Figures & data
Figure 1. Imaging before microwave ablation (MWA) in a 63-year-old woman with left central intraductal papilloma (IDP). (A) Ultrasound (US) scan before MWA shows the dilated duct with hypoechoic IDP (yellow arrow) connected to the nipple (red arrow). The dilated duct is in the middle of nipple (green arrow). (B) Contrast-enhanced US before MWA shows both the dilated duct and lesion hypo-enhancement with a size 2.0 × 0.3 × 0.4 cm. (C) Sagittal contrast-enhanced magnetic resonance imaging (MRI) shows hyperintense duct (arrow) in the left breast before MWA in the arterial phase.
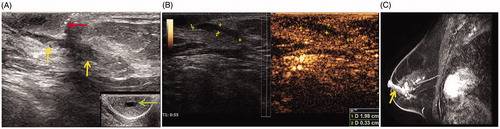
Figure 2. US imaging during MWA in the patient. (A) US shows 16 G core needle biopsy (arrow) of the hypoechoic lesion. (B) US showing the 22 G fine needle (yellow arrow) at the depth of the nipple for saline infusion (red arrow). (C) US showing the 16 G MWA needle (arrow) ablating the dilated duct and intraductal papilloma with the hyperechoic zone.
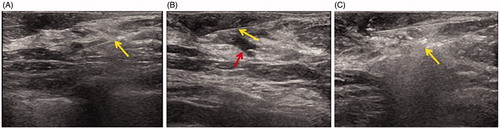
Table 1. The clinical features of patients and masses.
Figure 3. Image after MWA in the patient. (A) After MWA, only a pinhole-sized scar is visible on the skin (yellow arrow); around the ablation zone, skin flushing (red arrow) can be seen, which resolved in 1 week after 3-day antibiotic treatment. (B) US showing the heterogeneous ablation zone (measure markers) adjacent to the nipple (arrow) with a size 1.7 × 1.3 cm at 6 months after MWA. (C) Contrast-enhanced MRI image showing hypointense MWA treatment zone (arrow) in the arterial phase.
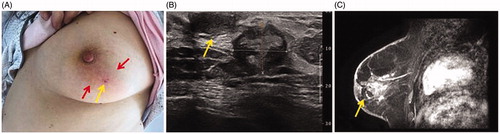
Table 2. The effect of IDPs volume reduction after MWA.
