Figures & data
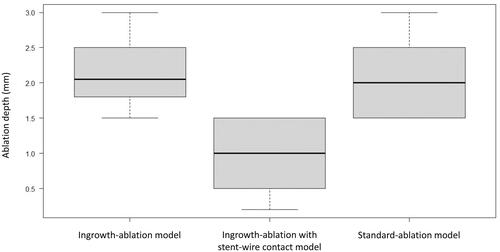
Figure 1. Prototype multifunctional RFA catheter. Four 2-mm ring electrodes are placed at the tip of the catheter at 3-mm intervals each. The catheter measures 2.8 mm in diameter and 2000 mm in length, compatible with a 0.025/0.035-inch guidewire. The intended electrode can be set as the active electrode in the unipolar, bipolar, or multipolar modes.
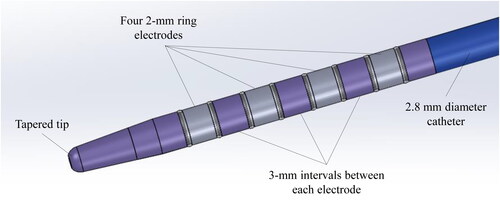
Figure 2. Ingrowth-ablation model. Tissue blocks measuring 50 × 30 × 30 mm3 were sectioned from the bovine livers (A), and a 10-mm diameter columnar structure was hollowed out from the center of the block using a cork borer (B). A 10 mm × 40 mm uncovered metal stent was filled with this columnar tissue, and 0.035-inch guidewire was passed through the center of it, followed by insertion of the ablation catheter over the guidewire (C). Finally, this assembly was refitted into the hollowed-out tunnel in the block (D).

Figure 3. Ingrowth-ablation with stent-wire contact model. Tissue blocks measuring 50 × 30 × 30 mm3 were sectioned from the bovine livers (A), and a 10-mm diameter columnar structure was hollowed out from the center of the block using a cork borer (B). The guidewire and ablation catheter were inserted into the chink between the stent and the columnar tissue structure (creating a situation where the electrodes are in contact with the stent-metal wire) (C), which was refitted into the hollowed-out block (D).

Table 1. Depth of radiofrequency ablation in three types of models.
Figure 4. After ablation, the block was cut longitudinally using a pathology knife to expose the stent. A sufficient ablation effect within the stent can be confirmed in the ingrowth-ablation model (A), while the tissue is hardly ablated in the ingrowth-ablation with stent-wire contact model (B).
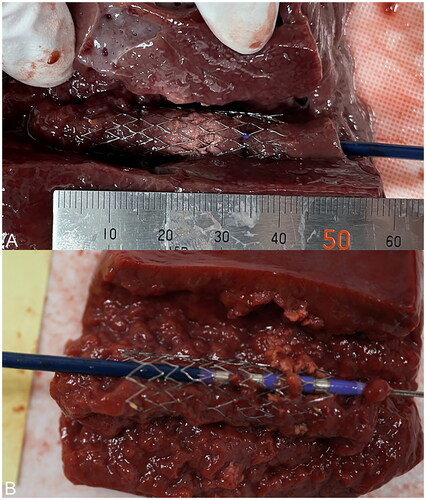
Figure 5. For experiments in the unipolar mode, the median ablation depth of the stent-wire contact model was significantly lower than that of the ingrowth-ablation model (p = 0.005) and the standard-ablation model (p = 0.004). There was no significant difference between the ingrowth-ablation and standard-ablation models (p = 0.563).
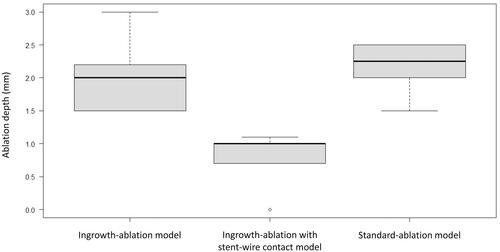
Figure 6. For experiments in the bipolar mode, the median ablation depth of the stent-wire contact model was significantly lower than that of the ingrowth-ablation model (p = 0.008) and the standard-ablation model (p = 0.011), while there was no significant difference between the ingrowth-ablation and standard-ablation models (p = 0.807).