Figures & data
Figure 1. An 80-year-old woman with cardiovascular disease (previous coronary artery bypass graft surgery) and severe emphysema from 40 packs per year smoking history developed an early stage non-small cell lung cancer and was referred for tumour ablation due to her high operative risk. (A) Axial CT image in lung windows shows the 1.4 cm left upper lobe NSCLC (arrow). (B) Axial fluorodeoxyglucose PET/CT fusion image shows intense standard uptake value (SUV) of 6.8 (arrow) without evidence of regional or distant spread (Stage IA). (C) Axial image during the microwave ablation shows satisfactory placement of the antenna within the centre of the mass parallel to the long axis (arrow) and (D) after 10 min of heating with 65 W a circumferential ’ground glass halo’ appears indicative of thermal damage to the mass and adjacent normal lung; (E) 1-month and (F) 6-month follow-up CT scans show the baseline thermal scar with antenna tract still visible (arrow) and expected involutional changes at 6 months.
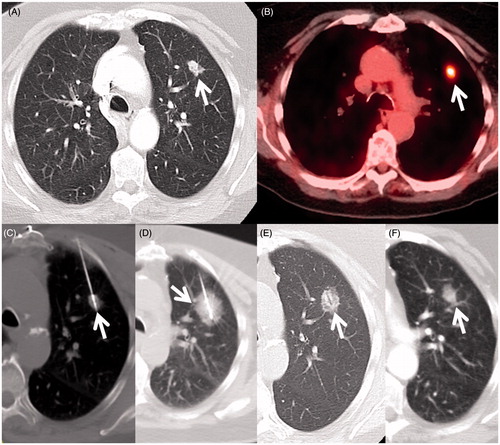
Figure 2. A 70-year-old woman with a 45 packs per year smoking history and previous lung cancer surgery on the left had a mass in the right lung discovered on chest X-ray. (A) Axial CT scan shows a 2.7-cm elliptical mass with central cavitation abutting the visceral pleural surface (arrow). (B) Axial FDG PET image shows intense uptake with standard uptake value of 10.9 (arrow) with no regional or distant disease (Stage IB). Biopsy confirmed squamous cell carcinoma and she was referred for ablation due to her high operative risk. (C) Axial image during the microwave ablation shows satisfactory placement of the antenna within the centre of the mass parallel to the long axis (arrow) and (D) after 10 min of heating with 65 W a circumferential ground glass halo appears; (E) 10- and (F) 14-month follow-up CT scans show a small growing nodule adjacent to the ablation zone consistent with recurrence (arrow). The patient returned for retreatment. (G) Axial CT image shows MW antenna in the recurrence. Extrapleural lidocaine was used to protect the chest wall (small arrows) (H) Axial CT image 30 months after initial ablation shows an air filled cavity and no recurrence at the treatment site (arrow).
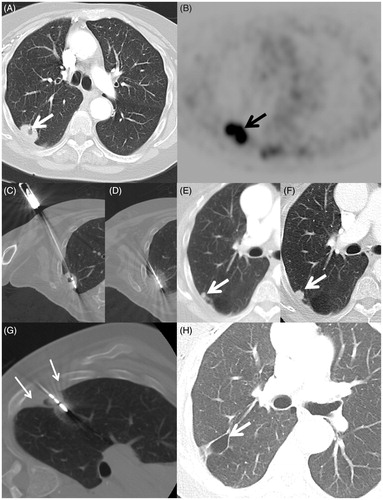
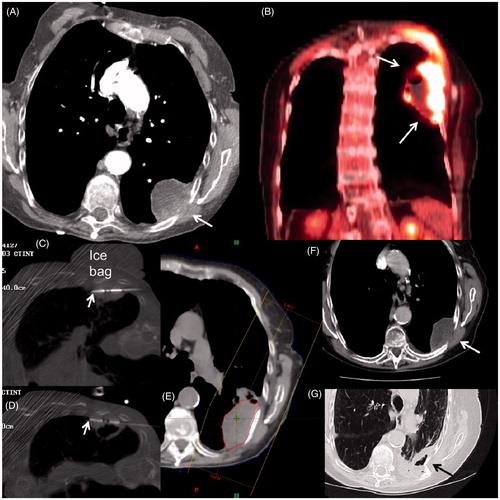
Figure 3. An 84-year-old woman with history of severe COPD from extensive cigarette smoking on oxygen therapy presented with severe left chest wall pain. (A) Axial CT scan shows a large necrotic mass with extension into chest wall (arrow) which was confirmed to be squamous cell carcinoma on subsequent biopsy. (B) Coronal image from staging FDG PET/CT shows extensive uptake with central necrosis without evidence of regional or distant spread (Stage 2B). Based on size and necrosis, a combination treatment with MWA and radiotherapy was planned. (C, D) Axial CT-fluoroscopic images show two antennas (arrows) placed superiorly and inferiorly within the mass close to the chest wall. Note the placement of the cold saline bag placed on the skin to reduce heating during the MWA. The patient’s pain was markedly relieved within 24 h of the MWA. (E) Image from subsequent radiation treatment plan targeting the mass. (F) Axial CT follow-up images at 6 months and (G) 2 years after treatment shows central necrosis (white arrow) and eventual shrinkage and cavitation (black arrow). The patient died of her respiratory disease, but not from her lung cancer.