Figures & data
Figure 1. Patient selection flow chart. RFA: radiofrequency ablation, GIST: gastrointestinal stromal tumor.
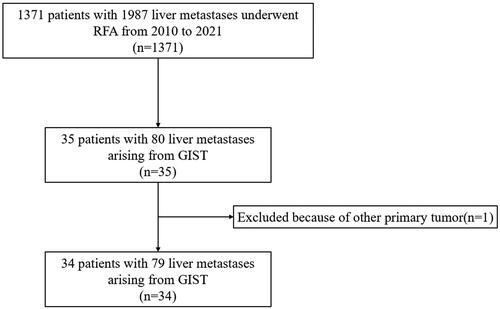
Table 1. The basic characteristics of 34 patients with liver metastasis from GIST.
Figure 3. Hepatic progression-free survival curves for patients with or without TKI therapy before RFA (p = 0.014).
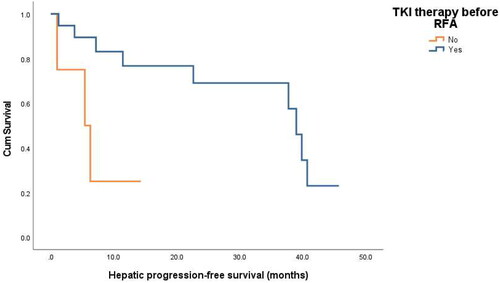
Table 2. Univariable and multivariable analyses of the risk factors for HPFS.
Table 3. Multivariate analysis of HPFS factors with Cox proportional hazards in patients with liver metastasis from GIST after RFA.
Figure 4. Overall survival curves for patients with or without extrahepatic metastasis before RFA (p = 0.044).
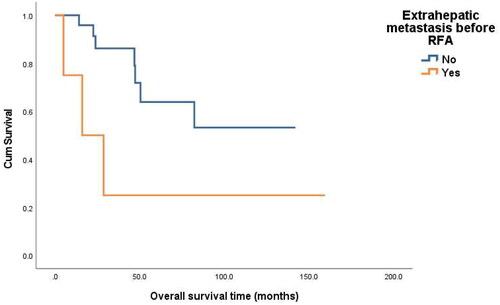
Figure 5. Images from a 60-year-old male with liver metastasis from GIST. (A) Ultrasound before RFA showed a 1.6 cm tumor in liver. (B) Contrast-enhanced ultrasound before RFA showed a 1.8 cm tumor with slight enhancement in liver. (C)MRI showed a 1.8 cm enhanced tumor (arrow) in liver. (D) with ultrasound guidance, two bipolar RFA electrodes (arrow) were inserted into the tumor (E)Contrast-enhanced CT one month after initial RFA showed ablation area showed ablation area had no viability. (F) Contrast-enhanced CT 6 months after initial RFA showed ablation area shrunk without local progression or new liver metastases.
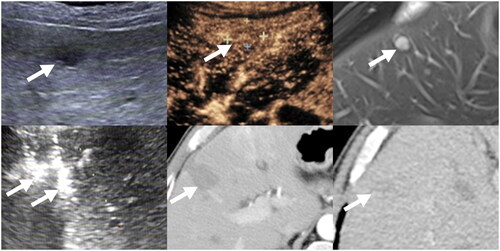
Table 4. Univariable analyses of the risk factors for OS.
Table 5. Multivariate analysis of OS factors with Cox proportional hazards in patients with liver metastasis from GIST after RFA.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.