Abstract
Objective: To determine the perceived oral health status and treatment needs of Nigerian dental therapists in training and dental technology students.
Methods: A descriptive cross-sectional study of students from Federal School of Dental Therapy and Technology Enugu, Nigeria was conducted using self-administered questionnaire to obtain information on demography, self-reported oral health status, knowledge of impact of oral health on daily life activity, dental attendance and perceived dental need.
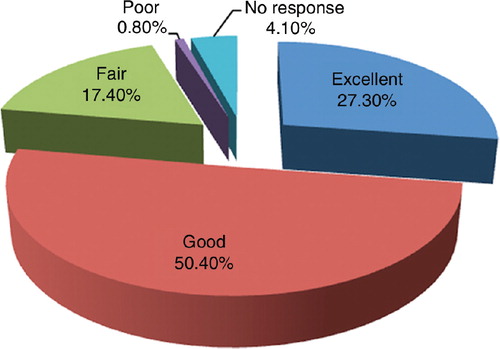
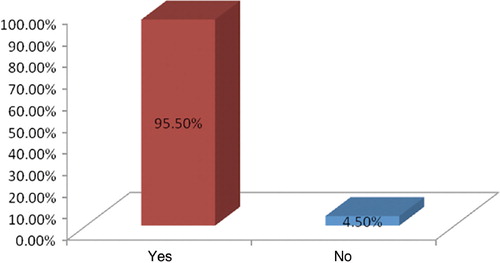
Results: The perception of oral health status and treatment need of the two groups of dental auxiliaries was the same. Fewer respondents (27.3%) rated their oral health as excellent, while 50.4% rated their oral health as good. Majority (95.5%) agreed that oral health is a part of general health and 94.6% agreed that oral health has a role in daily life.
Out of 81.4% that had previous dental treatment, scaling and polishing accounted for 66.1%. Presently, 48.8% think they need dental treatment ranging from scaling and polishing (33.9%), tooth restoration (10.3%), to extraction (1.2%).
Conclusion: This survey revealed that most of the students are aware that oral health is a component of general health and that it has an impact on an individual's daily life. More than half of the students perceived their oral health as good, but only a few knew that there is a need for a preventive approach to oral health as evident by the percentage that perceived scaling and polishing as a treatment need.
Introduction
The perceived oral health is a subjective measure of an individual's perception of his or her oral health Citation1. It has been said that an individual's self-perception of oral health will be determined by the clinical oral conditions and the impact of oral health on daily life Citation2. One measure commonly used is the single-item perceived oral health rating termed ‘How would you rate your overall oral health?’ Citation1. Studies have been conducted in China and other parts of the world using this measure Citation3Citation4Citation5. Self-assessment approaches have been reported to be effective in improving the long-term periodontal health status Citation6.
Patients’ perceived oral health is considered a useful measure of outcome in dentistry because of its relation to the predisposing socio-demographic factors and patients’ utilisation of dental services Citation1. An individual's perception of oral health measures the value attached to oral health and the likelihood of seeking oral care to achieve optimal oral health status.
Oral health problems can impact quality of life in several ways. Poor oral health may prevent children from expressing positive emotions, which can impact their social interactions and the way they feel about themselves Citation7. The periodontal health of adults affects their smiling patterns and their smile-related quality of life. Poor periodontal health may also prevent adults from expressing positive emotions which, in turn, can impact their self-concept as well as their social interactions Citation8. A study on the incidence of impacts of poor oral health on daily performances showed that eating, emotional stability, physical activities and sleeping were affected. Pain and discomfort, due to toothache, were mainly perceived as the causes of impact Citation9.
The most common measure of utilisation of dental services is the annual number of dental visits per person Citation10. Studies involving the assessment of the utilisation of service serve as an important tool for oral health policy decision-making Citation11. The perception of need for dental care will determine whether people in general will seek dental care or not. This perception may be wrong in some cases. It has been found that the perceived oral health in poor populations is incorrect and this may serve as a barrier to their achieving optimal oral health Citation1. A survey on perceived oral health of adult population in a deprived district of Karachi showed that just about half of the participants perceived that they had dental problems which included aesthetic issue, pain, cavities and difficulty in chewing Citation12. The reality of the situation revealed by the study was that majority of the participants had lost many of their teeth, leaving them with only 20 teeth or less Citation12. This implies that there is a gap between their perceived need and the actual need.
Preventive dental visit is part of optimal oral health behaviour recommended by dental professionals. Evidence from several studies shows that the majority of individuals visit the dentist only for symptomatic and curative reason. The most common reason for dentist visit in the literature is pain. Researchers have called for evidence- and community-based dental health education, and a philosophical change from disease-oriented and pain management care to primary preventive care Citation13.
A previous Nigerian study has shown poor utilisation of the available oral health services Citation14, and most people, especially males, only access such services when in pain. Some studies have showed that men tend to visit the dentist more when they are in pain Citation15Citation16Citation17Citation18Citation19. The reasons for non-utilisation range from not knowing that there is a need for such services to unsatisfactory previous dental visit to the fear of the dentist Citation20.
The poor utilisation is not limited to patients alone. It has been found that oral health care givers may actually perceive the need for dental care, but will give a relatively low priority to receiving the needed dental care Citation21.
Since the establishment and maintenance of good general and oral health is a priority, and a key factor in enabling adults to achieve overall well-being and improved quality of life, it is important to assess how individual rate their oral health status, their perceived dental need and actual utilisation of available dental services. The students of Federal School of Dental Therapy and Technology Enugu, Nigeria were recruited for this study. This study group is important because they are the future oral health care givers and it is very desirable that they have the right knowledge and proper oral health practices.
The objective of this study was to determine the perceived oral health status, dental treatment needs and the utilisation of dental services by students training to be dental therapists and dental technology students in Nigeria.
2 Materials and methods
A descriptive cross-sectional study of 242 students of Federal School of Dental Therapy and Technology Enugu, Nigeria was conducted. Self-administered questionnaire was used to obtain information on demography, self-reported oral health status, knowledge of impact of oral health on daily life activity, dental attendance and perceived dental need.
The ethical approval of this survey was obtained from University of Benin Teaching Hospital Ethics Committee. Informed consent was obtained from participants before the commencement of the survey. Statistical Package for Social Science (SPSS version 15.0) was used for data analysis and Chi Square was used for test of significance. The result was presented as tables, pie chart and bar charts.
3 Results
Most of the respondents (75.2%) were within the 20–25 age group. There were more females (61.2%) and almost all were single (95.5%) (). The percentage of respondents that rated their oral health as good and excellent was 50.4% and 27.3%, respectively (). Majority (95.5%) agreed that oral health is part of general health (). Almost all the respondents (94.6%) agreed that oral health has a role in daily life (). About 80.1% of respondents had utilised dental service in the past for various reasons. Scaling and polishing of teeth was the treatment done in 66.1% of cases (). Presently, 48.8% of respondents think that they still need other dental treatments. The perceived treatment needs are scaling and polishing (33.9%), fillings (10.3%), extraction (1.2%) and advanced restorations/prostheses (2%) ().
Figure 3. Respondents who believe that oral health has an impact on daily life activity of individuals.
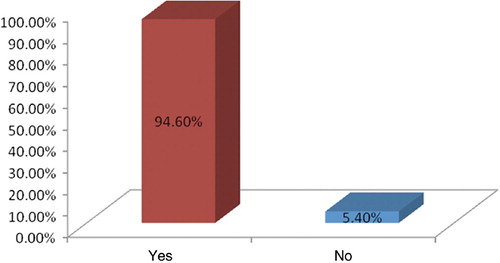
Table 1. Demographic variables of the respondents
Table 2. Distribution of previous treatment received by respondents
Table 3. Respondents’ perceived treatment need
4 Discussion
Oral health is now an important component of general health and there is an increasing awareness of oral health worldwide. A lot has been done by the World Health Organization Global Oral Health Programme in the last five years to increase this awareness Citation22. Oral diseases have obvious impact on daily activities, such as eating, speech and swallowing and have been measured in several studies using oral health quality of life index and oral health impact index. In this study, the awareness is high as majority (95.5%) agreed that oral health is part of general health and 94.6% agreed that oral health has a role in daily life. The result is similar to that from a study done in Brazil Citation23, where it was concluded that oral health conditions generate a significant impact on individuals’ quality of life. Oral health was regarded as important by a majority of the students (95%) in a previous study Citation24.
Personal rating of one's own health status is subjective, but self-efficacy ascertained from it is instrumental to the benefit attached to the health parameter being measured. In this study, those who rated their oral health as good and excellent were 50.4% and 27.3%, respectively. This shows that few people are still not sure of their oral health status and are sincere enough to own up. This result may just be a reflection of what is truly obtainable in the studied group. This result is also in accordance with a study from China Citation5, where self-assessment of dental health of Chinese adolescents was generally good. Only 12% of the students who participated in the Chinese study rated their oral health as ‘poor’ or ‘very poor’.
The study showed that 19.8% of the students have never been to a dentist in their life time. (The mean age of the participants is 23±4 years.) This is of interest since oral health practitioners recommend that a child should see a dentist six months after the eruption of the first tooth Citation25. It is said that taking a child to the dentist at a young age is the best way to prevent problems, such as tooth decay, help parents learn how to clean the child's teeth and to identify his or her fluoride needs. This leads to a lifetime-good oral care habits and ensure stress free visits in the future. The utilisation of dental services reported in this study is better than that reported by another Nigerian study carried out among nursing students Citation26. Here, the researchers reported that 68% of the nursing students had never visited a dentist before. The difference in the two groups may be due to poor exposure of nursing students to dentistry. Dental auxiliaries on the other hand take courses in various areas of dentistry.
Out of 80.1% of the respondents that had dental treatment prior to the study, scaling and polishing accounted for 66.1%. Presently, only 48.8% perceived a need for scaling and polishing at a future date. The results suggest a relatively low priority for receiving needed dental care similar to that reported among dental students Citation21. It has been said that regular dental checkups and treatment are the cornerstones of good oral health Citation27. This study suggests that the respondents are not utilising the dental services optimally as none of them will visit the dentist just for routine dental examination.
5 Conclusion
This survey revealed that most of the students are aware that oral health is a component of general health and that it has an impact on an individual's daily life. More than half of the students perceived their oral health as good, but only a few knew that there is a need for a preventive approach to oral health as evident by the percentage that perceived scaling and polishing as a treatment need. To improve the utilisation of the existing dental services, it is recommended that periodic oral health education be carried out among this group of students. They are expected to be knowledgeable about oral health issues by virtue of their training, but it should not be assumed that they will do the expected.
6 Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- Atchison KA, Gift HC. Perceived oral health in a diverse sample. Adv Dent Res. 1997; 11: 272–80.
- Jones JA, Kressin NR, Spiro A 3rd, Randall CW, Miller DR, Hayes C, et al.. Self-reported and clinical oral health in users of VA health care. J Gerontol A Biol Sci Med Sci. 2001; 56: M55–62.
- Jones JA, Kressin NR, Miller DR, Orner MB, Garcia RI, Spiro A 3rd. Comparison of patient-based oral health outcome measures. Qual Life Res. 2004; 13: 975–85.
- Ostberg AL, Lindblad U, Halling A. Self-perceived oral health in adolescents associated with family characteristics and parental employment status. Community Dent Health. 2003; 20: 159–64.
- Jiang H, Petersen PE, Peng B, Tai B, Bian Z. Self-assessed dental health, oral health practices, and general health behaviors in Chinese urban adolescents. Acta Odontol Scand. 2005; 63: 343–52.
- Nowjack-Raymer R, Ainamo J, Suomi JD, Kingman A, Driscoll WS, Brown LJ. Improved periodontal status through self-assessment. A 2-year longitudinal study in teenagers. J Clin Periodontol. 1995; 22: 603–8.
- Patel RR, Tootla R, Inglehart MR. Does oral health affect self perceptions, parental ratings and video-based assessments of children's smiles?. Community Dent Oral Epidemiol. 2007; 35: 44–52.
- Patel RR, Richards PS, Inglehart MR. Periodontal health, quality of life, and smiling patterns – an exploration. J Periodontol. 2008; 79: 224–31.
- Adulyanon S, Vourapukjaru J, Sheiham A. Oral impacts affecting daily performance in a low dental disease Thai population. Community Dent Oral Epidemiol. 1996; 24: 385–9.
- King T. Tooth brushing and utilization of dental services in Fiji (1998). Pac Health Dialog. 2003; 10: 23–7.
- Manski RJ, Moeller JF, Maas WR. Dental services. An analysis of utilization over 20 years. J Am Dent Assoc. 2001; 132: 655–64.
- Tanwir F, Altamash M, Gustafsson A. Perception of oral health among adults in Karachi. Oral Health Prev Dent. 2006; 4: 83–9.
- Goodman HS, Macek MD, Wagner ML, Manz MC, Marrazzo ID. Self-reported awareness of unrestored dental caries. Survey of the Oral Health Status of Maryland Schoolchildren, 2000–2001. Pediatr Dent. 2004; 26: 369–75.
- Agbelusi GA, Jeboda SO. Oral health status of 12-year-old Nigerian children. West Afr J Med. 2006; 25: 195–8.
- Tubaishat RS, Darby ML, Bauman DB, Box CE. Use of miswak versus toothbrushes: oral health beliefs and behaviours among a sample of Jordanian adults. Int J Dent Hyg. 2005; 3: 126–36.
- Reisine S. A path analysis of the utilization of dental services. Community Dent Oral Epidemiol. 1987; 15: 119–24.
- Tubert-Jeannin S, Riordan PJ, Morel-Papernot A, Roland M. Dental status and oral health quality of life in economically disadvantaged French adults. Spec Care Dentist. 2004; 24: 264–9.
- KIrtIloğlu T, Yavuz US. An assessment of oral self-care in the student population of a Turkish university. Public Health. 2006; 120: 953–7.
- Al-Omari QD, Hamasha AA. Gender-specific oral health attitudes and behavior among dental students in Jordan. J Contemp Dent Pract. 2005; 6: 107–14.
- Akaji EA, Oredugba FA, Jeboda SO. Utilization of dental services among secondary school students in Lagos, Nigeria. Niger Dent J. 2007; 15: 87–91.
- Coleman GC, Barnes GP, Tollefsbol RG, Nelson JF. Dental care utilization among dental students. Ann Dent. 1991; 50: 12–7.
- Petersen PE. Global policy for improvement of oral health in the 21st century – implications to oral health research of World Health Assembly 2007, World Health Organization. Community Dent Oral Epidemiol. 2009; 37: 1–8.
- Lacerda JT, Bona C, Tacca F, Traebert J. Oral health-related impact on daily life in a sample of adults of Tubarao city, Santa Catarina, Brazil. Rev Odontol UNESP. 2009; 38: 148–53.
- Ostberg AL, Lindblad U, Halling A. Gender differences in knowledge, attitude, behavior and perceived oral health among adolescents. Acta Odontologica. 1999; 57: 231–6.
- Academy of General Dentistry. Children's oral health. Available from: http://www.agd.org/public [cited 25 January 2009].
- Udoye C, Aguwa E. Oral health related knowledge and behavior among nursing students in a Nigerian tertiary hospital. Int J Dental Sci. 2009; 7: 2.
- Turtola L. Systematic dental health care among Finnish University students. Proc Finn Dent Soc. 1991; 87: 637–42.