Figures & data
Figure 1. Flow diagram of patients identified, included, and excluded. MWA: microwave ablation; HCC: hepatocellular carcinoma.
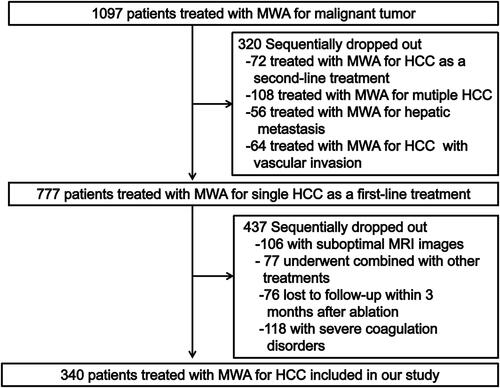
Figure 2. The graphical representations of four types of tumor recurrence after MWA. (A) LTP was defined according to imaging results of abnormal nodular, disseminated, and/or unusual patterns of peripheral enhancement around the ablation site in patients treated with MWA; (B) IDR was described as the appearance of an abnormal nodular, disseminated, or unusual patterns of peripheral enhancement of intrahepatic lesions, which were further away from the ablation zone after MWA treatment; (C) AIR was described as the generation of multiple nodular (≥3) distant from the edge of the ablation zone and the infiltrative recurrence in the treated liver segment that showed enhancement in hepatic arterial phase images and washout on portal or delayed venous phase images at follow-up. The AIR was confined to the initial manifestation of tumor recurrence in patients who were previously considered to have a disease-free status at least 6 months after initial MWA to avoid confusion with IDR [Citation18]; (D) EDR was defined as distant metastasis in the extrahepatic, which has the appearance of an abnormal nodular, disseminated, or unusual patterns of peripheral enhancement of intrahepatic lesions.
![Figure 2. The graphical representations of four types of tumor recurrence after MWA. (A) LTP was defined according to imaging results of abnormal nodular, disseminated, and/or unusual patterns of peripheral enhancement around the ablation site in patients treated with MWA; (B) IDR was described as the appearance of an abnormal nodular, disseminated, or unusual patterns of peripheral enhancement of intrahepatic lesions, which were further away from the ablation zone after MWA treatment; (C) AIR was described as the generation of multiple nodular (≥3) distant from the edge of the ablation zone and the infiltrative recurrence in the treated liver segment that showed enhancement in hepatic arterial phase images and washout on portal or delayed venous phase images at follow-up. The AIR was confined to the initial manifestation of tumor recurrence in patients who were previously considered to have a disease-free status at least 6 months after initial MWA to avoid confusion with IDR [Citation18]; (D) EDR was defined as distant metastasis in the extrahepatic, which has the appearance of an abnormal nodular, disseminated, or unusual patterns of peripheral enhancement of intrahepatic lesions.](/cms/asset/3121f302-da58-4d92-a814-33e8b105ce18/ihyt_a_1962548_f0002_c.jpg)
Table 1. Baseline patient characteristics.
Table 2. Univariate analysis for prognostic factors of four types of tumor progressions.
Table 3. Multivariate analysis for prognostic factors of tumor progression.
Figure 3. Kaplan–Meier curves comparing OS, RFS and four types of tumor progression outcomes after MWA between BCLC stage 0 and A group. (A) comparing OS between BCLC stage 0 and A group; (B) comparing RFS between BCLC stage 0 and A group; (C) comparing LTP between BCLC stage 0 and A group; (D) comparing IDR between BCLC stage 0 and A group; (E) comparing AIR between BCLC stage 0 and A group; (F) comparing EDR between BCLC stage 0 and A group. OS: overall survival; RFS: recurrence-free survival; MWA: microwave ablation; BCLC: Barcelona clinic liver cancer; LTP: local tumor progression; IDR: intrahepatic distant recurrence; AIR: aggressive intrasegmental recurrence; EDR: extrahepatic distant recurrence.
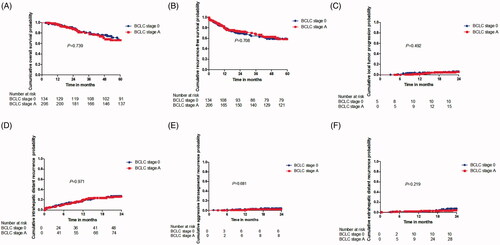
Figure 4. Overall survival curves for patients with and patients without TP of HCC after MWA. Curves were obtained with Kaplan–Meier method. (A) Overall survival curves for patients with and patients without LTP of HCC after MWA; (B) Overall survival curves for patients with and patients without IDR of HCC after MWA; (C) Overall survival curves for patients with and patients without AIR of HCC after MWA; (D) Overall survival curves for patients with and patients without EDR of HCC after MWA. HCC: hepatocellular carcinoma; MWA: microwave ablation; LTP: local tumor progression; IDR: intrahepatic distant recurrence; AIR: aggressive intrasegmental recurrence; EDR: extrahepatic distant recurrence.
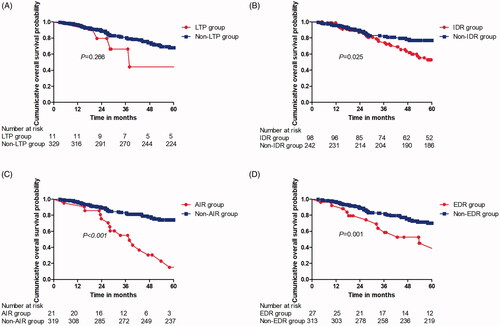
Table 4. Univariate and multivariable analysis of prognostic factors for overall survival after MWA.
