Figures & data
Figure 1. Display interface of the NeuroBlade System during ablation of deep-seated occipital brain metastases. Using this interface it is possible to assess the extent of ablation in three axial levels perpendicular to the laser probe (upper panels). On the bottom panels, it is possible to observe the sagittal and coronal planes, parallel to the probe. Note use of DTI-tractography (in white) to generate the optic radiations.
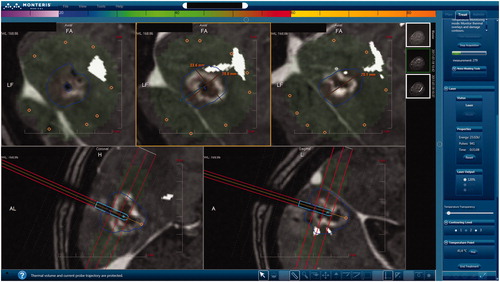
Table 1. Large published cohorts on the use of LITT treat brain metastases.
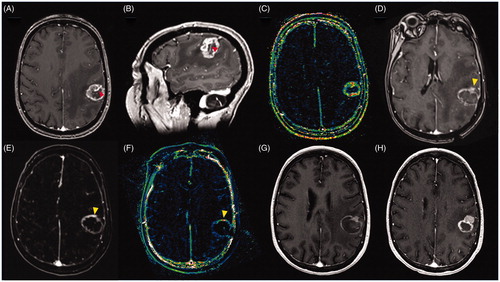
Figure 2. Images of 67-year-old male patient with a brain metastases recurrence after SRS from non-small cell lung cancer. (A) Pre-ablation axial T1C + MRI showing a deep seated ring enhancement in the left parietal lobe, compatible with recurrent tumor; (B) Pre-ablation Dynamic Contrast-Enhanced k-trans MR showing a high signal intensity inside the lesion suggesting high vascularization; (C) Post-ablation axial T1C + MRI showing the classic eggshell enhancement in the borders of the ablation; (D) Post-ablation MRI subtraction compatible with complete ablation; (E) Post-ablation axial Dynamic Contrast-Enhanced k-trans MR showing low signal intensity compatible with no viable tissue within the ablation zone; (F) One month post-ablation axial T1C + MRI showing eggshell enhancement and no signs of local recurrence; (G) Three month post-ablation axial T1C + MRI without local recurrence; (H) Six month post-ablation axial T1C + MRI with only remnant signs of ablation.
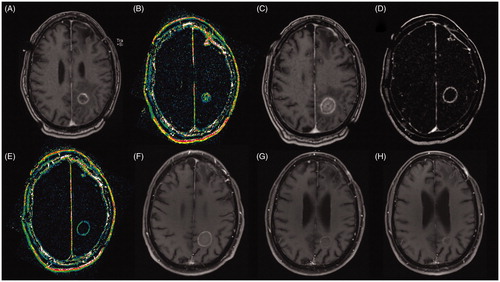
Figure 3. Images of 66-year-old female patient with metastatic breast cancer to the brain with a tumor recurrence after treatment with SRS. (A) Pre-ablation axial T1C + MRI showing a heterogeneous ring-enhancing lesion in the left frontoparietal region, compatible with recurrent tumor, note the large caliber vessel in the anterior third of the lesion (red arrow); (B) Pre-ablation sagittal T1C + MRI showing the large caliber vessel crossing the lesion; (C) ) Pre-ablation Dynamic Contrast-Enhanced k-trans MR showing a high signal intensity in the lesion’s margins compatible high vascularization; (D) Post-ablation axial T1C + MRI showing the classic eggshell enhancement in the margins of the ablation, notice in the anterior margin a solid enhancement compatible with unablated tissue (yellow arrow), it is possible that the large vessel worked as a heat sink preventing the complete ablation of the lesion; (E) Post-ablation MRI subtraction showing increased enhancement in the anterior margin of the ablation zone (yellow arrow); (F) Post-ablation axial Dynamic Contrast-Enhanced k-trans MR showing increased signal in the anterior margin of the ablation zone (yellow arrow); (G) One month post-ablation axial T1C + MRI showing eggshell enhancement a remnant unablated tumor in the anterior margin of the ablation zone; Three months post-ablation axial T1C + MRI showing tumor recurrence in the anterior part of the ablation zone.