Figures & data
Figure 1. (a) Sagittal CT image of an OO located in the neck of femur (circle). The nidus is sclerotic. There is no need to protect any surrounding structures during ablation (group (a)). L corresponds to the diameter of the transducer (L/2 = 50 mm) and d to the distance between the focal point and the skin (d = 61 mm). The plane perpendicular to d and containing AB is shown in the bottom right of figure (a): in this case, 12% of the US beam would be obstructed by the great trochanter. (b) Axial CT image illustrating laser ablation of the OO. A 14-gauge penetration set was used to drill the nidus. The laser fiber was inserted coaxially in an 18-gauge spinal needle (arrow).
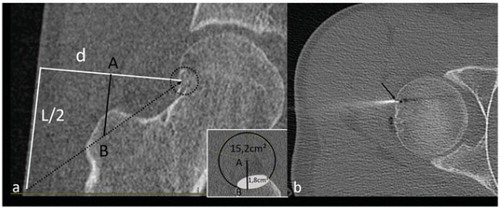
Figure 2. (a) CT-scan showing a mixed metastasis of the scapula (group (a)). L (100 mm) corresponds to the diameter of the transducer and d to the distance between the focal point and the skin (d = 18 mm). (b, c) Sagittal (b) and coronal (c) CT reconstructions showing placement of two cryoprobes used to freeze the lesion. The hypoattenuation surrounding the lesion corresponds to the ice-ball.
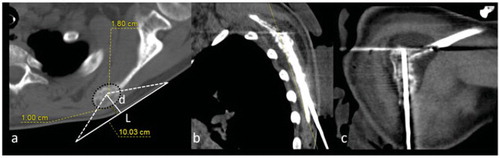
Figure 3. (a) CT-scan of an OO located in the right articular process of L5 (group (b)). The nidus is sclerotic. This case requires protection of the nerve root in the foramen (F for foraminal dissection) and the lumbar canal (E for epidural dissection). As the aim is to heat the nidus to 60 °C, foraminal and medullary canal temperatures may increase up to 45 °C, which may injure the nerve roots. The trajectory of the spinal needles for dissection are represented by dotted arrows. L corresponds to the diameter of the transducer (100 mm) and d to the distance between the focal point and skin (d = 66 mm). (b, c) CT-scan showing insertion of needles for ablation of the OO. A cryoprobe inserted coaxially in a 15-gauge needle is used to access the nidus (b, arrow) and 18-gauge needles are placed for epidural (b) and foraminal (c) dissections (dotted arrows).
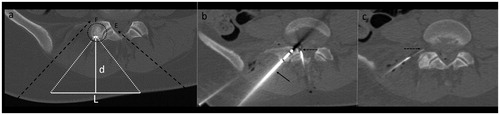
Figure 4. (a) CT-scan of a sclerotic metastasis (group (b)) of the ilium (dotted circle). L corresponds to the diameter of the transducer (100 mm) and d the distance between the focal point and the skin (d = 100 mm). (b, c) CT-scan showing cryoablation of the lesion performed with a 17-gauge cryoprobe inserted coaxially in a 14-gauge penetration set (b, arrow), associated with dissection (b, dotted arrow) of the sciatic nerve (b, star) and coxofemoral articulation (c, dotted arrow). Dissection fluid contains iodinated contrast (+) to optimize CT visibility.
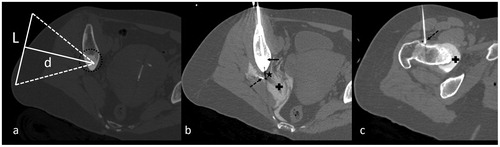
Figure 5. (a) Axial CT image showing an 8-mm OO in the left pedicle of C4. The vertical white line (L = 100 mm) represents optimal transducer placement. The white line (d = 30 mm) corresponds to the depth of the OO. In this case, cooling of the C5 foraminal space is mandatory but impossible due to transducer bulk. This case was considered ineligible for HIFU (group (c)). (b, c) Axial CT image demonstrating ablation: an 18-gauge spinal needle with a coaxially inserted thermocouple for temperature monitoring was positioned in the C4–C5 foramen, in contact with the C5 nerve root (b, arrow). The laser fiber was then inserted coaxially in an 18-gauge needle, with the tip in the center of the nidus (c, arrow).
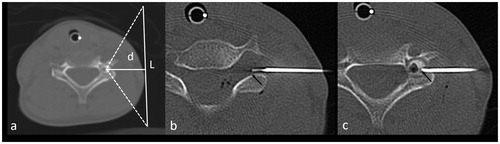
Figure 6. (a) Axial CT image of an osteolytic metastasis (dotted ellipse) in the sacrum. In this case, considering the deep location of the lesion in relation to the sacral canal (S) and sacral foramina (stars), there is no suitable access for the US beam (group (c)). (b, c) CT-scan images showing ablation of the lesion. Manual instillation of 0.9% normal saline in the sacral foramina was performed for thermo-protection (b). The ablative probe was inserted coaxially in a 14-gauge penetration set, introduced laterally into the lesion.
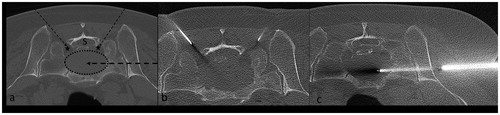
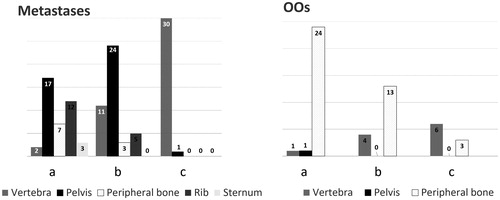
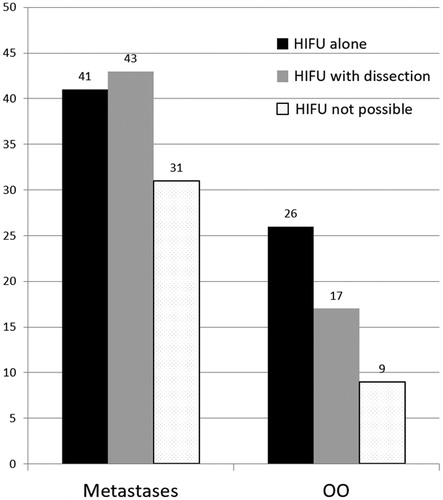
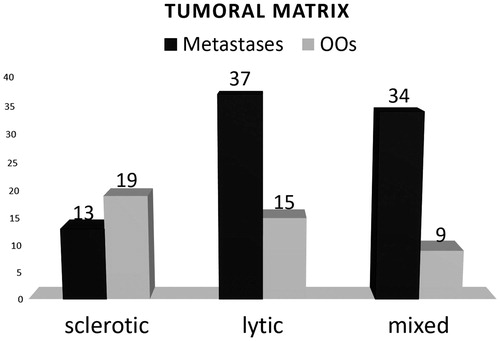
Figure 7. Classification resulting from our suitability study according to lesion location, for metastases and OOs. Categories a, b and c correspond to (a) lesions suitable for MRgHIFU therapy alone; (b) lesions suitable for MRgHIFU if protection of surrounding structures and/or bone consolidation is performed; (c) lesions not suitable for MRgHIFU.