Figures & data
Figure 1. Flowchart of the patients selection. TACE: transarterial chemoembolization; P-ablation: palliative ablation; PSM: propensity score matching.
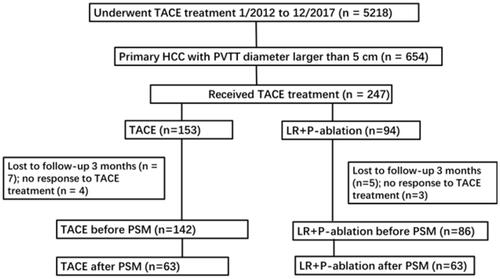
Table 1. Demographic and clinical characteristics of patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before and after propensity score matching (PSM), by type of treatment (TACE + P-ablation vs. TACE), January 2012 to December 2017.
Table 2. Tumor- and treatment-related characteristics of patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before and after propensity score matching (PSM), by type of treatment (TACE + P-ablation vs. TACE), January 2012 to December 2017.
Figure 2. Kaplan–Meier curves for progression-free survival (PFS) in 228 patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before propensity score matching (PSM), January 2012 to December 2017: (A) The PFS rates of the group of 86 patients who had transarterial chemoembolization (TACE) + palliative (P)-ablation (microwave ablation [MWA] and/or radiofrequency ablation [RFA]) were significantly higher than for the group of 142 patients who had only TACE (p < .001); (B) Of the group of 86 patients who had both TACE and P-ablation, for patients received more times of ablation had better PFS. Patients received more than 3 times of ablation had the best PFS. The OS rates were in good correlation with the times of P-ablation treatments (p = .03).
![Figure 2. Kaplan–Meier curves for progression-free survival (PFS) in 228 patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before propensity score matching (PSM), January 2012 to December 2017: (A) The PFS rates of the group of 86 patients who had transarterial chemoembolization (TACE) + palliative (P)-ablation (microwave ablation [MWA] and/or radiofrequency ablation [RFA]) were significantly higher than for the group of 142 patients who had only TACE (p < .001); (B) Of the group of 86 patients who had both TACE and P-ablation, for patients received more times of ablation had better PFS. Patients received more than 3 times of ablation had the best PFS. The OS rates were in good correlation with the times of P-ablation treatments (p = .03).](/cms/asset/35c70fdb-a18e-46a6-b80b-778e9be8d541/ihyt_a_2021303_f0002_c.jpg)
Table 3. Overall survival (OS) and progression-free survival (PFS) rates in patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before and after propensity score matching (PSM), by type of treatment (TACE + P-ablation vs. TACE), January 2012 to December 2017.
Table 4. Multivariate analyses of impact of clinical, tumor-related and treatment-related characteristicsa on progression-free survival (PFS) in 228 patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before and after propensity score matching (PSM), by type of treatment (TACE + P-ablation vs. TACE), January 2012 to December 2017.
Figure 3. Kaplan–Meier curves for overall survival (OS) in 228 patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before propensity score matching (PSM), January 2012 to December 2017: (A) The OS rates of the group of 86 patients who had transarterial chemoembolization (TACE) + palliative (P)-ablation (microwave ablation [MWA] and/or radiofrequency ablation [RFA]) were significantly higher than for the group of 142 patients who had only TACE (p < .001); (B) Of the group of 86 patients who had both TACE and P-ablation, for patients received more times of ablation had better OS. Patients received more than 3 times of ablation had the best OS. The OS rates were in good correlation with the times of P-ablation treatments (p = .025).
![Figure 3. Kaplan–Meier curves for overall survival (OS) in 228 patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before propensity score matching (PSM), January 2012 to December 2017: (A) The OS rates of the group of 86 patients who had transarterial chemoembolization (TACE) + palliative (P)-ablation (microwave ablation [MWA] and/or radiofrequency ablation [RFA]) were significantly higher than for the group of 142 patients who had only TACE (p < .001); (B) Of the group of 86 patients who had both TACE and P-ablation, for patients received more times of ablation had better OS. Patients received more than 3 times of ablation had the best OS. The OS rates were in good correlation with the times of P-ablation treatments (p = .025).](/cms/asset/0eaf64be-e15d-4bab-9b00-185a23eb1ae1/ihyt_a_2021303_f0003_c.jpg)
Table 5. Median overall survival (OS) in patients with different type of portal vein tumor thrombus (PVTT)a, before and after propensity score matching (PSM), by type of treatment (TACE + P-ablation vs. TACE), January 2012 to December 2017.
Table 6. Multivariate analyses of impact of clinical, tumor-related and treatment-related characteristicsa on overall survival (OS) in 228 patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), before and after propensity score matching (PSM), by type of treatment (TACE + P-ablation vs. TACE), January 2012 to December 2017.
Figure 4. Kaplan–Meier curves for (A) progression-free survival (PFS) and (B) overall survival (OS) in 59 patients with tumor size no more than 7 cm and portal vein tumor thrombus (PVTT), January 2012 to December 2017. PFS and OS rates for the group of 26 patients who had transarterial chemoembolization (TACE) + palliative (P)-ablation (microwave ablation [MWA] and/or radiofrequency ablation [RFA]) were significantly higher than for the group of 33 patients who had only TACE (p = .048 and p = .001, respectively).
![Figure 4. Kaplan–Meier curves for (A) progression-free survival (PFS) and (B) overall survival (OS) in 59 patients with tumor size no more than 7 cm and portal vein tumor thrombus (PVTT), January 2012 to December 2017. PFS and OS rates for the group of 26 patients who had transarterial chemoembolization (TACE) + palliative (P)-ablation (microwave ablation [MWA] and/or radiofrequency ablation [RFA]) were significantly higher than for the group of 33 patients who had only TACE (p = .048 and p = .001, respectively).](/cms/asset/4b9d1988-1bb5-4773-8fca-c0d0f2b27d54/ihyt_a_2021303_f0004_c.jpg)
Figure 5. Kaplan–Meier curves for (A) progression-free survival (PFS) and overall survival (OS) (B) in 126 patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), after propensity score matching (PSM), January 2012 to December 2017. PSM was used to create clinically comparable cohorts and to correct for potential biases, with patients matched 1:1 using the nearest neighbor method with a caliber of 0.05. OS and PFS rates for the group of patients who had transarterial chemoembolization (TACE) + palliative (P)-ablation (microwave ablation [MWA] and/or radiofrequency ablation [RFA]) were significantly higher than for the group of patients who had only TACE (p = .001 and p < .001, respectively).
![Figure 5. Kaplan–Meier curves for (A) progression-free survival (PFS) and overall survival (OS) (B) in 126 patients with hepatocellular carcinoma (HCC) and portal vein tumor thrombus (PVTT), after propensity score matching (PSM), January 2012 to December 2017. PSM was used to create clinically comparable cohorts and to correct for potential biases, with patients matched 1:1 using the nearest neighbor method with a caliber of 0.05. OS and PFS rates for the group of patients who had transarterial chemoembolization (TACE) + palliative (P)-ablation (microwave ablation [MWA] and/or radiofrequency ablation [RFA]) were significantly higher than for the group of patients who had only TACE (p = .001 and p < .001, respectively).](/cms/asset/1b2df373-727e-4026-8be2-e073d76480c1/ihyt_a_2021303_f0005_c.jpg)
