Figures & data
Figure 1. A 25-year-old woman presented with a recurrent tumor in the left neck operation bed close to the esophagus and tracheoesophageal groove (a). Before RFA, a hydrodissection technique was applied to obtain a safety margin from the esophagus and recurrent laryngeal nerve (b). An RF electrode with a 0.4 cm size active tip was inserted into the recurrent tumor and the ablation was started (c). During ablation, the patient complained that her voice had changed. Ablation was stopped immediately and a cold dextrose solution was injected directly around the ablated tumor (d). After injecting 15 ml of cold dextrose solution, the patient’s voice completely improved (e).
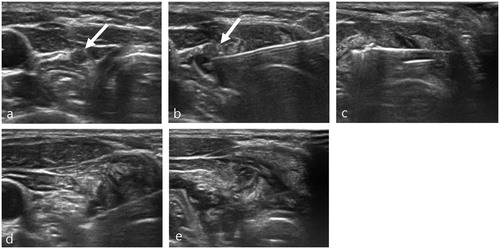
Figure 2. A 55-year-old woman who presented with a large nodule in the left thyroid gland (a). Pre-ablation US evaluation revealed a medial type middle cervical sympathetic ganglion located close to the thyroid nodule (b,c). An RF electrode with a 1 cm size active tip was used for ablation (d). During ablation, ipsilateral conjunctival injection was detected, which is one of the early symptoms of Horner syndrome. Ablation was stopped immediately and a cold dextrose solution was injected directly into the perithyroidal area (e). After injection of 7 ml of cold dextrose solution, the patient’s symptoms had completely improved (e).
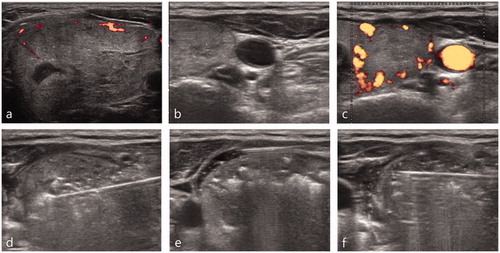
Table 1. Summary of the basic characteristics and clinical manifestations of the 17 patients.
Table 2. Comparison of clinical data between patients who received a cold dextrose solution injection for nerve damage and those who did not.
