Figures & data
Figure 1. Kidney with normal function and normal glomeruli, and examples of renal glomerular function impairment caused by fewer pores and shrunken pores.
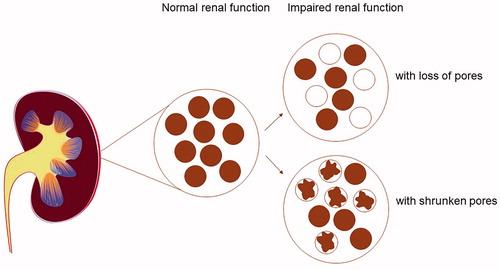
Figure 2. Flowchart showing the inclusion of study participants. All incident acute myocardial infarction (MI) from individuals in Norrbotten and Västerbotten counties of northern Sweden have been recorded since 1985 under the WHO's MONICA (Multinational Monitoring of Trends and Determinants in Cardiovascular Disease) project [Citation15]. Symptoms, biomarkers, and electrocardiogram (ECG) recordings were used for the diagnosis of MI. ECGs were evaluated according to the Minnesota code [Citation17]. The individuals with MI were cross-checked if they had participated in population-based risk factor surveys either as part of the Västerbotten Intervention Program (VIP), the MONICA project, or the Mammary Screening Program (MSP) within the Northern Sweden Health and Disease Study (NSHDS). At the MONICA Secretariat in Luleå and Umeå, research nurses validated MI cases that had participated. Two referent individuals with no previous MI were matched to every case based on sex, age (± 2 years), time of health examination and blood sampling, as well as geographical location and sub study.
![Figure 2. Flowchart showing the inclusion of study participants. All incident acute myocardial infarction (MI) from individuals in Norrbotten and Västerbotten counties of northern Sweden have been recorded since 1985 under the WHO's MONICA (Multinational Monitoring of Trends and Determinants in Cardiovascular Disease) project [Citation15]. Symptoms, biomarkers, and electrocardiogram (ECG) recordings were used for the diagnosis of MI. ECGs were evaluated according to the Minnesota code [Citation17]. The individuals with MI were cross-checked if they had participated in population-based risk factor surveys either as part of the Västerbotten Intervention Program (VIP), the MONICA project, or the Mammary Screening Program (MSP) within the Northern Sweden Health and Disease Study (NSHDS). At the MONICA Secretariat in Luleå and Umeå, research nurses validated MI cases that had participated. Two referent individuals with no previous MI were matched to every case based on sex, age (± 2 years), time of health examination and blood sampling, as well as geographical location and sub study.](/cms/asset/fb998683-931b-43cb-8af3-5aff5ecfad14/iclb_a_1941235_f0002_b.jpg)
Table 1. Baseline characteristics of the study population.
Figure 3. Univariable odds ratios with 95% confidence intervals for the risk of a first-ever MI in relation to glomerular function for men (▲) and women (■) separately. Risk through quartiles for (a) eGFRcreatinine, (b) eGFRcystatin C, and (c) the eGFRcreatinine/eGFRcystatin C ratio. p-Values ≤.05 are highlighted with *.
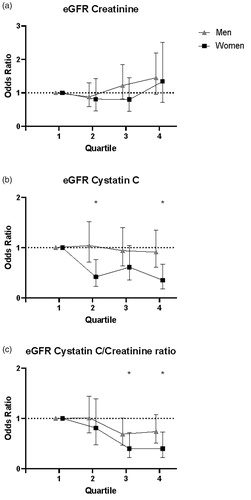
Table 2. Odds ratios (95% confidence intervals) for quartiles of glomerular function and risk of future MI.
Table 3. Univariable and multivariable odds ratios (95% confidence intervals) for z-scores of glomerular function and risk of future MI.
Supplemental Material
Download PDF (67.2 KB)Data availability statement
Aggregate data are included in the manuscript and its Supporting Information files. Individual data is not publicly available, as it contains potentially identifying patient information. Data are available upon request from the Northern Sweden Health and Disease Study Biobank. To request data, interested researchers must complete a formal application (available at https://www.umu.se/en/biobankresearch-unit/research/access-to-samples-anddata/access-to-nsdd/) and submit it to The Biobank Research Unit at Umeå University (contact via [email protected]).
