Figures & data
Figure 1. 59-year-old man with metastatic lung cancer and painful T7 pathologic fracture. Sagittal T1-weighted fat-saturated contrast-enhanced MR image (A) shows enhancing bone marrow replacing lesion within T7 vertebral body with pathologic compression fracture (A, arrow). Anterior-posterior fluoroscopic image during simultaneous bipedicular radiofrequency ablation (B) shows medial articulation of electrode tips which are 5–10 mm apart (width of the spinous process as landmark). Radiofrequency ablation was performed for a total of 16 min, and immediately followed by vertebral augmentation (not shown). Sagittal STIR MR image obtained 6 months following treatment (C) shows local tumor control with no evidence of recurrence (C, arrow). Note hypointense cement within vertebral body.
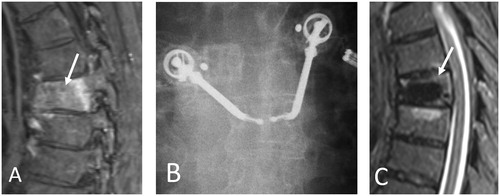
Figure 2. 60-year-old woman with metastatic peripheral nerve sheath tumor previously managed by surgical resection and adjuvant chemoradiation therapy presenting with recurrent tumor involving upper lumbar vertebral posterior elements and paraspinal soft tissues. Axial FDG-PET-CT image (A) shows hypermetabolic soft tissue mass within posterior upper lumbar paraspinal soft tissues (A, arrow). Prone axial (B) CT image during cryoablation shows placement of a cryoprobe (a total of 3 cryoprobes were used) within the lesion with hypoattenuating ice ball encompassing the tumor volume (B, arrows). Axial FDG-PET-CT image obtained 3 months following cryoablation (C) shows local tumor control with no evidence of residual or recurrent tumor (C, arrow).
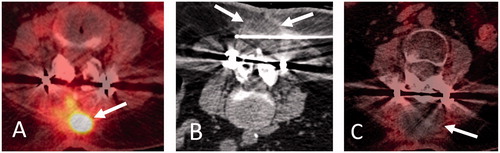
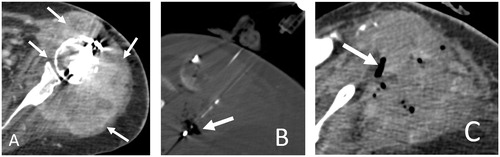
Figure 3. 55-year-old woman with metastatic lung adenocarcinoma and progressively enlarging left shoulder girdle metastatic lesion and intractable pain minimally relieved by oral and intravenous pain medications, admitted for pain palliation. Axial contrast-enhanced CT image (A) shows metastatic lesion involving the proximal humerus and scapular glenoid with glenohumeral intra-articular extension and surrounding shoulder girdle musculature involvement (A, arrows). Note metallic streak artifact from implants transfixing a proximal humerus pathologic fracture (not shown). Axial CT image during microwave ablation (B) shows placement of two microwave antennae within the soft tissue component of the metastatic lesion. Microwave ablation was performed at 100 Watts for a total of 10 min achieving overlapping 4 × 4 cm ablation zones. Antennae were repositioned caudally to ablate the inferior component of the lesion with identical ablation parameters. Note intra-tumoral gas from tissue vaporization (B, arrow). Axial CT image immediately following microwave ablation (C) shows largely CT-occult ablation zone with intra-tumoral gas from tissue vaporization (C, arrow). The patient endorsed substantial pain improvement.