Figures & data
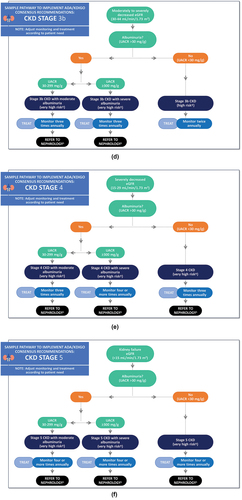
Figure 1. Sample CKD clinical care pathways for people with T2D based on UACR and eGFR. These are examples of pathways for implementation of the KDIGO heat map that is included in the ADA-KDIGO consensus report [Citation15]. It is not intended to prescribe an exclusive course of management. Clinicians should consider the individual needs of their patients. Monitoring may include performing an eGFR, UACR, and/or additional tests according to patient needs (e.g. if they have other comorbidities) and/or monitoring for possible drug side effects (e.g. hyperkalemia should be monitored/managed in patients taking a RASi or ns-MRA). *Consider risk factors for CKD such as advancing age (especially >65 years), genetic factors, family history of T2D, family history of DKD (including age at diabetes onset between 5 and 15 years), family history of CKD, metabolic syndrome, obesity, insulin resistance, smoking, high blood pressure, racial and ethnic minority group, and use of nephrotoxic agents. †Risk of CKD progression. Patients are considered low risk if they have an eGFR ≥60 mL/min/1.73 m2 and a UACR <30 mg/g and have no CKD/no other markers of kidney disease (e.g. hematuria, polycystic kidney disease, renovascular kidney disease, electrolyte abnormality etc.). ‡Author perspective: In primary care, patients with stage 1 or stage 2 CKD are typically treated with RASis (first-line) followed by SGLT2 inhibitors. The individual patient should be considered when choosing/initiating treatment. §Author perspective: Other reasons to refer to nephrology at all CKD stages include conditions such as gross hematuria or persistent microscopic hematuria, massive proteinuria, rapidly progressive decline in eGFR, and uncontrolled hypertension. ADA = American Diabetes Association; CKD = chronic kidney disease; DKD = diabetic kidney disease; eGFR = estimated glomerular filtration rate; KDIGO = Kidney Disease Improving Global Outcomes; ns-MRA = nonsteroidal mineralocorticoid receptor antagonist; RASi = renin angiotensin system inhibitor; SGLT2 = sodium glucose cotransporter-2; T2D = type 2 diabetes; UACR = urine albumin-to-creatinine ratio.
![Figure 1. Sample CKD clinical care pathways for people with T2D based on UACR and eGFR. These are examples of pathways for implementation of the KDIGO heat map that is included in the ADA-KDIGO consensus report [Citation15]. It is not intended to prescribe an exclusive course of management. Clinicians should consider the individual needs of their patients. Monitoring may include performing an eGFR, UACR, and/or additional tests according to patient needs (e.g. if they have other comorbidities) and/or monitoring for possible drug side effects (e.g. hyperkalemia should be monitored/managed in patients taking a RASi or ns-MRA). *Consider risk factors for CKD such as advancing age (especially >65 years), genetic factors, family history of T2D, family history of DKD (including age at diabetes onset between 5 and 15 years), family history of CKD, metabolic syndrome, obesity, insulin resistance, smoking, high blood pressure, racial and ethnic minority group, and use of nephrotoxic agents. †Risk of CKD progression. Patients are considered low risk if they have an eGFR ≥60 mL/min/1.73 m2 and a UACR <30 mg/g and have no CKD/no other markers of kidney disease (e.g. hematuria, polycystic kidney disease, renovascular kidney disease, electrolyte abnormality etc.). ‡Author perspective: In primary care, patients with stage 1 or stage 2 CKD are typically treated with RASis (first-line) followed by SGLT2 inhibitors. The individual patient should be considered when choosing/initiating treatment. §Author perspective: Other reasons to refer to nephrology at all CKD stages include conditions such as gross hematuria or persistent microscopic hematuria, massive proteinuria, rapidly progressive decline in eGFR, and uncontrolled hypertension. ADA = American Diabetes Association; CKD = chronic kidney disease; DKD = diabetic kidney disease; eGFR = estimated glomerular filtration rate; KDIGO = Kidney Disease Improving Global Outcomes; ns-MRA = nonsteroidal mineralocorticoid receptor antagonist; RASi = renin angiotensin system inhibitor; SGLT2 = sodium glucose cotransporter-2; T2D = type 2 diabetes; UACR = urine albumin-to-creatinine ratio.](/cms/asset/1b388da3-9e62-4a33-9387-0230c0d8585d/ipgm_a_2350924_f0001a_oc.jpg)
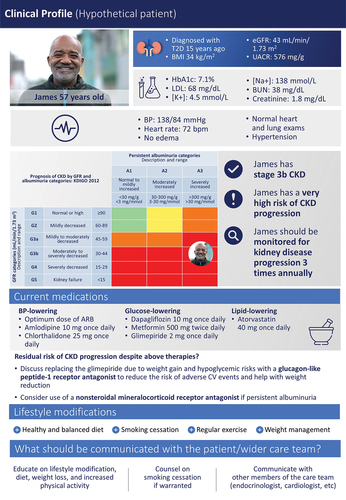
Figure 2. Hypothetical patient profile of an adult patient with CKD associated with T2D. The hypothetical patient profile presented here is fictional (not a real patient case). The content in this figure was provided by the authors and represents the opinions of the authors. The profile is intended to represent a clinical profile of an adult patient with CKD associated with T2D. ARB = angiotensin receptor blocker; BMI = BMI + Body Mass Index; BP = blood pressure; BUN = blood urea nitrogen; CKD = chronic kidney disease; CV = cardiovascular; eGFR = estimated glomerular filtration rate; HbA1C = hemoglobin A1c; K+ = potassium; KDIGO = Kidney Disease Improving Global Outcomes; LDL = low-density lipoprotein; Na+ = sodium; T2D = type 2 diabetes; UACR = urine albumin-to-creatinine ratio.