Figures & data
Figure 1. (A) Anatomical landmarks used for bra fitting. (B) Anatomical fiducial points used in the clinical bra measurements. MPP: most projecting point; TP: transition point; MC: mid-clavicle; SN: sternal notch; MP: medial point; M: midline; IMF: inframammary fold; LP: lateral point.
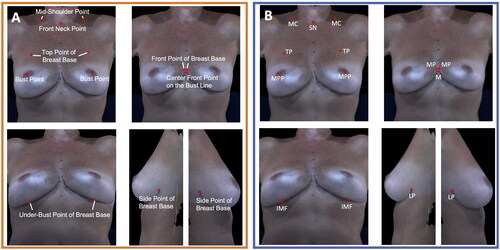
Figure 2. The front neck point to bust point measurement (sternal notch to most projecting point) significantly decreased in the reconstructed breast after unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of the front neck point to bust point measurement at baseline and post-reconstruction (median and interquartile range). (B) The front neck point to bust point measurement on an exemplar patient at baseline. (C) The front neck point to bust point measurement on the same patient post-reconstruction.
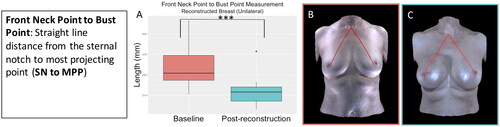
Figure 3. The front point of breast base to bust point measurement (medial point to most projecting point) significantly decreased in the reconstructed breast after unilateral implant-based reconstruction (p = 0.02). (A) Boxplot of the front point of breast base to bust point measurement at baseline and post-reconstruction (median and interquartile range). (B) The front point of breast base to bust point measurement on an exemplar patient at baseline. (C) The front point of breast base to bust point measurement on the same patient post-reconstruction.
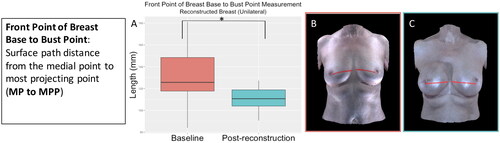
Figure 4. The centre front point on the bust line to bust point measurement (midline to most projecting point) significantly decreased in the reconstructed breast after unilateral implant-based reconstruction (p = 0.03). (A) Boxplot of the centre front point on the bust line to bust point measurement at baseline and post-reconstruction (median and interquartile range). (B) The centre front point on the bust line to bust point measurement on an exemplar patient at baseline. (C) The centre front point on the bust line to bust point measurement on the same patient post-reconstruction.
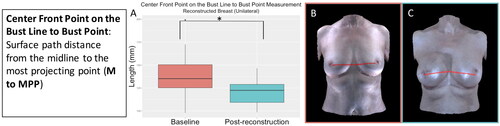
Figure 5. The mid-shoulder point to top point of breast base measurement (mid-clavicle to transition point) significantly decreased in the reconstructed breast after unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of the mid-shoulder point to top point of breast base measurement at baseline and post-reconstruction (median and interquartile range). (B) The mid-shoulder point to top point of breast base measurement on an exemplar patient at baseline. (C) The mid-shoulder point to top point of breast base measurement on the same patient post-reconstruction.
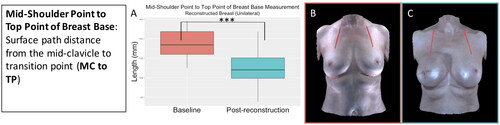
Figure 6. The front neck point to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The front neck point to bust point measurement on an exemplar patient. (C) The front neck point to bust point measurement on the same patient post-reconstruction.
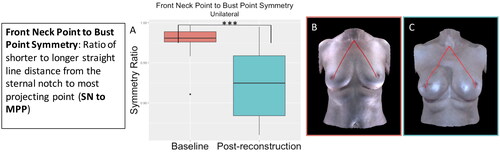
Figure 7. The front point of breast base to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The front point of breast base to bust point measurement on an exemplar patient. (C) The front point of breast base to bust point measurement on the same patient post-reconstruction.
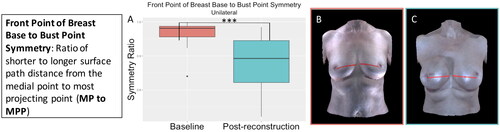
Figure 8. The side point of breast base to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The side point of breast base to bust point measurement on an exemplar patient. (C) The side point of breast base to bust point measurement on the same patient post-reconstruction.
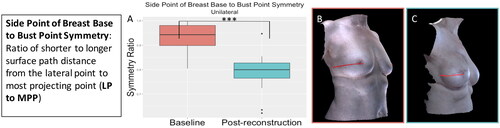
Figure 9. The centre front point on the bust line to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p = 0.01). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The centre front point on the bust line to bust point measurement on an exemplar patient. (C) The centre front point on the bust line to bust point measurement on the same patient post-reconstruction.
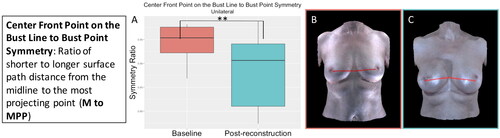
Figure 10. The mid-shoulder point to top point of breast base symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p = 0.002). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The mid-shoulder point to top point of breast base measurement on an exemplar patient. (C) The mid-shoulder point to top point of breast base measurement on the same patient post-reconstruction.
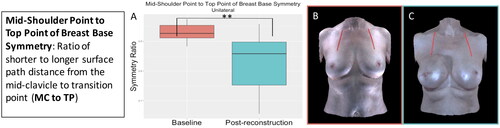
Figure 11. The front neck point to bust point measurement (sternal notch to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly decreased in the reconstructed breast after implant-based reconstruction (right breast: p < 0.001, left breast: p < 0.001). (A) Boxplot (median and interquartile range) of the front neck point to bust point measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The front neck point to bust point measurement on an exemplar patient at baseline. (C) The front neck point to bust point measurement on the same patient post-reconstruction.
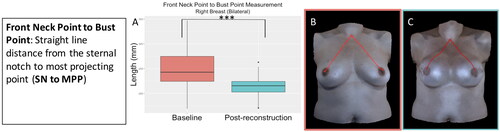
Figure 12. The bust point distance measurement (most projecting point to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly decreased after implant-based reconstruction (p = 0.003). (A) Boxplot of the bust point distance measurement at baseline and post-reconstruction (median and interquartile range). (B) The bust point distance measurement on an exemplar patient at baseline. (C) The bust point distance measurement on the same patient post-reconstruction.
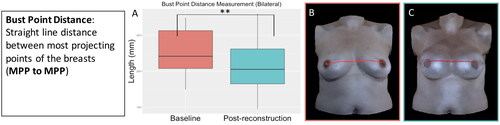
Figure 13. The front point of breast base to bust point measurement (medial point to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly decreased after implant-based reconstruction (right breast: p < 0.001, left breast: p < 0.001). (A) Boxplot (median and interquartile range) of the front point of breast base to bust point measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The front point of breast base to bust point measurement on an exemplar patient at baseline. (C) The front point of breast base to bust point measurement on the same patient post-reconstruction.
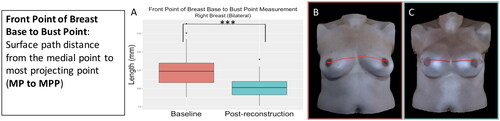
Figure 14. The under-bust point of breast base to bust point measurement (inframammary fold to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly increased after implant-based reconstruction (right breast: p = 0.03, left breast: p = 0.005). (A) Boxplot (median and interquartile range) of the under-bust point of breast base to bust point measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The under-bust point of breast base to bust point measurement on an exemplar patient at baseline. (C) The under-bust point of breast base to bust point measurement on the same patient post-reconstruction.
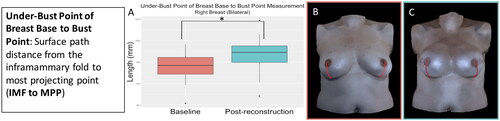
Figure 15. The centre front point on the bust line to bust point measurement (midline to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly decreased after implant-based reconstruction (right breast: p = 0.002, left breast: p = 0.003). (A) Boxplot (median and interquartile range) of the centre front point on the bust line to bust point measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The centre front point on the bust line to bust point measurement on an exemplar patient at baseline. (C) The centre front point on the bust line to bust point measurement on the same patient post-reconstruction.
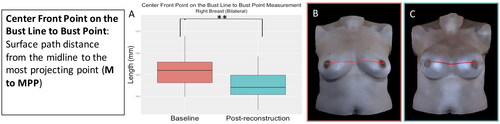
Figure 16. The mid-shoulder point to top point of breast base measurement (mid-clavicle to transition point) for the participants who underwent bilateral implant-based reconstruction significantly decreased after implant-based reconstruction (right breast: p < 0.001, left breast: p < 0.001). (A) Boxplot (median and interquartile range) of the mid-shoulder point to top point of breast base measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The mid-shoulder point to top point of breast base measurement on an exemplar patient at baseline. (C) The mid-shoulder point to top point of breast base measurement on the same patient post-reconstruction.
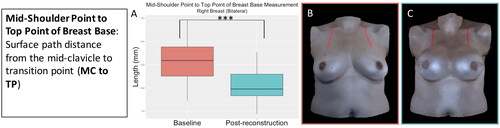
Figure 17. The front point of breast base to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent bilateral implant-based reconstruction (p = 0.01). (A) Boxplot (median and interquartile range) of symmetry at baseline and post-reconstruction. (B) The front point of breast base to bust point measurement on an exemplar patient. (C) The front point of breast base to bust point measurement on the same patient post-reconstruction.
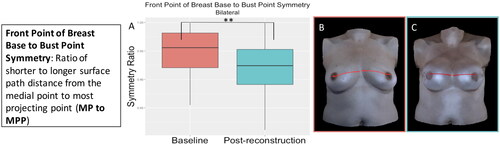
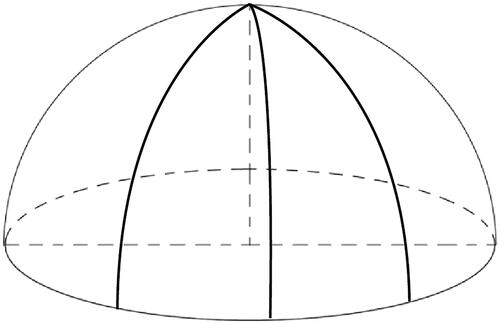
Figure 18. The semi-spherical shape of a bra cup for an implant-based reconstructed breast. The darts or the seams of the bra cup should be evenly distributed so that it will fit the semi-spherical shape of the implant-based reconstructed breast.
Supplemental Material
Download Zip (11 MB)Data availability statement
The data that support the findings of this study are available on request from the corresponding author, MKM. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
