Figures & data
Table 1. Demographic and laboratory data of study population (n = 40).
Table 2. Technical parameters of MRI sequences used in the study.
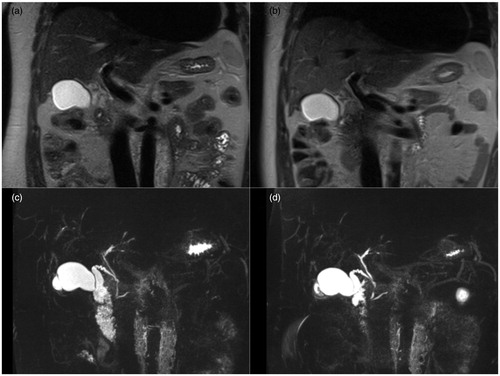
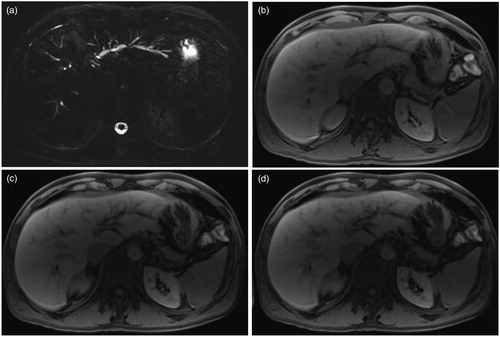
Figure 1. Gadoxetic acid-enhanced liver MRI examination of a 65-year-old male patient with PSC. Sequences included in imaging set with MRCP is depicted in (a) and without MRCP in (b). Both readers evaluated each data set in two-time points simultaneously and at two separate reading sessions.
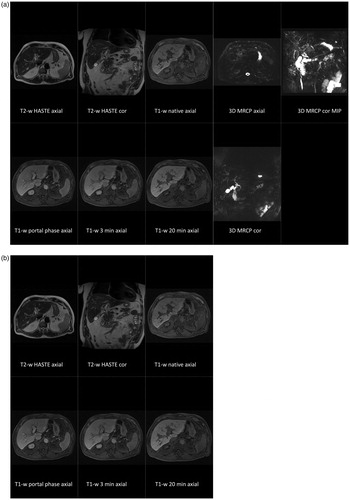
Table 3. Interpretation of radiological course of morphological changes of common bile duct and common hepatic duct (CBD/CHD), right-sided (RIHBD) and left-sided intrahepatic bile ducts (LIHBD) between two serial follow-up MRI examinations for imaging set with MRCP for reader A/B.
Table 4. Interpretation of radiological course of morphological changes of common bile duct and common hepatic duct (CBD/CHD), right-sided (RIHBD) and left-sided intrahepatic bile ducts (LIHBD) between two serial follow-up MRI examinations for imaging set without MRCP for reader A/B.
Table 5. Inter-reader agreement (ICC) between two serial follow-up MRI examinations for imaging sets with (+MRCP) and without MRCP (-MRCP) regarding interpretation of the radiological course of morphological changes of common bile duct and common hepatic duct (CBD/CHD), right-sided (RIHBD) and left-sided intrahepatic bile ducts (LIHBD).
Table 6. Intra-reader agreement (ICC) for readers A and B between imaging sets with and without MRCP regarding interpretation of the radiological course of morphological changes of common bile duct and common hepatic duct (CBD/CHD), right-sided (RIHBD) and left-sided intrahepatic bile ducts (LIHBD).
Table 7. Absolute number of cases with agreement and disagreement between readers for interpretation of radiological course of morphological changes of common bile duct and common hepatic duct (CBD/CHD), right-sided (RIHBD) and left-sided intrahepatic bile ducts (LIHBD) between two serial follow-up MRI examinations for imaging sets with (+MRCP) and without MRCP (-MRCP).