Figures & data
Figure 2. Percutaneous ablation for a subcardiac hepatocellular carcinoma (HCC) with artificial ascites under fusion image guidance. Gadoxetic acid-enhanced axial (A) and coronal (B) hepatobiliary phase MR images displays a 2.0-cm low signal intensity HCC (arrows) abutting the heart in the left lateral section of the liver. (C) Under fusion imaging guidance, three applicators (arrows) are inserted around the target tumor (red cross marker located at the upper margin of the low echoic target tumor). Artificial ascites (arrowheads) in the perihepatic space not only prevents thermal injury to adjacent organs but also helps insert applicators accurately around the target tumor without puncturing the pericardium. (D) Immediate follow-up contrast-enhanced portal venous phase axial CT demonstrates complete destruction of the target lesion with sufficient ablation margin.
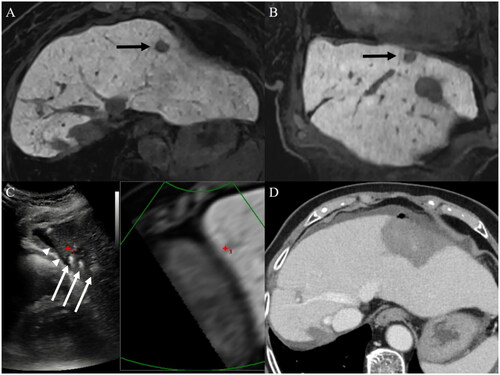
Figure 3. Percutaneous ablation for a subdiaphragmatic hepatocellular carcinoma (HCC) with artificial ascites under fusion image guidance. Contrast-enhanced axial (A) and coronal (B) arterial phase CT images displays a 1.2-cm hypervascular HCC (arrows) abutting the diaphragm in segment VIII of the liver. (C) Fusion imaging technique between real-time working US and reference arterial phase CT images cannot display the target lesion (red cross) due to the lung shadow. (D) After artificial ascites (arrowheads) injection between the diaphragm and liver dome, the target lesion is clearly visualized as a low echoic nodule (red cross) under fusion imaging guidance. (E) After radiofrequency energy delivery, the echo-cloud of micro-bubbles is created around the target lesion. (F) Immediate follow-up contrast-enhanced portal venous phase axial CT demonstrates complete destruction of the target lesion with sufficient ablation margin. (G) There was no local tumor progression at the 32-month follow-up CT.
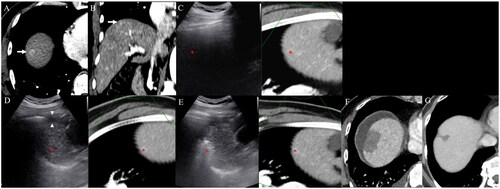
Figure 4. An infeasible case of percutaneous ablation. Gadoxetic acid-enhanced axial (A) and coronal (B) hepatobiliary phase MR images display a 1.6-cm low signal intensity hepatocellular carcinoma (arrows) abutting the right posterior hepatic duct (arrowheads) in the right liver central portion. Ablation was not performed due to a high risk of central bile duct injury.
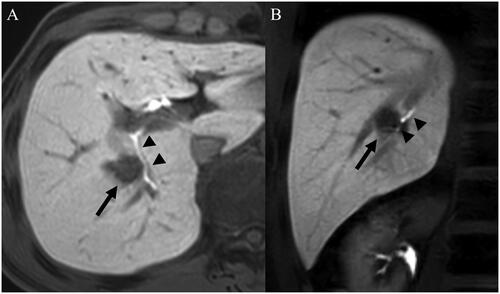
Table 1. Patients characteristics.
Table 2. Comparison of complication rates between difficult location and conventional location groups.
Figure 5. Cumulative incidence estimation of local tumor progression (LTP) and recurrence-free survival (RFS). (A) Cumulative incidence of LTP after ablation in 220 patients in the conventional location group was compared with 211 patients in the difficult location group. (B) Kaplan–Meier estimation of RFS after ablation in 220 patients in the conventional location group was compared with 211 patients in the difficult location group.
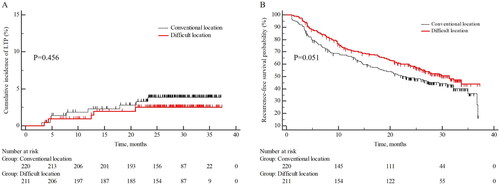
Table 3. Comparison of estimated cumulative incidence of local tumor progression between the difficult location and conventional location groups.
Data availability statement
Raw data were generated at Seoul National University Hospital. Derived data supporting the findings of this study are available from the corresponding author J.M.L. on request.