Figures & data
Table 1. Characteristics pregnant and non-pregnant IBD patients.
Figure 2. Disease course of IBD patients before, during and after pregnancy. (A) Significantly more UC/IBD-U patients than CD patients experienced relapses during pregnancy (36% vs 14.7%, respectively, p = .021) and post-partum (68% vs 30.7%, respectively, p = .01). Also, fewer CD patients presented with relapse post-partum as compared to pre-pregnancy (66.7% vs 30.7%, respectively, p = .01). (B) Mean relapses per person per year during the complete follow up time. For the patients who became pregnant this is displayed as 3 years pre-pregnancy and 4 years after pregnancy.
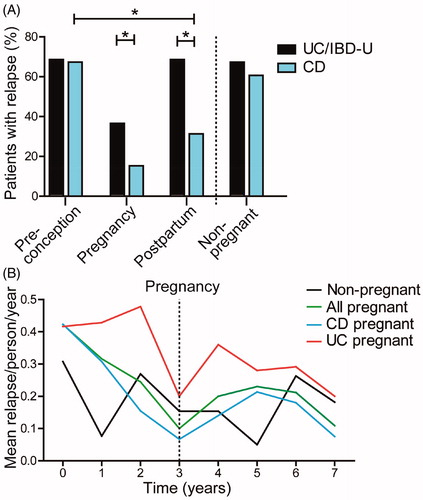
Figure 3. Endoscopy scores of IBD patients before and after pregnancy. (A) Comparison of the median SES-CD endoscopy scores divided by segments obtained during endoscopy. No significant difference in score between preconception and post-partum was seen (1.4 [IQR, 0.5] vs 1.4 [IQR, 0.6], respectively, p = .56). Furthermore no significant difference was found when post-partum score of pregnant patients was compared to non-pregnant patients (1.4 [IQR, 0.6] vs 2.2 [IQR, 2.2], respectively, p = .15). (B) Comparison of MAYO scores for UC obtained during endoscopy. We did not find a significant difference in score between preconception and post-partum (2 [IQR, 0] vs 2 [IQR, 0.15], respectively, p = .94). Also no significant difference was found when post-partum was compared to non-pregnant patients (2 [IQR, 0.15] vs 2 [IQR, 0.38], respectively, p = .52).
![Figure 3. Endoscopy scores of IBD patients before and after pregnancy. (A) Comparison of the median SES-CD endoscopy scores divided by segments obtained during endoscopy. No significant difference in score between preconception and post-partum was seen (1.4 [IQR, 0.5] vs 1.4 [IQR, 0.6], respectively, p = .56). Furthermore no significant difference was found when post-partum score of pregnant patients was compared to non-pregnant patients (1.4 [IQR, 0.6] vs 2.2 [IQR, 2.2], respectively, p = .15). (B) Comparison of MAYO scores for UC obtained during endoscopy. We did not find a significant difference in score between preconception and post-partum (2 [IQR, 0] vs 2 [IQR, 0.15], respectively, p = .94). Also no significant difference was found when post-partum was compared to non-pregnant patients (2 [IQR, 0.15] vs 2 [IQR, 0.38], respectively, p = .52).](/cms/asset/3558bfdb-5386-4598-b4c7-6c768646052d/igas_a_1910996_f0002_b.jpg)
Figure 4. Relapse rate before, during and after pregnancy of IBD patients stratified by treatment regimen. (A) Comparison of anti-TNFα treatment only versus other monotherapy (thiopurine, systemic corticosteroids, 5-ASA or Naltrexone). Post-partum relapse rate was lower in patients using anti-TNFα. Data during pregnancy is not shown since in our center, women discontinue anti-TNFα use from week 22 onwards. (B) Patients using anti-TNFα and thiopurine as combination therapy post-partum experienced less relapses when compared to patients using other combination therapy (anti-TNFα and steroids, thiopurine and 5-ASA, thiopurine and steroids, 5-ASA and steroids). (C) Thiopurine use only did not affect relapse rate from IBD patients as compared to other single treatment. Thio: Thiopurine.
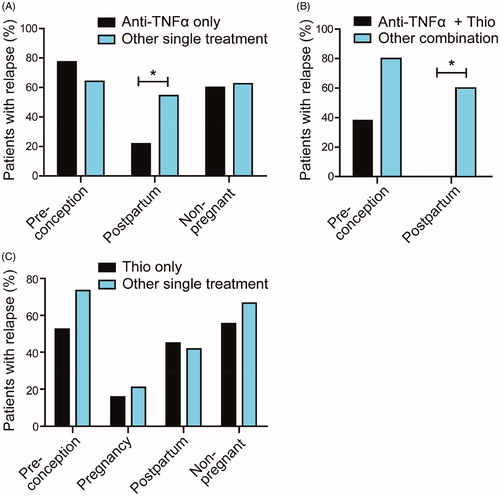
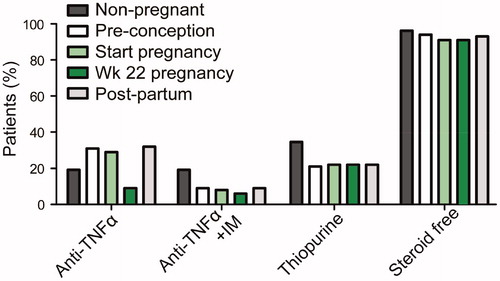
Figure 1. Medication regimen of non-pregnant and pregnant patients. For pregnant patients, pre-pregnancy, start of pregnancy, week 22 of pregnancy and post-partum medication use is indicated. Percentage of patients using anti-TNFα, using anti-TNFα plus immunomodulators (IM), using thiopurines and those that are steroid free are indicated.