Figures & data
Table 1. Dielectric and thermal parameter values at 70 MHz for the various tissue types used in the simulations: electrical conductivity (σ [S m−1]), relative permittivity (εr [-]), density (ρ [kg m − 3]), specific heat capacity (Ct [J kg−1 K−1]), thermal conductivity (k [W m−1 K−1]) and perfusion (ω Cb [J m−3 s−1 K−1])
Table 2. Overview of the volume of liquid in the bladder at the end of treatment, the volume of air, and the area of the contact surface between the air pocket and the bladder wall, both in absolute and relative measures.
Table 3. Effect of the presence of an air pocket in the bladder on the SAR.
Table 4. Effect of the presence of an air pocket in the bladder on the temperature distribution.
Figure 1. Effect of the presence of an air pocket on the SAR distribution in a typical patient (patient #6) compared to the situation without air pocket. The effect is mostly localised around the air pocket. Shown are (a) a coronal view, (b) a sagittal view and (c) a transversal view through the bladder’s center of gravity. The right-hand column shows zoomed in versions of the bladder region.
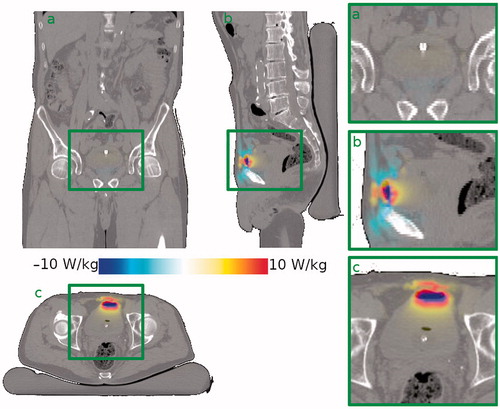
Figure 2. Effect of the presence of an air pocket on the steady state temperature distribution in a typical patient (patient #6) compared to the situation without air pocket. Since the air pocket acts as a thermally insulating layer, the liquid inside the bladder loses less heat to the upper part of the bladder wall. This leads to a higher temperature in the bladder contents, a slightly higher temperature in the upper part of the bladder wall, still in contact with the liquid bladder contents, and a lower temperature in the part of the bladder wall in immediate contact with the air pocket. Shown are (a) a coronal view, (b) a sagittal view and (c) a transversal view through the bladder’s center of gravity. The right-hand column shows zoomed in versions of the bladder region. Gravity points into the paper, to the left, and to the bottom, respectively.
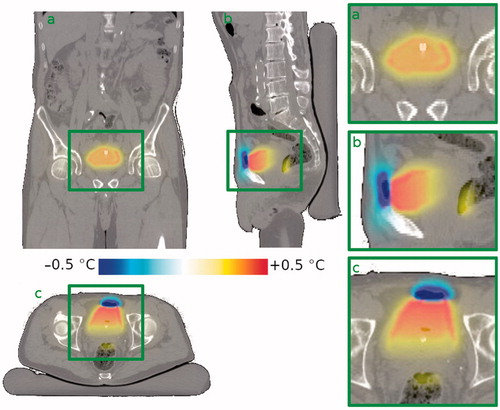
Figure 3. Steady state temperature profile along the cardinal axes, through the bladder’s center of gravity, for a typical patient (patient #6). Vertical purple lines show the outside of the bladder wall, yellow lines the interface between the bladder contents and the bladder wall and the red line the interface between the bladder contents and the air pocket. It is observed that the air pocket causes the bladder contents, and hence the bladder wall in contact therewith, to be slightly warmer, the effect increasing towards the air pocket. The air pocket itself, and the part of the bladder wall in contact therewith, however, are cooler than they would be in the absence of an air pocket. Shown are profiles for the patient’s left-to-right (top), anterior-posterior (middle) and caudal-cranial (bottom) directions.
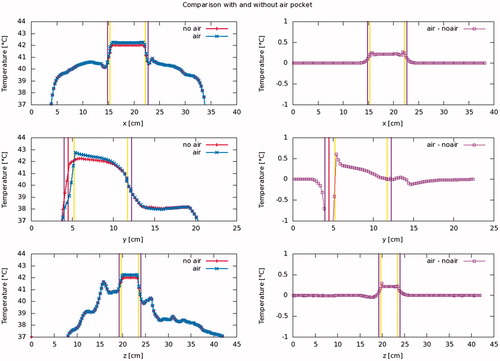
Figure 4. Predicted changes in median temperature (T50) of the bladder content (blue circles) and bladder wall (red squares) plotted against air pocket volume for 16 NMIBC patients. On average, the median temperature in the bladder contents is slightly (0.1 °C) higher if there is an air pocket present in the bladder, and the temperature appears to increase slightly with increasing air pocket volume. The median bladder wall temperature is slightly (0.1 °C) lower in the presence of an air pocket, but there is no correlation with air pocket size.
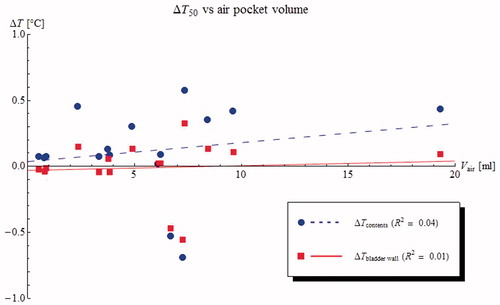
Figure 5. Predicted changes in T90 (blue circles) and T10 (red squares) bladder wall plotted against air pocket contact surface for 16 NMIBC patients. The presence of an air pocket in the bladder has the undesirable effect of making the bladder wall temperature less homogeneous, increasing the T10 and decreasing the T90.
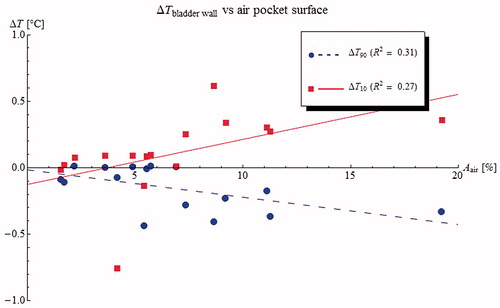
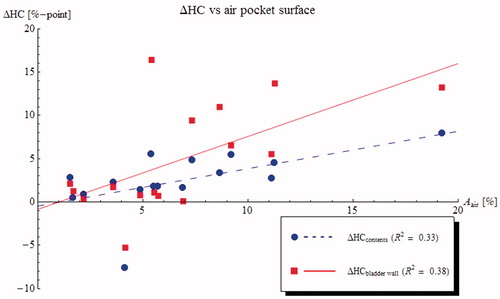
Figure 6. Predicted changes in heterogeneity coefficient (HC = (T10 − T90)/(T10 − 37 °C)) for the bladder contents (blue circles) and the bladder wall (red squares) plotted against air pocket contact surface for 16 NMIBC patients. The presence of an air pocket in the bladder increases the heterogeneity of the bladder wall temperatures, but has less effect on the heterogeneity of the bladder contents.