Figures & data
Figure 1. Schematic diagram of microwave ablation for papillary thyroid microcarcinomas. A. Anatomical structure of the neck; B. Normal saline is injected as a spacer fluid to separate the normal tissues from the ablation area; C. The needle or antenna is inserted into the tumor lesion; D. An extended ablation area is introduced.
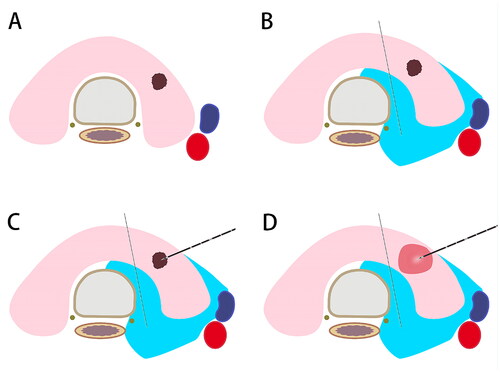
Figure 2. Ultrasonographic imaging of TA. A. Hydrodissection is performed to build up a barrier to protect normal tissues from heat injury; B. The needle or antenna is percutaneously inserted into the PTMC; C. The power turns off with tissue degeneration; D. Contrast-enhanced ultrasonography after ablation with a filling defect. TA, thermal ablation. PTMC, papillary thyroid microcarcinoma.
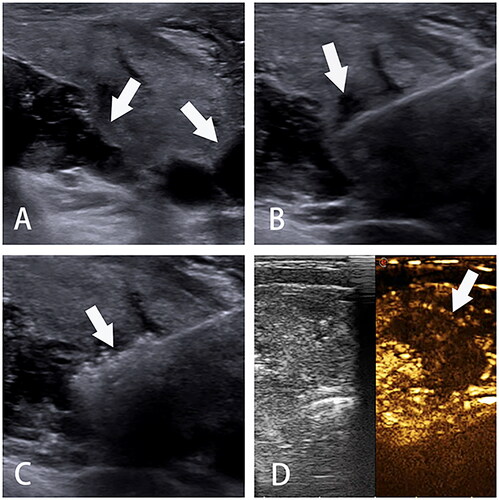
Figure 3. The fixed-needle technique (A) and moving-shot technique (B) adopted to ablate PTMCs and surrounding tissues.
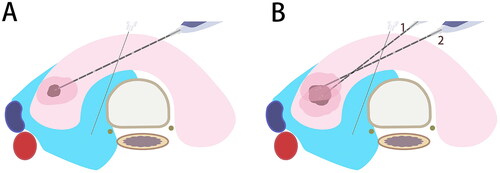
Figure 4. Flow chart for the multidisciplinary management of PTMCs. Surgery is preferred to high-risk PTMCs if feasible; otherwise, they can be managed by as or TA based on patients’ desire, tumor features and medical resources, etc. Surgery is still preferred to PTMC patients with tumor progression or recurrence detected during as after TA. PTMC, papillary thyroid microcarcinoma; as, active surveillance; TA, thermal ablation; MWA, microwave ablation; LA, laser ablation; RFA, radiofrequency ablation.
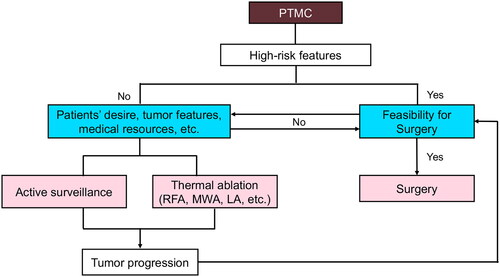
Table 1. Characteristics of selected studies (2018–2023).
Data availability statement
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
