Figures & data
Table 1. Grading of histopathological characteristics.
Figure 1. Flow-chart of patients with inflammatory bowel diseases (IBD) with at least two liver biopsies prior to, at time of, or after cessation of thioguanine (TG) treatment.
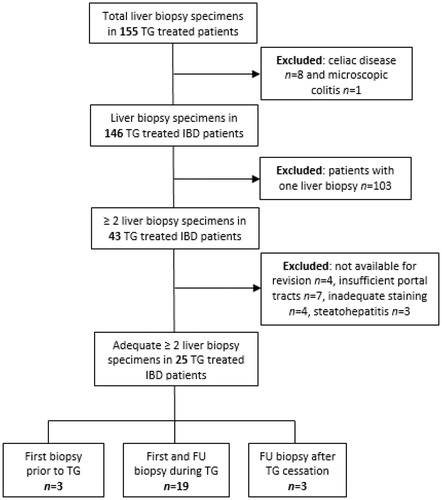
Table 2. Patient and disease characteristics.
Figure 2. Histopathological findings as observed in sequential liver biopsies obtained during thioguanine treatment. Histopathological abnormalities were graded from 0 to 3 according to the characteristics depicted in . The first and second bars represent the observed histopathological abnormalities in the first and second biopsy, respectively. No statistical significant differences between the first and second biopsy specimens were found although a trend towards statistical significance was observed for phlebosclerosis.
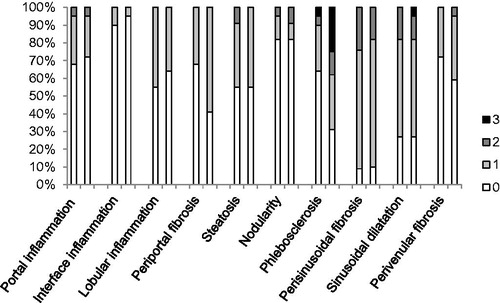
Figure 3. Microscopic examination of a liver biopsy with hepatic sinusoidal dilatation. Histopathology of a liver biopsy with hepatic sinusoidal dilatation characterized by widening of hepatic sinusoids in a patient with inflammatory bowel disease during thioguanine treatment (Hematoxylin-Eosin stained).
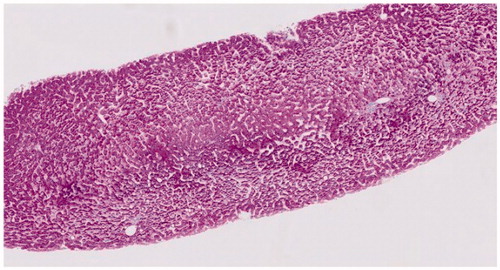
Figure 4. Microscopic examination of a liver biopsy with phlebosclerosis. Histopathology of a liver biopsy with phlebosclerosis characterized by sclerosis of the portal tract with diminished caliber of the portal vein caliber and extraportal shunt vessels in a patient with inflammatory bowel disease treated with thioguanine (Hematoxylin-Eosin stained).
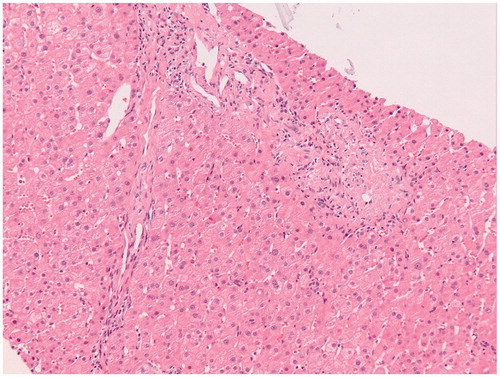
Figure 5. Microscopic examination of a liver biopsy with nodular regenerative hyperplasia (NRH). Histopathology of a liver biopsy with NRH characterized by nodules of hypertrophic hepatocytes surrounded by a rim of atrophic liver plates with compression of sinusoids in a patient with inflammatory bowel disease treated with thioguanine without signs of (non-cirrhotic) portal hypertension (Hematoxylin-Eosin stained).
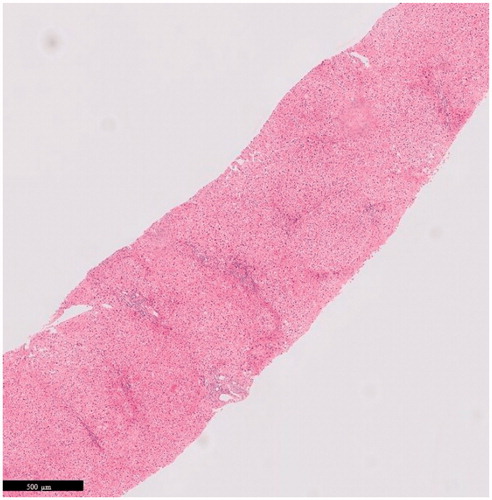
Table 3. Histopathological irregularities of the liver and their progression during time of TG treated IBD patients (n = 22).
Table 5. Histopathological and clinical alterations in 3 patients who ceased thioguanine due to hepatotoxicity.
Table 4. Laboratory findings at time of first and second liver biopsy.
