Figures & data
Figure 1. (A) An intravenous catheter (arrow) was inserted into the shallow site (a), and then, a small amount of saline was injected to separate the intestinal tract (*) from the uterus surface. (B) The catheter was inserted deeper, and the process (A) was repeated until the tip of the catheter (arrow) was positioned between the uterus and the bowel (*) under ultrasound guidance. (C) After anechoic artificial ascites was introduced, the gap between the uterus and abutting bowel (*) was widened. We then found a better antenna path. (D) Artificial ascites fluid was added into the pelvis, separating the uterus from adjoining structures by more than 5 mm. The separation was still identifiable after 15 min of ablation (Arrow = antenna, a = ablation zone, b = artificial ascites). Complete separation was achieved in this patient.
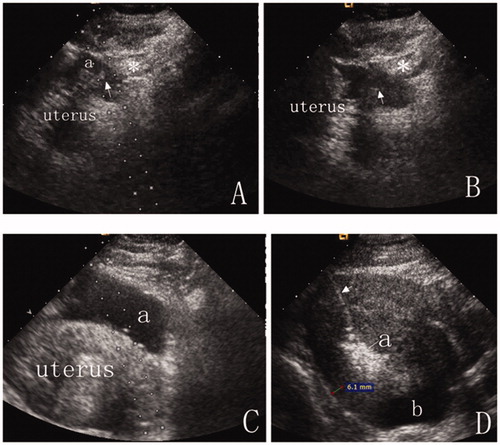
Figure 2. A 43-year-old woman with diffuse adenomyosis. (A) T2WI before MWA. The anterior uterine wall was extensively involved with adenomyosis. A bowel loop was close to the anterior uterine wall. (arrow = bowel). (B) A percutaneous approach was difficult due to bowel interference under ultrasound guidance. (C) After anechoic artificial ascites fluid was added, part of the uterus was separated from the bowel, and a distinct adhesion (arrow) was observed between the uterus and the adjacent bowel (*). (D) A CEUS image displays the ablative margin. The ablative margin (#) is more than 0.5 cm from the serosa where the uterus was not separated from the adjacent structures due to distinct pelvic adhesion (arrow). The ablative margin (*) was 0.3 cm from the uterine serosa where the uterus was completely separated from the adjacent organs by artificial ascites (a). (E) Enhanced T1WI at five days after MWA. The dark shadow indicates the area of lesion ablation (nonperfused volume, NPV). The percentage of NPV in this patient was 72%. The ablative margin was 0.7 cm from the distinct adhesion between the uterus and the bowel (arrow = distinct adhesion between uterus and bowel; a = uterine endometrium).
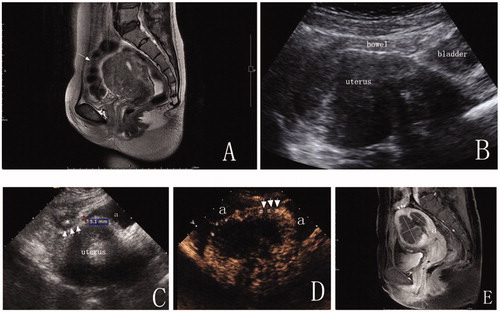
Table 1. Baseline information; means ± SD or median (P25-P75).
Table 2. Technical efficacy and therapeutic results at the 3-month follow-up.
Table 3. Complications after percutaneous microwave ablation.
