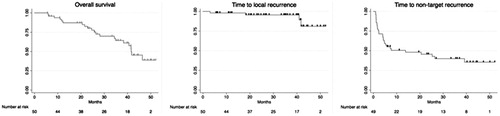
Figures & data
Table 1. Summary of acquisition parameters for planning, targeting, monitoring and controlling.
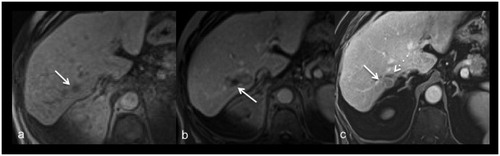
Figure 1. 79-years-old male patient treated for a singular hepatic metastasis of a melanoma. Unenhanced T1-weighted planning imaging (a) depicts the target tumor in segment V (arrow) measuring 18 mm. Contrast-enhanced control imaging in the portal-venous phase shows the ablation zone with the contour of the treated tumor (b). Die smallest safety margin was measured with 5 mm at the lateral portion of the ablation zone (arrow).
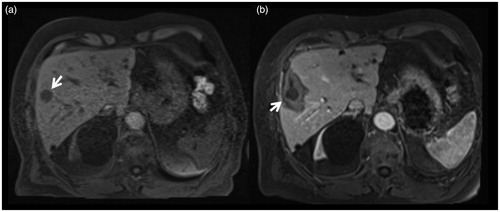
Table 2. Baseline patient characteristics and ablation procedure related parameters.
Figure 2. Images of a 56-year-old male patient with metastasis of a mixed adenoneuroendocrine carcinoma in segment VIII. Metastasis is clearly depictable in planning imaging without administration of intravenous contrast agent (a; arrows). During first targeting with MR fluoroscopy (b) the applicator was positioned toward the cranial part of the metastasis (arrow). After ablation for 10 min with 18 kJ there is no coagulated tissue visible on the caudal part in monitoring (c; circle). Therefore, the applicator was repositioned (d) for an additional ablation for 15 min with 27 kJ toward the caudal part of the metastasis (e; circle). On final postprocedural imaging (f) there is a well-defined, T1-weighted hyterintense, oval shaped ablation zone with a 4 mm safety margin. No local recurrence was observed during follow-up.
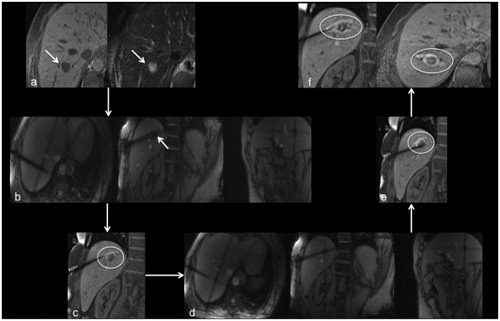
Table 3. Ablation procedure related parameters.
Table 4. Summary of complications according to the SIR reporting system.
Figure 3. Images of a 77-year-old female with metastasis of a melanoma. Planning imaging (a) depicts the small metastasis (17 mm) in segment VII (arrow). Post-procedural imaging (b) depicts an ablation zone with an almost non-visible safety margin dorso-medial (arrow). After 40 months local recurrence (arrow) was diagnosed on routine contrast-enhanced follow-up imaging (c) dorsal to the shrunken ablation zone (dash arrow).