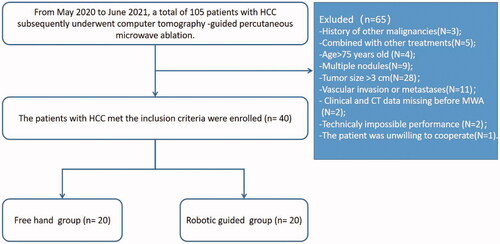
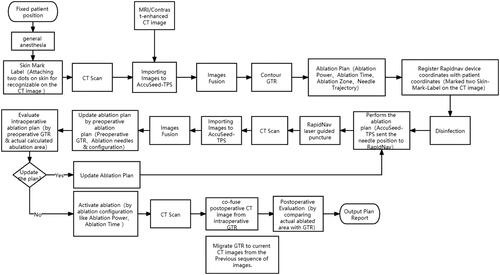
Figures & data
Figure 2. The needle position system consists of a circular rail as the main structure that paralleled with the CT scanning plane. ① A circular orbit for assisting needle position; ② a semicircular supporting structure with control panel fixed to the CT bed; ③ a movable collimator for guidance on the axial CT images; ④ a laser cross-line.
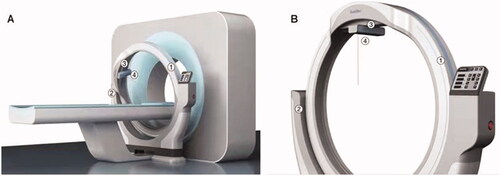
Figure 4. A 56 years, male patients with HCC (the lesion located on the liver segment V, and the maximum tumor diameter is 2.4 cm) who underwent robotic position for antenna in CT-guided microwave ablation was shown. In order to show the target more clearly on the CT image, this patient received hepatic artery embolization before ablation, and the location of the tumor in the target area was determined by lipiodol deposition. (A) Pre-ablation planning; (B) robotic position; (C) the laser cross-line to determine entry point; (D) an interventional radiologist perform the puncture by the robot guidance; (E) the MW antenna was inserted into the tumor according to the pre-ablation planning (yellow arrow); (F) according to the artificial intelligence algorithm, the preoperative tumor shape (yellow arrow) is transferred intraoperatively; (G) the MW antenna was fixed, ablation was performed; (H) the ablation area was outlined on CT image; (I) the ablation area (yellow arrow) was clear and no recurrence was found 1 month after operation.
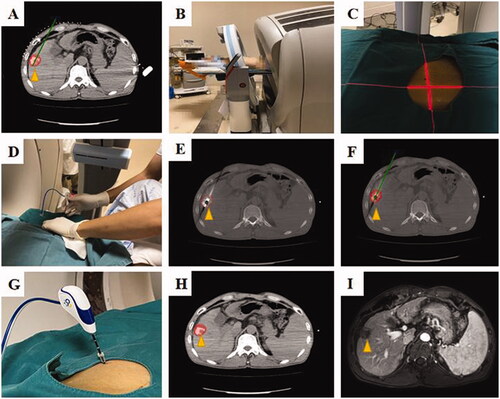
Table 1. Baseline characteristics of patients with HCC who underwent MWA.
Table 2. The comparison of technical outcomes between freehand and robot.
Table 3. Operational comfort and safety comparison between freehand and robot.