for that person. Allocation according to ethnicity, FHSS team and healthcare centre corresponds to what is found in Nunavik's population (Citation19).
The correlation analysis between these variables revealed some significant associations, but only at a mild to moderate intensity (Phi ≤ 0.33). As a result, they were considered sufficiently independent to be retained for the multivariate analysis.
Anxiety episodes outnumber depressive episodes. The majority of anxiety episodes are recurring; that is, there is a history of CMD. Finally, the mental disorder diagnosis was accurate for approximately 40% of episodes. The correlation analysis between the variables Symptom Predominance, Presence of CMD History and Diagnosis Accuracy revealed significant associations of mild to moderate intensity (Phi ≤ 0.26).
Examining episodes of care
presents the success, delays and interruptions for each stage in the episode of care. Of the 155 initial episodes, 48 (31%) were pursued until the second follow-up was conducted and 107 (69%) were interrupted during one of the other previous stages. Of these interruptions, 11 (7%) involved conditions that did not require interventions or follow-ups or were associated with the individual's preferences. The other 96 (62%), showed breaks in the continuum of care that occurred mainly during planning of the first follow-up visit (n = 40; 42%) and at its implementation (n = 21; 22%). For most episodes of care, detection and interventions were carried out without delay. For the assessment stage, more than a third of the episodes required more than 1 visit. The median time for first and second follow-ups was 30.0 days (x=36.4±34.9) and 34.0 (x=55.9 days±62.7), respectively.
Factors associated with breaks in the continuum of care
Bivariate analyses were carried out between breaks and certain clinical, individual and organizational characteristics. The bivariate analyses are shown in Table . Only breaks that occurred in the overall continuum of care as well as stages involving planning and implementation of the first follow-up visit showed a sufficient number of occurrences to perform multivariate analyses. The results of these analyses, expressed as odd ratios (OR), are shown in Tables V , VI and VII . An OR > 1 means an increased risk for a break in the continuum of care while OR < 1 indicates a lower risk.
Table IV. Bivariate analyses for interruptions in continuum of care
Table V. Logistic regressions for interruptions to total continuum of care (n=155)
Table VI. Logistic regressions for interruptions when planning a first follow-up (n=128)
Table VII. Logistic Regressions for interruptions at the implementation of a first follow-up (n=86)
Analyses first performed on clinical characteristics of episodes show that predominantly anxious episodes are 6–7.5 times more likely to result in a premature break in the overall continuum (OR 6.63, p=0.000) than are predominantly depressive episodes, when planning a first follow-up visit (OR=5.89, p=0.000) and at its implementation (OR=7.58, p=0.001). By contrast, Table shows that breaks during the assessment stage would mainly affect depressive episodes (χ2=4.57, p=0.032). For diagnostic accuracy, episodes associated with a precise diagnosis were less likely to experience a break than those categorized as imprecise in the overall continuum (OR=0.15, p=0.000) and in the planning of a first follow-up visit (OR 0.33, p=0.014). It would not influence the implementation of the first follow-up (OR=0.68, p = 0.491), but bivariate analysis indicated that less breaks occurred at the second follow-up for episodes of care showing a precise diagnosis (χ2=5.82, p=0.016). When there was a history of CMD, only one trend was observed for episodes dealing with a CMD relapse that would have shown more breaks in the overall continuum than for episodes considered incidents (OR=2.25, p=0.055).
For individual and organizational characteristics, only age group and team type showed significant differences. Individuals 14–20 years old were more likely to extend across the entire continuum (OR=0.35, p=0.033) compared to the ≥21 age group. For team type, episodes involving the expanded teams had fewer breaks when planning a first follow-up visit when compared to limited’ teams (OR=0.34, p=0.024).
Factors associated with delays in the continuum of care
Table shows delays based on independent variables. No significant differences were found for delays at the detection and intervention stages. For the assessment stage, a significant difference in diagnostic accuracy (Table ) was observed. The assessment of episodes with precise diagnoses was conducted over more than 1 visit whereas imprecise diagnosis took place in 1 visit (OR=3.58, p=0.001). T-tests showed no significant difference when estimating effects of the clinical characteristics of episodes on delays in implementing the first and second follow-up visits. Estimating the effects of individual and organizational characteristics on delays in conducting the first and second follow-up visits using bivariate linear regression models, necessitated the conducting of a log transformation for time to ensure normal sample distribution. The results involving these stages refer to Exp (β)-1, which represents how much longer the delay was when an individual presented the studied factor. These analyses showed that the non-Inuit had a 203% (exp (β)-1=2.03; p=0.002) longer delay for the first follow-up visit than the Inuit, and that individuals aged 14–20 years had a 55% (exp (β)-1 =0.55; p=0.046) longer delay for the second follow-up visit than those aged 21 and over.
Table VIII. Bivariate analysis of delays occurring at each step of the continuum of care
Table IX. Logistic regression analysis of delays occurring at assessment
Discussion
The study's main objective was to document the continuum of care for episodes of care involving individuals with CMD in Nunavik. Most importantly, the results show that a little less than a third of episodes of care get as far as the second follow-up visit. They also indicate that most interruptions in episodes of care involve breaks in the continuum of care. These interruptions generally occur during the planning and implementation of the first follow-up visit, which makes these the most critical stages in episodes of care. Examination of delays showed that for a third of the episodes of care, the assessment necessitated more than 1 visit to be complete. Even so, these delays were associated with more precise diagnoses. The delays measured at the first follow-up (35.6 days±34.14, md=30 days) and at the second (55.9 days±62.7, md=34.0 days) easily surpassed those suggested in the guidelines. The guidelines recommend that the individual be seen again 7–14 days after the initial assessment and that closer monitoring be implemented after that (Citation13, Citation15).
The second objective was to examine whether clinical, individual and organizational characteristics were associated with breaks and delays at various stages in the continuum of care. When breaks occurred, clinical characteristics of episodes of care (prevalence of symptoms and diagnosis accuracy) were most often the cause. For individual and organizational variables, only age (for the continuum as a whole) and composition of the FHSS team (for planning of the first follow-up) showed statistically significant associations.
Not planning a first follow-up visit could have led individuals to think they should return only if symptoms reappeared or worsened. This practice may point towards the adoption of an acute illness management method for CMDs. Yet, current service guidelines for individuals with CMDs advocate follow-up mechanisms based on management models for chronic diseases (Citation13, Citation15) (Citation28, Citation29). These responsive clinical practices in FHSS teams were also found in other studies conducted in Nunavik (Citation7) and other remote regions (Citation30, Citation31). The studies show that these FHSS teams are generally ready to respond to crisis situations, but not as ready when it comes to prevention of mental disorders.
The behaviour of healthcare providers and individuals may be the cause of delays and breaks in the implementation of a first follow-up (Citation32). These delays and breaks can be explained by failures in the healthcare system and show, for example, the poor integration of mental health services between health sectors and social services that can be encountered in the context of Aboriginal peoples and remote regions (Citation7, Citation30). Delays and breaks can also be associated with the lack of commitment to treatment plans (Citation31, Citation33) possibly due to how the Inuit of Nunavik perceive depression. Inuit regard depression as a mental health problem that, when it has no hallucinations, does not require medical or professional help and they view anxiety as a transient situation associated with concerns related to difficult life experiences (Citation3). Coincidentally, Kirmayer and Paul (Citation4) reported that in cases of psychological distress, most Nunavimmiut (persons from Nunavik) consult their loved ones rather than FHSS providers (Citation4).
The rate of breaks for depressive-type episodes in Nunavik FHSSs (34.8%) is similar to those documented for depression in the general population (Citation14), but not so for anxiety-type episodes, most of which (82%) end before the second follow-up visit. This could be because healthcare providers tend to get distracted by somatic symptoms, many of which appear to be cardiac related (Citation31, Citation34). Eliminating physical, drug or substance abuse-related causes of somatic symptoms of anxiety disorders and depression is a normal part of a diagnostic approach (Citation11, Citation13). However, our results suggest that even after attributing observed symptoms to anxiety, FHSS care for individuals in Nunavik remains rudimentary. Finally, the fact that, compared to the older age group, episodes among the 14–20 age group persist after the second follow-up, indicates the availability of more sustained approaches for young people. It would be interesting to document these approaches to learn from them and improve the services offered to adults.
Courses of action
While psychotherapy is often the treatment of choice for individuals with an anxiety disorder (Citation13), this type of treatment is virtually unavailable in Nunavik. Also, results suggest that there are few compensation mechanisms implemented in the region to address the shortage of competent psychotherapists. In similar contexts, initiatives to improve FHSS providers’ cognitive behavioural therapy skills have led to positive experiences when faced with a lack of specialized mental health resources (Citation35, Citation36). Telepsychology, educational interventions and self-care tools adapted for the Inuit are other ways to increase access to quality approaches while promoting empowerment for individuals with anxiety disorders or depression, (Citation31). Results show that more breaks at the planning stage of the first follow-up were documented for the limited FHSS teams. Furthermore, the presence of a precise diagnosis, which suggests the assessment involved a physician or psychologist, meant less premature breaks in the continuum of care. Similar to other studies conducted in remote areas (Citation37), these results show that nurses and social workers should be targeted first in the effort to improve care for individuals with CMDs. Studies have shown that giving nurses a greater role in the treatment and monitoring of individuals with depression significantly increases FHSS quality (Citation38, Citation39).
Strengths and limits
An important strength of the present study is to identify when delays and breaks occur in mental health care trajectories. This information allows targeting more precisely which clinical aspects (e.g. implementation of a first follow-up) have to be improved in priority to influence the whole continuum of care.
In the present study, success, delays and breaks at each stage in the continuum of care are based solely on FHSS activities and not their nature, quality or individual outcomes. Therefore, further work is needed in Inuit Nunangat to document them. It will lead to a better understanding of how FHSSs contribute to the well-being of individuals with CMDs.
In addition, the continuum of care study was conducted using relatively short episodes that reflect only the early stages of the individual's true care trajectories. Even so, there was sufficient time to expose several gaps and to identify courses of action to improve FHSSs in this region.
Broadening selection criteria beyond the medical diagnosis of depressive and anxiety disorders takes into account the underdiagnosis of these conditions in Inuit Nunangat (Citation4, Citation5). This approach fosters awareness and so can include the disease's prodromal stages in the continuum of care study. This choice is made at the expense of specificity and forces us to proceed with caution when considering the results. Moreover, as most other studies are based on medical diagnoses, there is less possibility for comparison.
The use of clinical records as data sources preserves anonymity and reduces desirability bias while circumventing issues related to the recruitment of participants with mental disorders in such small communities. The quality of a retrospective records review depends largely on the quality of notes within the records. Unfortunately, researchers have little control over this aspect. Consequently, the lack of information in certain records could cause breaks in the continuum of care or skew the effect of certain independent variables, such as alcohol and drug consumption, which appear to be underdocumented in clinical records.
Conclusion
The study's results support the recent claim of Inuit Tapiriit Kanatami (ITK), an organization representing the Inuit of Canada, which stated that mental health provisions are a patchwork of services, interventions and support measures (Citation1). Poor management leads to chronicity of conditions, reduced quality of life, adoption of harmful behaviours, an increased suicide risk and a worsening of functional limitations (Citation8).
Quality mental health services rely on clinical approaches sustained over time, between healthcare providers and service levels (Citation12, Citation13) (Citation15). Also, FHSSs must have a greater impact on recovery. To achieve this, it is important to guide the FHSS teams and those service users with CMD towards chronic disease management methods.
The uniqueness of this study rests upon new data obtained on the quality of FHSSs offered to individuals with CMDs in Inuit Nunangat. It provides a method that can also be reproduced in similar isolated settings, where human and financial resources are limited. It helps us better target courses of action and improve them. Furthermore, observing continuums of care over time could be used to monitor changes made to the healthcare services.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study. The Trajectoires project, which provided most of the data for this research, was financed by the Canadian Institutes of Health Research and the Ministère de la Santé et des Services sociaux du Québec within the “Partnerships for Health System Improvement” program. L. Lessard received doctoral scholarships from the Fondation de recherche en sciences infirmiéres du Québec, Quebec's provincial education ministry, the National Network of Aboriginal Mental Health Research and the Canada Research Chair on Comparative Aboriginal Conditions. L. Fournier held a CIHR-FRSQ-MSSS Research Chair in Public Health at the time of this project.
Acknowledgements
The authors would like to thank the research partners for their broad support. These are: the Nunavik Regional Board of Health and Social Services, the Tullatavik and Inuulitsivik health care centres and the Institut national de santé publique du Québec.
References
- Inuit Tapiriit Kanatami. Alianait Inuit mental wellness action plan update. 2012; Ottawa: Inuit Tapiriit Kanatami.
- Hodgins S. Health and what affects it in Nunavik: how is the situation changing?. 1997; Kuujjuaq: Nunavik Regional Board of Health and Social Services.
- Kirmayer LJ, Fletcher C, Corin E, Boothroyd LJ. Inuit concepts of mental health and illness: an ethnographic study. 1994; Montréal: Culture & Mental Health Research Unit.
- Kirmayer LJ, Paul K. Mental health, social support and community wellness. 2008; Quebec: Institut national de santé publique du Québec.
- Haggarty J, Cernovsky Z, Kermeen P, Merskey H. Psychiatric disorder in an Artic community. Can J Psychiatry. 2000; 45: 357–62. [PubMed Abstract].
- Mental Health Commission of Canada. Changing directions, changing lives: the mental health strategy for Canada. 2012; Calgary: Mental Health Commission of Canada.
- Lessard L, Bergeron O, Fournier L, Bruneau S. Contextual study of mental health services in Nunavik. 2008; Quebec: Institut national de santé publique du Québec.
- Boothroyd LJ, Kirmayer LJ, Spreng S, Malus M, Hodgins S. Completed suicides among the Inuit of northern Quebec, 1982–1996: a case-control study. CMAJ. 2001; 165: 749–55. [PubMed Abstract] [PubMed CentralFull Text].
- Government of Canada. The Human Face of Mental Health and Mental Illness in Canada. 2006; Ottawa: Minister of Public Works and Government Services Canada.
- Commissaire à la santé et au bien-être. Pour plus d’équité et de résultats en santé mentale au Québec. 2012; Québec: Commissaire à la santé et au bien-être.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 2000; Washington, DC: American Psychiatric Association. 4th ed., text rev.
- WHO. Integrating mental health into primary care: a global perspective. 2008; Geneva: World Health Organization.
- NICE. Common mental health disorders: identification and pathways to care. 2011; London: National Institute of Clinical Excellence.
- Pence BW, O'Donnell JK, Gaynes BN. The depression treatment cascade in primary care: a public health perspective. Curr Psychiatry Rep. 2012; 14: 328–35. [PubMed Abstract] [PubMed CentralFull Text].
- Fournier L, Roberge P, Brouillet H. Faire face à la dépression au Québec: Protocole de soins à l'intention des intervenants de première ligne [Dealing with Depression in Quebec : Care protocol for primary health care providers]. 2012; Montréal: Centre de recherche du CHUM.
- Lamarche P, Beaulieu MD, Pineault R, Contandriopoulos A-P, Dennis J, Haggerty J. Choices for chance: the path for restructuring primary healthcare services in Canada. 2003; Ottawa: Canadian Health Services Research Foundation.
- WHO. Updated draft: Primary Health Care: a framework for future strategic directions, global report, noncommunicable diseases and mental health evidence and information for policy World Health Organization, WHO/MNC/OSD/03.01. 2003; Geneva: World Health Organization.
- Wierdsma A, Mulder C, de Vries S, Sytema S. Reconstructing continuity of care in mental health services: a multilevel conceptual framework. J Health Serv Res Policy. 2009; 14: 52–7. [PubMed Abstract].
- Statistic Canada. Aboriginal Peoples in Canada in 2006: Inuit, Métis and First Nations, 2006 Census: Findings 2006 [cited 2014 Nov 3]. Available from: https://www12.statcan.gc.ca/census-recensement/2006/as-sa/97-558/index-eng.cfm.
- Government of Quebec. James Bay and Northern Quebec Agreement and Complementary Agreements (JBNQA), Le Publications du Québec. 1998. Available from http://www.collectionscanada.gc.ca/webarchives/20051228173704/; http://www.ainc-inac.gc.ca/pr/agr/que/jbnq_e.html [cited 2014 Nov 3].
- Fournier L, Aubé D, Lessard L, Gauthier J, Bruneau S. Modèles d'organisation des services de première ligne en santé mentale pour les personnes consultant dans les régions du Nunavik et des Terres-Cries-de-la-Baie-James. 2015. Projet de recherche [Organizational Models of Primary Care Services for Mental Health in Nunavik and Eastern James Bay Cree Territory]. Institut de recherche en santé du Canada.
- Lessard L, Fournier L, Gauthier J, Morin D. Assessment of quality of primary care for common mental disorders in isolated communities: taking advantage of clinical records. Rural Remote Health. Forthcoming 2015 July
- Muckle G, Boucher O, Laflamme D. Alcohol, drug use and gambling among the Inuit of Nunavik: epidemiological profile. 2007; Québec: Institut National de santé publique du Québec.
- Fortney J, Sullivan G, Williams K, Jackson C, Morton SC, Koegel P. Measuring continuity of care for clients of public mental health systems. Health Serv Res. 2003; 38: 1157–75. [PubMed Abstract] [PubMed CentralFull Text].
- Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am J Epidemiol. 2003; 157: 364–75. [PubMed Abstract].
- Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996; 49: 1373–9. [PubMed Abstract].
- Patten SB, Wang JL, Williams JV, Currie S, Beck CA, Maxwell CJ, etal. Descriptive epidemiology of major depression in Canada. Can J Psychiatry. 2006; 51: 84–90. [PubMed Abstract].
- Gilbody DS. Review: disease management programmes improve detection and care of people with depression. Evid Based Ment Health. 2004; 7: 80. [PubMed Abstract].
- Gilbody S, Whitty P, Grimshaw J, Thomas R. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA. 2003; 289: 3145–51. [PubMed Abstract].
- Minore B, Boone M, Katt M, Kinch P, Birch S. Facilitating the continuity of care for first nation clients within a regional context. 2001; Ottawa: Canadian Health Services Research Foundation.
- Roy-Byrne PP, Wagner AW, Schraufnagel TJ. Understanding and treating panic disorder in the primary care setting. J Clin Psychiatry. 2005; 66(Suppl 4): 16–22. [PubMed Abstract].
- Neuhauser D. Assessing health quality: the case for tracers. J Health Serv Res Policy. 2004; 9: 246–7. [PubMed Abstract].
- Pepper C, Thompson VM, Nieuwsma JA. Providers’ perceptions of barriers to the treatment of emotional disorders in non-urban primary care clinics. Prim Care Community Psychiatr. 2008; 13: 59–65.
- Roberge P, Fournier L, Duhoux A, Nguyen CT, Smolders M. Mental health service use and treatment adequacy for anxiety disorders in Canada. Soc Psychiatry Psychiatr Epidemiol. 2011; 46: 321–30. [PubMed Abstract].
- Hodgins G, Murray G, Donoghue A, Judd F, Petts A. Introducing a professional development programme to a rural area mental health service: the importance of context. Australas Psychiatry. 2004; 12: 153–60. [PubMed Abstract].
- Bower P, Gilbody S. Managing common mental health disorders in primary care: conceptual models and evidence base. BMJ. 2005; 330: 839–42. [PubMed Abstract] [PubMed CentralFull Text].
- Silverman BE, Goodine WM, Ladouceur MG, Quinn J. Learning needs of nurses working in Canada's First Nations communities and hospitals. J Contin Educ Nurs. 2001; 32: 38–45. [PubMed Abstract].
- Rost K, Nutting PA, Smith J, Werner JJ. Designing and implementing a primary care intervention trial to improve the quality and outcome of care for major depression. Gen Hosp Psychiatry. 2000; 22: 66–77. [PubMed Abstract].
- Machado RJ, Tomlinson V. Bridging the gap between primary care and mental health. J Psychosoc Nurs Ment health Serv. 2011; 49: 24–9. [PubMed Abstract].