Abstract
The author, a parent of a child with autism, describes an n=1 case in which his child's autism symptoms dramatically and rapidly improved following administration of a common antibiotic. The author asserts that this finding is not unusual in the autism population and that, when combined with prior recent medical research, suggests that a link between autism and the microbiome in some children is not just plausible, but in fact likely for some meaningful percentage of cases. The author argues for increased funding for a more thorough examination of links between autism and the microbiome and poses a series of questions to be further examined in future research.
This paper is part of the Supplement: The Microbiome in Autism Spectrum Disorder. More papers from this supplement can be found at http://www.microbecolhealthdis.net
Thanksgiving Day in the United States is usually a quiet time with family, unless both of your young children contract strep throat while visiting family as ours did in 2012. Because it was a holiday, my wife and I took them to an extended-hours clinic, where a physician confirmed strep via a rapid strep test and prescribed a 10-day course of amoxicillin, one of the most commonly prescribed antibiotics in the United States. Neither had received an antibiotic before and in 2 days they seemed back to normal. This would not be a very interesting story except for what happened next.
Earlier that year our son had been diagnosed with moderate-to-severe autism by a team of clinicians and practitioners at Children's Medical Center in Dallas, Texas. On day four of his 10-day course of amoxicillin, we began noticing changes in his autism symptoms: he began making eye contact, which he had previously avoided; his speech, which was severely delayed, began to improve markedly; he became less ‘rigid’ in his insistence for sameness and routine; and he also displayed an uncharacteristic level of energy, which he had historically lacked. The improvements continued each day. On day six he rode a tricycle around the room for the first time, alone and unprompted, which was remarkable because we had purchased the tricycle 6 months earlier and had worked with him continuously so he could learn to ride it, however until that point, he had never so much as been able to push the pedals enough to move forward.
Although we had previously seen transient improvement in our son's autism symptoms when he had a fever, as others have documented (Citation1), he had no fever now and we had never seen any improvement of this magnitude. Some may question the accuracy and validity of parental observations. Since his diagnosis I have used customized software to track more than 20 different parameters of his autism with a rating system that I devised. In addition, the software allows me to capture daily qualitative observations. I feel confident the improvements we saw were real, significant, and unprecedented. It is important to note that, in addition to my own observations, his therapists made unsolicited comments about how much better he seemed, although they were unaware of the antibiotic he was taking at that time or of my perceptions of his gains. I would encourage any parent that believes they are observing a similar phenomenon to take detailed, careful notes and obtain as much video documentation as possible, because such information may prove useful in the future.
Why so little study?
The obvious questions I asked were “what was happening?” and, “why were we seeing these improvements?” We asked other parents of children with autism spectrum disorder (ASD) and many had observed similar changes while taking antibiotics. In fact, we discovered, much to our surprise, that many parents of autistic children routinely give their children antibiotics to improve their symptoms. It should also be noted, however, that we later also heard from some parents that felt that their children's autism symptoms became worse when they received antibiotics, whereas still others felt that that their children's autism only arose after repeated or long-term antibiotic use. In my view, these stories are not contradictory but rather reinforce the notion that an antibiotic can create an effect in autism. I was determined to better understand this phenomenon because I believed that if we could understand the biological basis of his improvements, we might gain insight into how autism works and be able to help him.
To try and understand the link between autism and antibiotics further, I reviewed the medical literature and found a single relevant paper that described a clinical trial that gave vancomycin, an antibiotic that is not systemically absorbed when taken orally, to a small group of severely autistic children as part of a clinical research study at Chicago Rush Children's hospital (Citation2). Eight out of ten of these children experienced a marked improvement in their autism symptoms. The authors speculated that the improvements were likely triggered by changes in the gut microbiome resulting from the antibiotic. I looked for additional studies, directly related to this ‘antibiotic effect’ in autism. I found none.
To this day I remain confused by the lack of follow-up studies on this commonly observed phenomenon. Despite the alarming rise in autism (discussed below), we still do not know what autism is. There are no universal medical treatments and a mechanism or etiology remains elusive. Yet, I personally witnessed evidence that this seemingly intractable condition could be rapidly and dramatically ameliorated in response to an antibiotic, at least for some children, but surprisingly there were no attempts to repeat this study, even as a means to study it mechanistically or to subtype patients.
The latest numbers from the US Centers for Disease Control and Prevention (based on data for 2010) estimate the prevalence of ASD to be 1:68 (and 1:42 for boys) (Citation3). The prevalence estimates rise every year the statistics are compiled. One study put the number as high as 1:29 (Citation4). It is difficult to think of another medical condition with such a wide and growing prevalence that science cannot say what it is: neurological, genetic, infectious, autoimmune, metabolic? All of the above? Although it is almost certainly a heterogeneous condition, for years the conventional wisdom has been that autism is a developmental disorder, largely driven by genetics where the associated behaviors and symptoms are a by-product of abnormal neuronal development and connectivity. When our child was diagnosed we were told, like so many other parents, ‘We don't know what it is, but he will not just outgrow it’. The conventional view suggests it is a ‘wiring’ problem, but the evidence we observed on Thanksgiving of 2012 suggested something very different.
After speaking with some of the original authors of the Sandler et al. paper (Citation2), as well as other key researchers in the field, I found that there was substantial interest in continuing the investigation into this ‘antibiotic effect’ and in exploring the links between autism and the microbiome. The consistent message I heard from researchers, however, was that it was almost impossible to get funding for projects like these from the handful of public and private organizations that fund autism research because most in those organizations simply do not believe that there is enough evidence that a link exists - it does not fit the current paradigm of a genetically driven cause for ASD. If the history of science has taught us anything, it is that real breakthroughs do not occur until paradigms shift, and that that process can be messy and full of controversy (Citation5).
Growing evidence of a link
In reviewing the literature, I have come to rely on a handful of papers to serve as a starting point for what may be going on (Citation2, Citation6–Citation9). The good news is that this area seems to be gaining momentum, though not because of an improvement in the funding picture, but because the scientific evidence of a link seems to be accumulating.
The evidence suggesting a link between autism and alterations in the microbiome,Footnote at least for some children, is strong and continues to build in momentum: several studies have now shown that, compared to neurotypical children, children with autism as a group have compositional changes in their gut microbiomes, as well as less species diversity (Citation6, Citation8–Citation15). Some papers have found species in children with autism that they did not find in controls, for example (Citation6, Citation8). A recent meta-analysis of all autism and gut microbiome studies concluded that there were consistent differences in the gut bacteria of groups of ASD patients compared to healthy controls, although the compositional differences were inconsistent (Citation16). This is not surprising given the great variation in our diets (a powerful driver of gut microbiome composition) (Citation17), or the restrictive food interests and specialized diets of many ASD children. The lack of standardized approaches, including what type of sample is used (stool vs. biopsy), collection techniques, and how the samples are analyzed, could contribute to inter-study variances. However, the point remains that regardless of experimental conditions, when examined, children with autism have consistently been found to have differential gut bacterial compositions, compared to controls.
How might such differences come about?
If one accepts the premise that there are differences in the gut microbiome of ASD vs. neurotypical children (and more research needs to be done on this alone), a logical question is how and when during development might this come about? Intriguing evidence has come from a very recent study showing gut microbiome variations in the maternal immune activation (MIA) mouse model of autism (Citation7). In this well-studied model, pregnant mice are given a simulated infection, which triggers an immune response. The male offspring of those pregnant immune-activated mice develop autism-like symptoms (Citation7, Citation18–Citation21). More recently, the offspring were found to have different gut bacterial compositions compared to controls. What is striking about this finding is that from birth these mice were grown under identical lab conditions and received identical food (Citation7) – something that could not be done with human subjects. Regardless of whether this particular mouse model is representative of autism, the fact that a prenatal, immunological event results in a different gut microbiome under highly controlled conditions is a fascinating finding. This finding suggests that the differences seen in the gut bacteria of the mice were not a result of chance but perhaps allowed or enabled by the changes provoked by the mother's simulated infection. The question of how this process occurs and what it means becomes critical here, and it is an important one to investigate thoroughly as we may be flirting with a core mechanism of the development of autism. Do the emergent autistic-like behaviors exhibited by the mice arise from changes provoked by the maternal infection or the shifts in the gut microbiota that develop? Interestingly, many of the young mice's autistic behaviors were corrected by the administration of a bacterial probiotic (Citation7).
Could there be microbes that are required for normal development? As mentioned earlier, some parents feel that repeated or long-term antibiotic use was a trigger for their child's autism. It is frequent topic of public debate that antibiotics are overused. The gut microbiome of newborns and babies change and mature dramatically in the first few years of life (Citation22, Citation23). Is it possible that in some cases disrupting the development of gut microbiome through repeated antibiotic use early in life could set the stage for the development of autism in some children?
As described in Sandler et al. (Citation2), as well as anecdotally according to parents who have seen a similar antibiotic effect, when the drug is withdrawn, the children lose their gains or at least stop making them. Is this a sign that the source of improvement is a result of some yet unknown action of the antibiotics or a result of the gut flora returning to its previous state? It is possible that the mechanism could be due to the antibiotic working in some non-antimicrobial way we are not familiar with. However, the fact that some lose their gains quickly (days) following removal of the antibiotic, whereas others lose them slowly (weeks and months) and still others keep their improvements, seems more consistent to me with changes in gut microbiome brought about by the antibiotic rather than some non-antimicrobial action of the antibiotic. Although it is known that most antibiotics have dramatic effects on the gut microbiome (Citation24), the degree to which it recovers following withdrawal of an antibiotic is variable from person to person (Citation25). Does this return to a previous state coincide with the return of ASD symptoms in those antibiotic-responders? Any study of these responding children should closely examine the relationship between the return of autism symptoms (or loss of gains) and the return of the gut microbiome to a stable state.
What might cause differences in the gut microbiome in children with ASD to begin with? Hsiao et al. showed one possible trigger, in the animal model used, was an early immunological event; but, by what mechanism might this occur? Is it possible that in some cases of autism there is an immunological shift that permits some potentially problematic species to thrive or that blocks colonization by other beneficial species? Or could the altered microbiome simply be a by-product of an ASD-induced alteration in the physiological conditions of the gastrointestinal tract (e.g. altered nutritional adsorption, pH, redox states) that favor a different ecological landscape in the guts of these children, much like different climates on Earth favor different plants and animals? Is there such a thing as an autism-driven ecology that is a by-product of autism but that contributes to some of its symptoms?
What might be going on and by what mechanism?
Many people think they know why some children with autism have a positive response to antibiotics. I do not. Many parents and even clinicians strongly believe that the benefits seen from antibiotics are a result of killing a specific, problematic bacterium. This view has the benefit of simplicity and fits the limited data well; however, the problem is that despite some extensive searching, a ‘bad’ bacterial species responsible for autism has not yet been found. That is not to say that one may not be found. Indeed, the current approach to the identification of bacterial species using 16S ribosomal RNA gene libraries necessitates that we know what we are looking for in advance; however, the bacterial species ‘catalogs’ that scientists use with this technique are incomplete. It is also theoretically possible that a so-called ‘bad’ species could have a 16S region so similar to that of another known species that it could be practically invisible using this particular characterization technique. Importantly, knowing which species are present does little to tell us about what they are capable of doing.
Although the concept of a ‘bad’ species in ASD is seductive, other hypotheses need to be considered and studied in parallel. Instead of the presence of a ‘bad’ species, perhaps it is the absence of certain beneficial species that is important. Moreover, the entire construct of species may be the wrong one. Bacteria frequently share DNA in ways that are foreign to our human way of thinking. A more beneficial construct may be to think about the functional genome or even metabolic capability or output of the microbial community (Citation26). Such a paradigm shift may put the disparate findings of those early studies that have looked at gut bacterial composition in ASD in a whole new light or may even render that way of thinking an impediment to what is really going on. Thinking about species may be a case of not being able to see the forest for the trees.
Recent advances in the field of metabolomics have dramatically improved the number of metabolites that can be detected and characterized. A meaningful percentage of those metabolites are by-products of microbial ecology (Citation27), any number of which could be interfering with core cellular metabolism, gene regulation, neuronal transmission, or other perturbations commonly observed in autism. Hsaio et al. showed that the metabolite 4-ethly-phenyl sulfate (4EPS) was found at levels 46 times higher in the affected mice compared with controls. After rescue by a probiotic, the levels of 4EPS dropped to normal. When 4EPS was injected into the bloodstream of healthy mice, they developed some of the abnormalities seen in the MIA mice (Citation7). MacFabe et al. have reported similar findings for propionic acid, a short-chain fatty acid that is a known fermentative by-product of certain gut microbial species and that is also used as a preservative by the food industry (Citation28–Citation30). These findings argue for further investigations into the possible role of microbial metabolites in ASD.
Much exciting autism research in recent years has been devoted to the metabolic abnormalities commonly observed in autism, in particular those related to mitochondrial pathways (Citation20, Citation31–Citation33). Historically this work was not linked to the microbiome, however, this is beginning to change (Citation21, Citation28) (Citation34). Indeed the metabolic and catabolic processes of our mammalian cells and the microbiome may be an intricate biochemical dance – one that works well in health but improperly in autism.
Although it is possible that metabolic by-products of the microbiome such as 4EPS are directly responsible for some behaviors associated with autism, it is also possible that alterations of the microbiome may somehow dysregulate immunity and lead to the formation of autoantibodies. The proposed molecular mimicry mechanism of PANDAS (Pediatric Autoimmune Neuropsychiatric Disorder Associated with Streptococcal infections), which sometimes co-occurs with autism, serves as one example of where the presence of certain bacteria is thought to create antibodies reactive with the basal ganglia resulting in behavioral abnormalities (Citation35).
In summary, there is no shortage of proposed mechanisms: presence or absence of certain species or functional genes, metabolic by-product or toxin, molecular mimicry, provocation of cellular or immune hyper-responsiveness, and others. Each proposed mechanism has its own intriguing strands of evidence and plausibility worth consideration and further inquiry.
A way forward
There is compelling evidence of a link between autism and the microbiome in at least a subset of children. Are the microbial abnormalities observed in autism merely a superfluous by-product of autism, or are they at the root of its cause or symptomology? Science will eventually tell us, but for me the simple fact that my child and many others like him improved dramatically while taking an antibiotic suggests the latter.
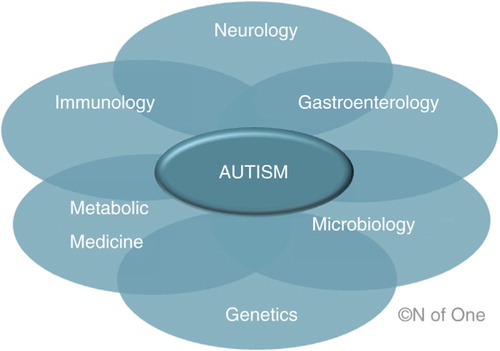
The true devil, however, will be in the details: long-term use of antibiotics does not seem like a good option or treatment approach because of its potential to further disrupt the microbiome and promote resistance. To tease apart what may be going on will take a tremendous commitment of resources and can only be done in a highly collaborative, multidisciplinary way. To even begin to address some of the questions posed in this paper requires expertise in disparate fields of medicine and science (), many of which have historically had little reason to collaborate. Such cooperation will require a departure from the typically siloed nature of medical research and (perhaps more importantly) how grants are made. But it can be done, indeed it must be done!
In early 2014, I formed the N of One: Autism Research Foundation, with the mission of encouraging, sponsoring, and communicating breakthrough autism research. Our focus is to garner support for promising research areas that we believe are not receiving sufficient funding relative to their scientific merit. Additionally, we favor research that treats the observations of parents and doctors as clues to the mechanism of autism. Research into the microbiome's role in ASD fits both of those conditions well.
In February of 2014, working with Dr. Richard Frye at Arkansas Children's Hospital, we came up with the idea of assembling an interdisciplinary group of experts to address what could be done to further investigate the antibiotic effect first documented in 2000 (Citation2). This group included both Dr. Sydney Finegold and Ellen Bolte, authors of that original paper. The group considered investigations into the microbiome and autism that might provide insight into mechanism or therapeutic benefit. An in-person meeting was held on June 27, 2014, in Little Rock, Arkansas, to discuss further the development of a clinical research trial. An additional day was set aside to conduct a conference, free and open to the public, dedicated to topics surrounding autism and the microbiome. The point of the conference was to increase awareness of possible links between autism and the microbiome and to bring together interested members of the scientific community as well as parents to discuss, collaborate, and exchange ideas on this subject. That same group of researchers decided to publish this special issue, and I am proud and honored to be a part of that group. I am appreciative that scientists and clinicians would ask an ordinary parent to contribute to this journal.
At the time of his diagnosis, we had been led to believe that our son's autism was a hard-wired neurological condition from which he would not emerge, but during the fall and winter of 2012 and subsequent periods since then we have seen our son with the veil of autism partially lifted. I love him unconditionally regardless of his autism or how he is doing on any given day, but because I have seen what is possible, I will endeavor to promote research that benefits all children with autism and to remove all impediments from him becoming the fullest embodiment of who he can be and until it is definitively proven otherwise, I will strive to foster research consistent with the evidence of the microbiome's involvement in autism.
Conflict of interest and funding
The author has not received any funding or benefits from industry or elsewhere to conduct this study.
Acknowledgements
The author wishes to thank Ellen Bolte, Emma Allen-Verco PhD, and John Slattery for their helpful discussion and comments on the manuscript.
Notes
This paper is part of the Supplement: The Microbiome in Autism Spectrum Disorder. More papers from this supplement can be found at http://www.microbecolhealthdis.net
1In this paper, the term microbiome is primarily used to mean the collection of bacteria that live on and in humans, the vast majority of which reside in the gut. However, this definition is incomplete as it does not also include the myriad of archaea, yeasts, fungi, protists, viruses, etc., that comprise the human microbial ecosystem and contribute to its genetic and metabolic diversity
References
- Curran LK , Newschaffer CJ , Lee LC , Crawford SO , Johnston MV , Zimmerman AW . Behaviors associated with fever in children with autism spectrum disorders. Pediatrics Dec. 2007; 120: e1386–92.
- Sandler RH , Finegold SM , Bolte ER , Buchanan CP , Maxwell AP , Väisänen ML , etal. Short-term benefit from oral vancomycin treatment of regressive-onset autism. J Child Neurol. 2000; 15: 429–35.
- Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators, Centers for Disease Control and Prevention. Prevalence of autism spectrum disorder among children aged 8 years – autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ. 2014; 63: 1–21.
- Kim YS , Leventhal BL , Koh YJ , Fombonne E , Laska E , Lim EC , etal. Prevalence of autism spectrum disorders in a total population sample. Am J Psychiatry. 2011; 168: 904–12.
- Kuhn TS . The structure of scientific revolutions. 1962; Chicago: University of Chicago Press.
- Finegold SM , Dowd SE , Gontcharova V , Liu C , Henley KE , Wolcott RD , etal. Pyrosequencing study of fecal microflora of autistic and control children. Anaerobe. 2010; 16: 444–53.
- Hsiao EY , McBride SW , Hsien S , Sharon G , Hyde ER , McCue T , etal. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell. 2013; 155: 1451–63.
- Williams BL , Hornig M , Parekh T , Lipkin WI . Application of novel PCR-based methods for detection, quantitation, and phylogenetic characterization of Sutterella species in intestinal biopsy samples from children with autism and gastrointestinal disturbances. MBio. 2012; 3: e00261–11.
- Williams BL , Hornig M , Buie T , Bauman ML , Cho Paik M , Wick I , etal. Impaired carbohydrate digestion and transport and mucosal dysbiosis in the intestines of children with autism and gastrointestinal disturbances. PLoS One. 2011; 6: e24585.
- Adams JB , Johansen LJ , Powell LD , Quig D , Rubin RA . Gastrointestinal flora and gastrointestinal status in children with autism – comparisons to typical children and correlation with autism severity. BMC Gastroenterol. 2011; 11: 22.
- De Angelis M , Piccolo M , Vannini L , Siragusa S , De Giacomo A , Serrazzanetti DI , etal. Fecal microbiota and metabolome of children with autism and pervasive developmental disorder not otherwise secified. PLoS One. 2013; 8: e76993.
- Kang DW , Park JG , Ilhan ZE , Wallstrom G , Labaer J , Adams JB , etal. Reduced incidence of Prevotella and other fermenters in intestinal microflora of autistic children. PLoS One. 2013; 8: e68322.
- Parracho HM , Bingham MO , Gibson GR , McCartney AL . Differences between the gut microflora of children with autistic spectrum disorders and that of healthy children. J Med Microbiol. 2005; 54: 987–91.
- Song Y , Liu C , Finegold SM . Real-time PCR quantitation of clostridia in feces of autistic children. Appl Environ Microbiol. 2004; 70: 6459–65.
- Wang L , Christophersen CT , Sorich MJ , Gerber JP , Angley MT , Conlon MA . Increased abundance of Sutterella spp. and Ruminococcus torques in feces of children with autism spectrum disorder. Mol Autism. 2013; 4: 42.
- Cao X , Lin P , Jiang P , Li C . Characteristics of the gastrointestinal microbiome in children with autism spectrum disorder: a systematic review. Shanghai Arch Psychiatry. 2013; 25: 342–53.
- Voreades N , Kozil A , Weir TL . Diet and the development of the human intestinal microbiome. Front Microbiol. 2014; 5: 494.
- Malkova NV , Yu CZ , Hsiao EY , Moore MJ , Patterson PH . Maternal immune activation yields offspring displaying mouse versions of the three core symptoms of autism. Brain Behav Immun. 2012; 26: 607–16.
- Patterson PH . Maternal infection and immune involvement in autism. Trends Mol Med. 2011; 17: 389–94.
- Naviaux RK , Zolkipli Z , Wang L , Nakayama T , Naviaux JC , Le TP , etal. Antipurinergic therapy corrects the autism-like features in the poly(IC) mouse model. PLoS One. 2013; 8: e57380.
- Naviaux JC , Schuchbauer MA , Li K , Wang L , Risbrough VB , Powell SB , etal. Reversal of autism-like behaviors and metabolism in adult mice with single-dose antipurinergic therapy. Transl Psychiatry. 2014; 4: e400.
- Blaser MJ , Falkow S . What are the consequences of the disappearing human microbiota?. Nat Rev Microbiol. 2009; 7: 887–94.
- Garrido D , Dallas DC , Mills DA . Consumption of human milk glycoconjugates by infant-associated Bifidobacteria: mechanisms and implications. Microbiology. 2013; 159: 649–64.
- Modi SR , Collins JJ , Relman DA . Antibiotics and the gut microbiota. J Clin Invest. 2014; 124: 4212–18.
- Dethlefsen L , Relman DA . Incomplete recovery and individualized responses of the human distal gut microbiota to repeated antibiotic perturbation. Proc Natl Acad Sci USA. 2011; 108: 4554–61.
- Toh MC , Allen-Vercoe E . The human gut microbiota with reference to autism spectrum disorder: considering the whole as more than a sum of its parts. Microb Ecol Health Dis. 2015; 26 26309, doi: http://dx.doi.org/10.3402/mehd.v26.26309 .
- Wikoff WR , Anfora AT , Liu J , Schultz PG , Lesley SA , Peters EC , etal. Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc Natl Acad Sci USA. 2009; 106: 3698–703.
- Macfabe D . Autism: metabolism, mitochondria, and the microbiome. Glob Adv Health Med. 2013; 2: 52–66.
- Macfabe DF . Short-chain fatty acid fermentation products of the gut microbiome: implications in autism spectrum disorders. Microb Ecol Health Dis. 2012; 23 19260, doi: http://dx.doi.org/10.3402/mehd.v23i0.19260 .
- MacFabe DF , Cain NE , Boon F , Ossenkopp KP , Cain DP . Effects of the enteric bacterial metabolic product propionic acid on object-directed behavior, social behavior, cognition, and neuroinflammation in adolescent rats: relevance to autism spectrum disorder. Behav Brain Res. 2011; 217: 47–54.
- James SJ , Cutler P , Melnyk S , Jernigan S , Janak L , Gaylor DW , etal. Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am J Clin Nutr. 2004; 80: 1611–17.
- Frye RE , Delatorre R , Taylor H , Slattery J , Melnyk S , Chowdhury N , etal. Redox metabolism abnormalities in autistic children associated with mitochondrial disease. Transl Psychiatry. 2013; 3: e273.
- Frye RE , James SJ . Metabolic pathology of autism in relation to redox metabolism. Biomark Med. 2014; 8: 321–30.
- Frye RE , Melnyk S , Macfabe DF . Unique acyl-carnitine profiles are potential biomarkers for acquired mitochondrial disease in autism spectrum disorder. Transl Psychiatry. 2013; 3: e220.
- Williams KA , Swedo SE . Post-infectious autoimmune disorders: Sydenham's chorea, PANDAS and beyond. Brain Res. 2014. (in press).