Figures & data
Table 1. Inclusion and exclusion criteria in patients with thyroid nodules.
Table 2. Baseline characteristics of the whole cohort.
Table 3. Description and comparison of patient characteristics and nodules according to intervention group.
Table 4. Comparison of volume reduction over time and between radiofrequency and laser ablation.
Table 5. Comparison of the safety and efficacy in the two groups at the last post-thermal ablation evaluation.
Figure 2. Median nodule volume reduction over time, in the two interventional groups. Percentage decrease significantly differed when comparing RFA to laser ablation treatment at 6 weeks (p < .0001). *p value significance < .05; ** Not statistically significant.
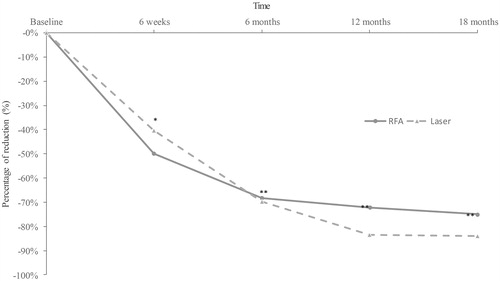
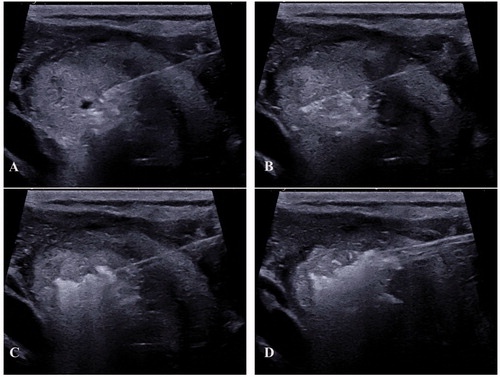
Figure 4. ‘pTA-UsNodule’: post-Thermal-Ablation Ultrasound Nodule. The electrode is introduced slowly in the nodule (A) after a peri-capsular anesthesia with lidocaine. The electrode is located one centimeter before the limits of the nodule (to avoid carotid and vagal nerve contact = ‘danger zone’) (B). The micro bubbles correspond to gas due to carbonization of the tissue (hyper-echoic aspect) (C). The electrode was slowly removed until the anterior limit (see bubbles around the nodule) (D).