Abstract
Hand and upper extremity transplantation offers a promising reconstructive solution for select patients lacking a functional upper limb. For such an endeavor, it is imperative that multiple medical and surgical specialties and teams work in concert to achieve a common goal. Sixteen years from the first successful hand transplantation, the number of centers performing or planning to perform hand transplantation worldwide has increased considerably. This procedure may become the standard of care for properly selected patients in the not-too-distant future. To facilitate this transition, unified protocols are required. In this manuscript, we focus on the donor limb procurement process, including the sequence of events, logistics, and inter-specialty team interaction. Through review of the current literature, we acknowledge and address possible variations, and provide an illustrative overview of the operation. It is important that all members involved in this procedure, including the Organ Procurement Organization (OPO), solid organ procurement teams, and donor hospital staff, are aware of this process. Opportunities for future research in this field are further discussed.
Abbreviations:
- CMV, vytomegalovirus
- EBV, Epstein-Barr virus
- IRHCTT, International Registry of Hand and Composite Tissue Transplantation
- HBV, hepatitis b virus
- HCV, hepatitis c virus
- HIV, human immunodeficiency virus
- HLA, human leukocyte antigen
- HSV, herpes simplex virus
- HTK, histidine-tryptophan-ketoglutarate
- LCP, locking compression plates
- OPO, organ procurement organization
- OPTN, Organ Procurement and Transplantation Network
- OR, operating room
- PRA, panel reactive antibodies
- SOT, solid organ transplantation
- UNOS, United Network for Organ Sharing
- USO, ulnar shortening osteotomy
- UW, University of Wisconsin
- VCA, vascularized composite allotransplantation
- VZV, Varicella-Zoster virus
Introduction
Successful hand transplantation requires careful recipient selection, appropriate donor-recipient matching, extensive and well-rehearsed operative planning, teamwork, meticulous surgical technique, diligent follow-up, and proactive rehabilitation.Citation1,2 The technical and immunological feasibility of hand and upper extremity transplantation in the short and long-term is now established,Citation1,3-7 and continuing to evolve. The most recent published report of the International Registry of Hand and Composite Tissue Transplantation (IRHCTT) in 2010 provided results of 49 hand and upper extremity transplantations in 33 patients worldwide, with greater than 90% allograft survival rate.Citation8 In just 3 years following that report, from 2010–2013, the number of has nearly doubled, totaling 89 upper extremity transplantations.Citation9 Improvement in disability scores has been achieved for transplants at the level of the wrist, forearm, and arm.Citation3-7 Strides toward inducing long-term allograft tolerance have shown great promise in both translational animal models and clinical trials.Citation10-12 For continued improvement, standardized protocols are required to facilitate the widespread use of this novel reconstructive modality.
Many aspects of upper extremity transplantation currently follow solid organ transplantation (SOT) protocols. As may be expected through experience with SOT, careful recipient selection is one of the most important elements for successful outcomes.Citation13,14 However, donor selection and procurement has not received the same attention as other areas regarding upper extremity transplantation. As of the last IRHCTT report, 16 of 33 recipients underwent bilateral upper extremity transplantation, which has significant implications for procurement logistics, especially in the context of multi-visceral organ donors and working with SOT procurement teams.Citation8 Herein, we aim to address aspects of donor selection specific to hand and upper extremity transplantation, and specifically describe the sequence of procurement. We complement this with an illustrative procurement procedure outline.
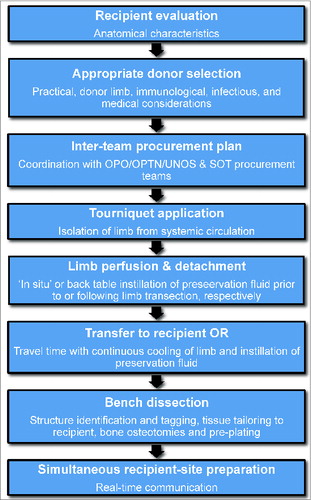
Planning of upper extremity allotransplantation, as with that of any vascularized composite allotransplantation (VCA), is recipient specific. The donor procurement plan requires careful consideration prior to actively wait-listing the patient. An overview of the donor procurement process is given in . In the United States, donor organ and tissue procurement is coordinated in each jurisdiction by the Organ Procurement Organization (OPO) overlooked by the United Network for Organ Sharing (UNOS).Citation15,16 In many cases, cadavers are utilized to rehearse team organization, sequence of events, and operative details; ideally, integrating the plan for donor harvest. Priority must be given to maintaining the viability of life-saving organs, namely thoracic and abdominal viscera. The technique used in unilateral and bilateral upper extremity transplantations is essentially identical, which has implications for procurement in the context of brain-dead heart-beating multi-visceral organ donors. The contribution and experience of the OPO is crucial to the success of the donor procurement process, including specialized donor family consent.Citation17 With still a very small number of currently approved hand and upper extremity allotransplantation centers in the United States, OPOs and SOT teams must be independently familiar with the logistical aspects of upper extremity procurement, as the combination of VCA and SOT teams for any given donor is unpredictable.
Donor Selection
Once a matching donor is identified by the OPO and specific consent has been obtained through a separate consenting process from any SOT donation, the hand transplant team is offered the opportunity to procure donor limbs for hand and upper extremity transplantation. This entails a very time sensitive process of decision making during which the VCA team must consider travel/ischemia time, donor limb characteristics, immunological and infectious disease barriers, and any other medical contraindications. Specific donor limb characteristics taken into consideration include physical/anatomical factors and quality ().
Figure 2. Chart outlining practical, donor limb specific, and immunological/medical considerations in proper donor selection.
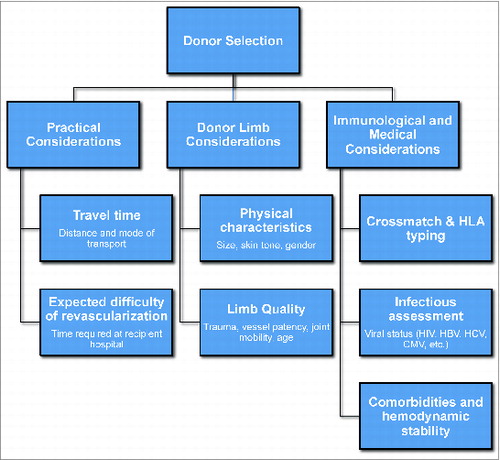
Practical considerations
In order to avoid prolonged ischemic times, greater distances between donor and recipient hospitals should be avoided. Geographical location of the donor center, mode of transportation, and expected difficulty revascularizing the donor extremity are important. Dedicated thought should be given to this prior to actively wait-listing the recipient for transplantation, and should follow Organ Procurement Transplantation Network (OPTN) guidelines.Citation18 The contribution of the OPO is vital to this process.Citation17 Although no current clinical studies exist with regards to maximal ischemic time, minimization is advocated.Citation19 Whereas grafts that do not include a large muscle mass (very distal forearm or wrist level hand transplants) might by fairly tolerant to ischemia this is particularly important in more proximal transplantations given the sensitivity of the muscle tissue to ischemia.Citation1 It is the preference of the senior authors to set the upper limit of expected cold ischemia time to 8–10 hours, which should be obtainable. Hautz and colleagues reported reperfusion within 4 hours for all transplants, including bilateral cases.Citation20 If the location of the donor will allow for ischemia time to remain under the suggested 8–10 hours, further analysis of the physical characteristics and quality of the donor upper extremities is indicated.
Donor limb considerations
The requirement to match physical characteristics of the transplanted organ to the recipient is unique to the field of VCA. In hand and upper extremity transplantation, one of the first considerations is closely matching donor-recipient limb size.Citation14 Further considerations include age, skin tone, and gender. The relative importance of these secondary characteristics is debatable. Although it is logical to avoid transplanting an older donor limb to a young recipient, it may not be necessary to prevent a young donor limb from being given to an older recipient. Skin tone matching is ideal, but slight to moderate mismatch should not be a hard contraindication. Gender mismatch is no longer considered a contraindication in many VCA centers, as size matching may be easier to achieve when both genders are included in the donor pool.Citation6,21,22 Overall, the above recipient-specific factors must be weighed against the availability of donors, as the more selective the hand transplantation team becomes, the less likely a donor match will ever be identified. These considerations should be discussed with the recipient in detail, as the patient may be able to guide the team with general preferences such as donor age, race, gender, and level skin tone similarity. It is also important that such individual recipient-specific matching criteria are clearly communicated with the OPO and added to the waitlist information.
Donor upper extremity quality must be evaluated once it is determined to be a suitable physical match for the recipient. Quality is affected by underlying co-morbidities, previous trauma and/or surgery to the limb, possible vascular injury secondary to invasive monitoring (e.g. arterial linesCitation6), circulating drugs and their effects (e.g., vasopressors), and the underlying mechanism leading to brain death (e.g. major trauma). In the United States, trauma is most common cause of brain death, thus, extremity injury must be excluded.Citation1 Patency of vessels can be confirmed with clinical inspection. Performance of computed tomographic angiography is typically not needed, and if desired must be discussed with SOT teams as contrast can potentially compromise renal function and thus complicate kidney donation. It is crucial to ensure full range of motion of all joints being transferred, as nerve regeneration will never be able to overcome stiff or arthritic joints.
Immunological and medical considerations
Upon deciding to proceed further with the matching process once donor limb characteristics are assessed, the next step is to perform a pre-transplant crossmatch. Donor lymphocytes are exposed to recipient blood to screen for anti-donor reactivity as well as any potential hyper reactivity due to pre-formed antibodies. A positive crossmatch precludes transplantation. The presence of high panel reactive antibodies (PRA), in particular when donor-specific, can be problematic and the corresponding HLA antigens are considered by many centers as “unacceptable antigens” that would preclude further evaluation of such a donor. There is no specific goal for HLA-matching in hand and upper extremity transplantation, as current immunotherapy regimens are able to overcome full mismatches, and there is no correlation between HLA-match and number of acute rejection episodes.Citation23
A thorough medical evaluation of the donor, including testing for viral infectious diseases, must then be undertaken. Most centers currently consider HIV, HBV, or HCV seropositivity an absolute contraindication for VCA. Cytomegalovirus (CMV) is one of the most important infectious considerations prior to proceeding with transplantation, as CMV positive recipients can reactivate with initiation of immunosuppression and CMV positive donors can infect naïve recipients. CMV negative donors are optimal in all scenarios, but with prevalence rates as high as 50–90%, might not be feasible. If high-risk pairings are selected (CMV positive donor to CMV negative recipient), familiarity with prophylaxis and treatment is paramount to prevention of complications and invasive disease,Citation24-26 though we currently consider this a relative contraindication in our own program. Further viral testing to be considered includes, Epstein-Barr virus (EBV), herpes simplex virus (HSV), and varicella-zoster virus (VZV).
In addition to immunological and infectious assessment of the donor, a detailed general medical history is undertaken. Points of emphasis are cancer history, connective tissue disease, end-organ disease, and current hemodynamic stability.
Donor Limb Procurement Team
The hand and upper extremity transplantation team is multi-disciplinary and utilizes the strengths of multiple surgical specialties. The foundation of the team should include hand surgeons and/or reconstructive microsurgeons, a transplant physician, and a transplant coordinator.Citation17 Once the core of the team is defined, additional personnel include transplant infectious disease physicians, psychiatrists, social workers, and occupational/physical therapists. Each team member must have a clearly defined role, and be prepared in the event that a donor becomes available. When a donor becomes available and the team decides to proceed with transplantation, a small group travels to the donor hospital for procurement, while the remaining team members prepare the recipient in concert. The composition and size of the procurement team will vary based on the number of upper extremities being retrieved. Ideally, at least 2 hand/reconstructive microsurgeons travel to the donor hospital for each limb that is being procured. Larger ORs are preferable, both for the procurement and ultimate transplantation, given the number of surgeons involved in both procedures. With the harvest team established, the next step is to discuss the practical aspects of procurement with the SOT teams.
Surgical Procurement
Inter-team procurement logistics
Donors in hand and upper extremity transplantation are commonly also multi-visceral organ donors.Citation6,7 The organ procurement logistics must be understood and agreed upon by all parties involved prior to initiation of the harvest. The OPO is responsible for coordinating inter-team dynamics. Thus, knowledge of the limb procurement process by both the OPO and the SOT teams is critical. This increases efficiency, provides less room for error, and decreases tension between teams. It is possible for donor limb procurement to occur prior to, simultaneously with, or immediately following solid organ harvest (). As mentioned earlier, priority is always given to maintaining the viability of life-saving organs. In the event that a donor becomes unstable and procurement of solid organ grafts such as the heart or liver needs to be expedited it goes without saying that the VCA donor procedure will be aborted.
Figure 3. Pathways for donor limb harvest. (A) Prior to solid organ procurement, (B) Post- solid organ procurement, and (C) Simultaneously with solid organ procurement.
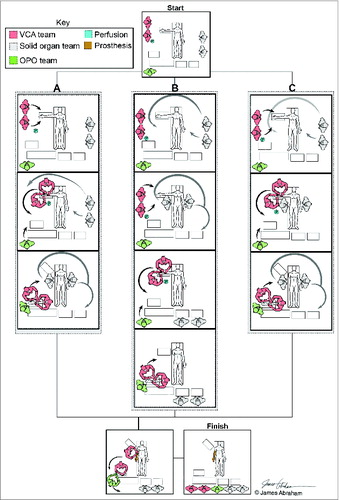
The most common method of limb procurement reported in the literature is prior to solid organ harvest, with rapid transection and back table perfusion.Citation7 Successful outcomes procuring upper extremities post-solid organ recovery have been reported, but are not widely performed given the concern for ischemia time.Citation6 The 3 possible timeframes for hand and upper extremity harvest in relation to solid organ procurement are detailed below and illustrated in .
Upper extremity harvest prior to solid organ ()
Tourniquet application ensures isolation of the limb vasculature from that of the donor. Rapid transection occurs at the desired level, and the donor limb(s) is perfused on back table with preservation solution. ‘In situ’ perfusion may occur given sufficient time and prior OPO and SOT agreement. This method is useful for bilateral limb procedures, whereby each upper extremity team can work simultaneously. Cavadas et al. reported recovery of both limbs within 45 minutes in 4 cases of bilateral upper extremity allotransplantation.Citation7
Upper extremity harvest post-solid prgan ()
Limb recovery post-solid organ procurement is uncommon, given considerations for the immediate need for preservation fluid instillation to avoid warm ischemia time. Hemodynamically unstable donors may require SOT teams to proceed first to limit injury to life-saving organs. Once the SOT team cross-clamps the aorta, the donor is converted to a non-heart-beating cadaveric donor. If time allows, the cardiothoracic team can isolate the limbs for instillation of preservation fluid by inserting cannulas in the proximal vessels (ie brachiocephalic or subclavian) prior to proceeding with solid organ procedures. If time does not allow for cannula insertion, perfusion of the limb with preservation fluid can occur ‘in situ’ after the SOT teams are finished. When extremity perfusion occurs after aortic cross-clamping, it is wise to externally cool the extremities prior to initiation of solid organ procurement.
Simultaneous upper extremity and solid organ harvest ()
During simultaneous procurement, the extremity harvest merges with that of the solid organs. Limb vascular isolation should occur prior to aortic cross-clamping by the SOT teams. In this scenario, availability of operating room space becomes a real concern. This may prove challenging in cases of bilateral limb procurements. If time constraints are in place, rapid transection occurs with back table perfusion.
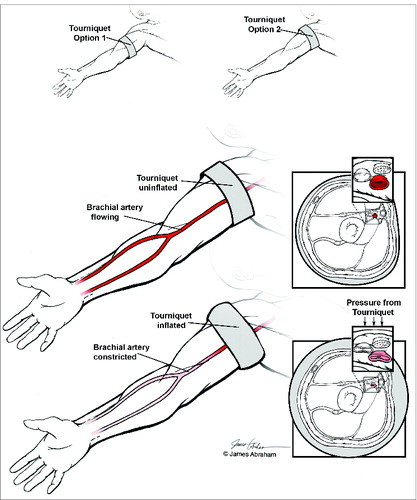
Tourniquet application
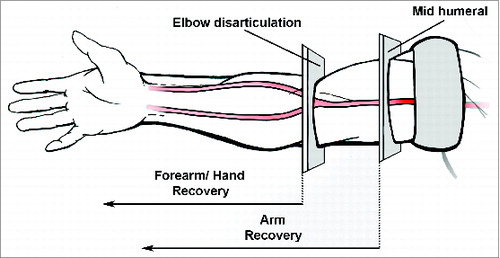
The procurement begins with tourniquet application. The tourniquet is placed proximal to the required level of the transplantation, allowing for excess soft tissues, bone, and adequate length of nerves and vascular structures once transection is completed (). The purpose of the tourniquet is to minimize blood loss and isolate the limb from the systemic circulation in the heart-beating donor, avoiding the risk of destabilization due to blood loss (). The removal of excess tissue from the procured limb occurs later, during the actual transplant, where it is discussed in real-time with the recipient-site team as it is being performed.Citation2 Esmarch exsanguination of the limb before tourniquet application is usually performed. For mid-forearm and more distal transplants (i.e. wrist), mid-humeral placement of the tourniquet is sufficient. For arm transplantations (i.e., above elbow), the tourniquet is applied as proximal as possible, within the axilla. More proximal transplantations are theoretically possible with occlusion of blood flow to the limb via access to the subclavian artery, though such transplantations remain experimental at present. Once the tourniquet is applied, the arm should remain cool. A barrier must be placed between the limb and ice to prevent cutaneous cold-induced injury. This may be achieved by placing ice covered in a towel below the sterile operative drapes.Citation1
Figure 4. Tourniquet application. (A) The tourniquet may be placed at mid-humeral (for elbow transection) or proximal arm (for mid-humeral transection) dependent on recipient anatomical requirements (B) The pressure of the tourniquet should be sufficient to isolate the limb segment from the systemic vasculature.
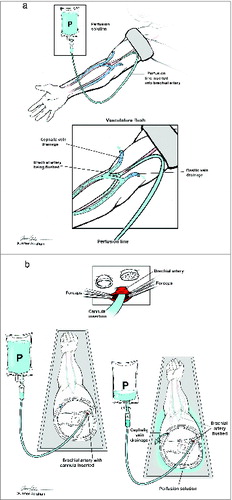
Instillation of preservation fluid
Perfusion of the donor limb with preservation fluid is commenced as soon as possible. The ideal preservation solution should protect against injurious effects ischemia, cooling on ice, and reperfusion. It is the preference of the senior authors to use 500–1000 mL of histidine-tryptophan-ketoglutarate (HTK) (Custadiol®) infused with 5000 units of unfractionated heparin, though use of alternative solutions such as University of Wisconsin (UW) solution and Belzer solution have been reported in the literature.Citation7,17.20 Ideally, this is infused ‘in situ’ after tourniquet application prior to transection, which is not always possible due to time constraints, necessitating rapid detachment with back table perfusion.
The superficial veins (basilic and cephalic) are carefully identified and reflected. Proximal and distal control of the brachial artery is obtained. A cannula is inserted into the brachial artery and secured, through which the preservation fluid is instilled (). The instillation continues until the venous efflux is clear. Observation of which veins are the dominant venous return should be noted. ‘In situ’ perfusion involves vessel identification through a circumferential cutaneous incision around the limb just distal to the tourniquet. The cannula is inserted through a brachial artery ‘fish-mouth’ arteriotomy (). The advantage of this method is the immediate instillation of preservation fluid. In the back table perfusion method, rapid transection of the donor limb occurs and the limb is transferred to the back table, where the instillation proceeds ().
Figure 5. Preservation fluid instillation. (A) ‘In situ’ instillation: While the limb remains attached an infusion catheter is inserted into the brachial artery via arteriotomy. (B) Back table perfusion: Following rapid transection, the donor limb is transferred to the back table where preservation fluid is instilled. Forceps are used to open the arterial lumen.
Detachment of the donor limb
The level of transection is dependent upon the recipient-specific level of the transplantation (). A conservative approach is taken with excess tissue, as described earlier. Dissection of neurovascular structures is performed to aid later identification. Once neurovascular structures are tagged, muscles are identified and divided, and the bone is osteotomized.Citation27 For mid-forearm or more distal transplantations, disarticulation at the level of the elbow is sufficient. For those occurring more proximally, transections are typically mid-humeral.Citation6 If a more proximal transection is required, isolation of the limb vasculature through the subclavian vessels is possible, but requires careful coordination with solid organ procurement. Following detachment, the tourniquet is left in place indefinitely until all organs have been recovered and the donor circulation has ceased.
Limb packaging and transportation
Following transfer to the back table, the limb is packaged and prepared for transport to the recipient center. It is wrapped in moist sterile gauze and placed in a sealed sterile bag. A second empty sterile bag is applied, which is finally placed in a third sterile bag filled with ice water as per standard SOT protocol (Policy 16, OPTN, effective 07/03/2014).Citation2,18,27 Cavadas and co-workers reported that they immersed their allografts in perfusion solution and transported these on ice.Citation7 Similar descriptions include covering the limb in moist gauze, which is placed in a sterile container of ice water at 4–6°C, with option for continuous instillation of preservation fluid during transport.Citation17
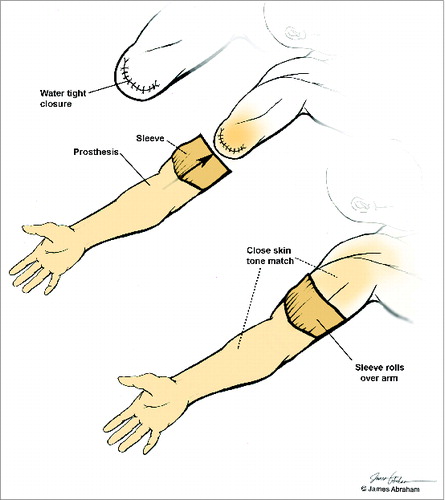
Donor prosthesis
Once actively wait-listing the patient, a custom-made cosmetic prosthesis is obtained based on recipient-specific physical parameters collected, i.e. size, skin tone etc. Thus, through close donor-recipient matching, the prosthesis is suited to the donor. The prosthesis should be taken to the donor center with the procurement team. Following donor limb and solid organ recovery, the blood vessels are tied and the tourniquet is removed. Skin flaps are utilized for stump closure (). The sleeve on the proximal segment of the prosthesis is rolled over the donor limb stump allowing for restoration of form. This also allows for donor integrity, family viewing, and the possibility of an open casket funeral.Citation17
Back Table Dissection
Following transfer to the recipient center, the limb is prepared for transplantation in concert with the recipient site. This should ideally occur in the recipient OR, allowing for real-time communication between all teams involved, minimizing ischemia time and producing an ideal anatomical match.Citation2 The donor limb should be continually cooled with ice covered in a towel under the operative draping, surrounded by sterile ice packs or with iced sponges.
Dissection of the donor limb is from proximal to distal. All structures are carefully identified and clearly tagged. The latter may be achieved using pieces of Esmarch bandage, labeled using a permanent marker and anchored to tissues via sutures. Tagging structures is essential, as identification becomes unnecessarily challenging later due to reperfusion, with blood and edema obscuring the field.Citation2 The donor soft tissue and bone is tailored to the lengths and contour of the recipient. Importantly, the superficial veins, arteries and nerves should be kept as long as possible until excess length is confirmed on the recipient table.
Cutaneous preparation
Incisions are marked with a sterile permanent marker. These should be made at 90° to the incisions used on the recipient such that the skin flaps interdigitate. This acts to prevent circumferential scarring with later contracture.Citation2 Excess skin can be removed in the future and prevents the need for future skin grafts.
Blood vessels
Careful dissection of the vascular anatomy is necessary to minimize damage to these structures. The absence of circulating blood in the vascular tree makes this process more challenging. It is essential to limit the division of perforators to cutaneous flaps to avoid devascularization and unexpected bleeding on reperfusion. Vessels are kept as long as possible until ultimate anastamosis, whereby they are shortened to reduce kinking.Citation27 Minimal adventitial stripping is performed and microclips are used for all small branches divided. Post reperfusion bleeding can be substantial from small vessel branches that were not recognized and divided or not appropriately controlled with ligation or clips.
Nerves
Nerves are kept as long as possible. Immediately prior to coaptation they are trimmed to allow the minimum length for tension-free repair, minimizing the distance recipient nerves must regenerate. Potential areas of nerve compression (carpal tunnel and cubital tunnel) may be decompressed/transposed as deemed beneficial.
Muscle
The muscles involved will depend on the level of transplantation. Tendons, myo-tendinous junctions, and/or muscles bellies may require dissection and attachment to the recipient limb. If possible, harvest of donor tensor fascia lata, Achilles tendon, or contralateral biceps tendon allows for reinforcement during inset and reconstruction.Citation27 For complete replacement of the recipient forearm musculature, the pronator/flexor and extensor origins can be elevated off the donor skeleton as a sleeve opened dorsally and suture anchored on top of the recipient musculature at the medial and later epicondyles. These require full re-innervation after recipient nerve transfer into the donor nerves.Citation28
Bone
Lastly, bone length is established prior to osteosynthesis and after careful discussion with recipient team, a ‘trimming’ osteotomy is made at the desired length with an oscillating saw. Limb length is tailored to “normal” for the patient's height in bilateral cases, or to the patient's contralateral limb if present. Measurements should be calculated directly from bony landmarks and verified on pre-operative radiographs of the donor limb and recipient stump. The use of Kirschner wires as fidelity points for measuring can aid in this process. In addition, pinning the distal radial-ulnar joint (DRUJ) in full supination allows adequate exposure to all structures and helps prevent rotational deformity of the ulna in relation to the recipient ulna.
Bones are pre-plated with pre-selected hardware. Several pilot holes and screws are placed to adapt the plate to the correct location, ensuring that the ‘trimming’ osteotomy can be performed at the correct location. In wrist and forearm level transplantations, the radius ‘trimming’ osteotomy is performed and the radius is pre-plated. Once this is performed the 2 separate ‘work stations’ (bench and recipient-site) are condensed to a single workstation. Once the radius osteosynthesis is complete, an oblique osteotomy is made on the ulna to maximize bone-bone contact and provide a small amount of “wiggle room” to cheat the ulna in position or length.Citation29 It is the preference of the authors to use 3.5 mm locking compression plates (LCP) (Synthes, Obernorf, Switzerland) to achieve rigid fixation. In addition, the authors have helped develop a surgical technique utilizing an ulnar shortening osteotomy (USO) plate for rigid stabilization and compression of the ulna.Citation29 This enables rapid advancement of load bearing therapy in the mid- and proximal forearm regions. In the distal forearm region, volar locking extended distal radius and distal ulna plates are preferred. With transplants distal to the elbow, the radius and ulna can be pre-plated on the ‘bench’. For supracondylar transplants, a single 4.5 mm LCP placed through an anterolateral approach can be used.Citation27 Successful humeral osteosynthesis in the context of gross donor-recipient transverse humerus size mismatch has also been achieved in one patient using a K-wire bundle.Citation6
Future Directions
There is an increasing need for functional upper extremity reconstructive solutions. As hand and upper extremity allotransplantation increases in frequency, a standardized limb procurement protocol is required which all parties involved must understand and agree to. A multi-disciplinary team approach is essential, and clear communication is required at all times. Cadaveric recipient-specific rehearsal can be utilized to ensure all aspects of the procurement and transplantation are well understood by the limb procurement team. Efficiency in the procurement process is of paramount importance in minimizing cold ischemic time.
Certain practices within the donor procurement process remain unexplored. The effect of cold ischemic time on immunological and functional outcomes is largely unknown. As surgical procedures expand to include an increasing number of proximal upper extremity transplantations, the effect of the ischemic time becomes even more important given the added muscle bulk (metabolic demand) and skin surface area (antigen load).Citation30-32 Similarly, the optimal preservation fluid for VCA requires further research.Citation33,34 Thoroughly defining the limits of ischemia time and optimizing preservation fluid could expand the donor pool to even include cadaveric (non-heart-beating) donors. Multiple VCA recipients have experienced poor outcomes, possibly related to high antigen load, mass ischemia, and undefined critical care needs.Citation35 As VCA continues to expand, newer immunotherapies are needed to favor the risk-benefit ratio. Novel immunomodulation protocols, such as infusion of donor derived bone marrow cells as used by the senior authors, further impact procurement logistics and need to be carefully considered.Citation12,36,37
Overall, the field of VCA is rapidly evolving, requiring further standardization, guidelines, more consistent reporting, and is ripe with opportunity to advance current practice and knowledge.
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- Schuind F, Abramowicz D, Schneeberger S. Hand transplantation: the state-of-the-art. J Hand Surg Eur 2007; 32(1):2-17; PMID:17084950; http://dx.doi.org/10.1016/j.jhsb.2006.09.008
- Hartzell TL, Benhaim P, Imbriglia JE. Surgical and technical aspects of hand transplantation: is it just another replant? Hand Clin 2011; 27(4):521-30; PMID:22051392; http://dx.doi.org/10.1016/j.hcl.2011.08.001
- Breidenbach WC, Gonzales NR, Kaufman CL, Klapheke M, Tobin GR, Gorantla VS. Outcomes of the first 2 American hand transplants at 8 and 6 years post transplant. J Hand Surg Am 2008; 33:1039-47; PMID:18762094; http://dx.doi.org/10.1016/j.jhsa.2008.02.015
- Petruzzo P, Badet L, Gazarian A, Lanzetta M, Parmentier H, Kanitakis J, Sirigu A, Martin X, Dubernard JM. Bilateral hand transplantation: six years after the first case. Am J Transplant 2006; 6(7):1818-724; PMID:16827876; http://dx.doi.org/10.1111/j.1600-6143.2006.01369.x
- Brandacher G, Ninkovic M, Piza-Katzer H, Gabl M, Rieger M, Schocke M, Schocke M, Egger K, Loescher W, Zelger B, et al. The Innsbruck hand transplant program: update at 8 years after the first transplant. Transplant Proc 2009; 41(2):491-4; PMID:19328910; http://dx.doi.org/10.1016/j.transproceed.2009.01.013
- Jablecki J. World experience after more than a decade of clinical hand transplantation: update on the polish program. Hand Clin 2011; 27:433-42; PMID:22051385; http://dx.doi.org/10.1016/j.hcl.2011.08.003
- Cavadas PC, Landin L, Thione A, Rodriguez-Pérez JC, Garcia-Bello MA, Ibañez J, Vera-Sempere F, Garcia-Cosmes P, Alfaro L, Rodrigo JD, et al. The Spanish experience with hand, forearm, and arm transplantation. Hand Clin 2011; 27(4):443-53; PMID:22051386; http://dx.doi.org/10.1016/j.hcl.2011.08.002
- Petruzzo P, Lanzetta M, Dubernard JM, Landin L, Cavadas P, Margreiter R, Schneeberger S, Breidenbach W, Kaufman C, Jablecki J, et al. The international registry on hand and composite tissue transplantation. Transplantation 2010; 90(12):1590-4; PMID:21052038; http://dx.doi.org/10.1097/TP.0b013e3181ff1472
- Siemionow M, Gharb BB, Rampazzo A. Succeses and lessons learned after more than a decade of upper extremity and face transplantation. Curr Opin Organ Transplant 2013; 18(6): 633-9; PMID:24126806; http://dx.doi.org/10.1097/MOT.0000000000000021
- Ibrahim Z, Cooney DS, Shores JT, Sacks JM, Wimmers EG, Bonawitz SC, Gordon C, Ruben D, Schneeberger S, Lee WP, et al. A modified heterotopic swine hind limb transplant model for translational vascularized compositeallotransplantation (VCA) research. J Vis Exp 2013; 14(80); PMID:24145603
- Hettiaratchy S, Melendy E, Randolph MA, Coburn RC, Neville DM, Sachs DH, Huang CA, Lee WP. Tolerance to composite tissue allografts across major histocompatibility barrier in miniature swine. Transplantation 2004; 77(4): 514-21; PMID:15084927; http://dx.doi.org/10.1097/01.TP.0000113806.52063.42
- Schneeberger S, Gorantla VS, Brandacher G, Zeevi A, Demetris AJ, Lunz JG, Metes DM, Donnenberg AD, Shores JT, Dimartini AF, et al. Upper-extremity transplantation using a cell-based protocol to minimize immunosuppression. Ann Surg 2013 257(2): 345-51; PMID:23001085; http://dx.doi.org/10.1097/SLA.0b013e31826d90bb
- Dobbels F, Vanhaecke J, Dupont L, Nevens F, Verleden G, Pirenne J, De Geest S. Pretransplant predictors of posttransplant adherence and clinical outcome: an evidence base for pretransplant psychosocial screening. Transplantation 2009; 87(87), 1497-504; PMID:19461486; http://dx.doi.org/10.1097/TP.0b013e3181a440ae
- Shores, J. Recipient screening and selection: who is the right candidate for hand transplantation? Hand Clin 2011; 27(4): 539-43; PMID:22051394; http://dx.doi.org/10.1016/j.hcl.2011.07.009
- UNOS governance structure can be found at http://www.unos.org/about/index.php?topic=governance. Accessed on September 15, 2014.
- McDiarmid SV, Pruett TL, Graham WK. The oveversight of solid organ transplantation in the United States. Am J Transplant 2008; 8(4): 739-44; PMID:18318780; http://dx.doi.org/10.1111/j.1600-6143.2007.02147.x
- Banegas RN, Moreno R, Duggal A, Breidenbach WC 3rd. Surgical aspects of donor hand recovery for transplantation. J Reconstr Microsurg 2012 Jan; 28(1):21-6; PMID:21861253
- UNOS governance structure can be found at http://www.unos.org/about/index.php?topic=governance. Accessed on September 15, 2014.
- Landin L, Cavadas PC, Garcia-Cosmes P, Thione A, Vera-Sempere F. Perioperative ischemic injury and fibrotic degeneration of muscle in a forearm allograft: functional follow-up at 32 months post transplantation. Ann Plast Surg 2011; 66(2): 202-09; PMID:21200306; http://dx.doi.org/10.1097/SAP.0b013e318206a365
- Hautz T, Engelhardt TO, Weissenbacher A, Kumnig M, Zelger B, Rieger M, Rumpold G, Pierer G, Ninkovic M, Gabl M, et al. World experience after more than a decade of clinical hand transplantation: update on the Innsbruck program. Hand Clin 2011; 27(4): 423-31; PMID:22051384; http://dx.doi.org/10.1016/j.hcl.2011.07.004
- Cavadas PC, Thione A, Carballeira A, Blanes M. Bilateral transfemoral lower extremity transplantation: result at 1 year. Am J Transplant 2013; 13:1343-9; PMID:23433015; http://dx.doi.org/10.1111/ajt.12178
- Gordon CR, Swanson EW, Susarla SM, Coon D, Rada MA, Santiago GF, Shores JT, Bonawitz SC, Fishman EK, Murphy R, et al. Overcoming cross-gender differences and challenges in Le Fort-based craniomaxillofacial transplantation with enhanced computer assisted technology. Ann Plast Surg 2013; 71(4): 421-28; PMID:24025655
- Ashvetiya T, Mundinger GS, Kukuruga D, Bojovic B, Christy MR, Dorafshar AH, Rodriguez ED. Donor-recipient human leukocyte antigen matching practices in vascularized composite allotransplantation: a survey of major transplantation centers. Plast Reconstr Surg 2014; 134(1): 121-9; PMID:25028821; http://dx.doi.org/10.1097/PRS.0000000000000278
- Kotton CN, Kumar D, Caliendo AM, Asberg A, Chou S, Danzinger-Isakov L, et al. Updated international consensus guidelines on the management of cytomegalovirus in solid organ transplantation. Transplantation 2013; 96(4): 333-60; PMID:23896556; http://dx.doi.org/10.1097/TP.0b013e31829df29d
- Broyles, JM, Alrakan M, Ensor CR, Khalifian S, Kotton CN, Avery RK, Brandacher G, Lee WP, Gordon CR. Characterization, prophylaxis, and treatment of infectious complications in craniomaxillofacial and upper extremity allotransplantation: a multicenter perspective. Plast Reconstr Surg 2014; 133(4): 543-51; PMID:24675206; http://dx.doi.org/10.1097/PRS.0000000000000015
- Gordon CR, Avery RK, Abouhassan W, Siemionow M. Cytomegalovirus and other infectious issues related to face transplantation: specific considerations, lessons learned, and future recommendations. Plast Reconstr Surg 2011; 127(4): 1515-23; PMID:21460660; http://dx.doi.org/10.1097/PRS.0b013e318208d03c
- Shores JT, Higgins JP, Lee WP. Above-elbow (supracondylar) arm transplantation: clinical considerations and surgical technique. Tech Hand Up Extrem Surg 2013; 17(4): 221-7; PMID:24275765; http://dx.doi.org/10.1097/BTH.0000000000000026
- Haddock NT, Chang B, Bozentka DJ, Steinberg DR, Levin LS. Technical implications in proximal forearm transplantation. Tech Hand Up Extrem Surg 2013; 17(4): 228-31; PMID:24310233; http://dx.doi.org/10.1097/BTH.0000000000000025
- Higgins JP, Shores JT, Katz RD, Lee WP, Wolock BS. Forearm transplantation osteosynthesis using modified ulnar shortening osteotomy technique. J Hand Surg Am 2014; 39(1):134-42; PMID:24369942; http://dx.doi.org/10.1016/j.jhsa.2013.10.005
- Pradka SP, Ong YS, Zhang Y, Davis SJ, Baccarani A, Messmer C, Fields TA, Erdmann D, Klitzman B, Levin LS. Increased signs of acute rejection with ischemic time in a rat musculocutaneous allotransplant model. Transplant Proc 2009; 41(2): 531-6; PMID:19328919; http://dx.doi.org/10.1016/j.transproceed.2009.01.021
- Siemionow M, Arslan E. Ischemiareperfusion injury: a review in relation to free tissue transfers. Microsrugery 2004; 24(6): 468-75; PMID:15378577; http://dx.doi.org/10.1002/micr.20060
- Land WG. The role of postischemic reperfusion injury and other nonantigen-dependent inflammatory pathways in transplantation. Transplantation 2005; 79(5): 505-14; PMID:15753838; http://dx.doi.org/10.1097/01.TP.0000153160.82975.86
- O’Callaghan JM, Knight SR, Morgan RD, Morris PJ. Preservation solutions for static cold storage of kidney allografts: a systematic review and meta-analysis. Am J Transplant 2012; 12(4): 896-906; PMID:22221739; http://dx.doi.org/10.1111/j.1600-6143.2011.03908.x
- Liu Q, Li Q, Zheng S, Zheng D. Preservation of canine composite facial flaps using UW solution. Arch Facial Plast Surg 2010; 12(4): 263-8; PMID:20644232; http://dx.doi.org/10.1001/archfacial.2010.47
- Swanson EW, Brandacher G, Gordon CR. Discussion of lessons learned from the first quadruple extremity transplantation in the world: comments and concerns regarding quadruple extremity allotransplantation. Ann Plast Surg 2014; 73(3): 343-5; PMID:25003409; http://dx.doi.org/10.1097/SAP.0000000000000281
- Gorantla VS, Schneeberger S, Moore LR, Donnenberg VS, Zimmerlin L, Lee WP, Donnenberg AD. Development and validation of procedure to isolate viable bone marrow cells from the vertebrae of cadaveric organ donors for composite organ grafting. Cytotherapy 2012; 14(1): 104-13; PMID:21905958; http://dx.doi.org/10.3109/14653249.2011.605350
- Donnenberg AD, Gorantla VS, Schneeberger S, Moore LR, Brandacher G, Stanczak HM, Koch EK, Lee WA. Clinical implementation of a procedure to prepare bone marrow cells from cadaveric vertebral bodies. Regen Med 2011; 6(6): 701-6; PMID:22050522; http://dx.doi.org/10.2217/rme.11.89