Figures & data
Figure 1. The Knowledge-to-Action Framework (Citation8). The Knowledge-to-Action Framework involves 2 main components: 1) Knowledge Creation and 2) the Action Cycle. Knowledge Creation is represented by a funnel that illustrates the process by which knowledge becomes more refined and, presumably, more useful over time. The Action Cycle refers to the actions necessary to drive the changes in practice that result from application of new knowledge (Citation8). The first step of the Action Cycle is to identify the problem and review knowledge, and this is the part of the cycle addressed in this report. Reprinted with permission from Wolters Kluwer Health, Inc (Citation8). https://journals.lww.com/jcehp/Abstract/2006/26010/Lost_in_knowledge_translation__Time_for_a_map_.3.aspx.
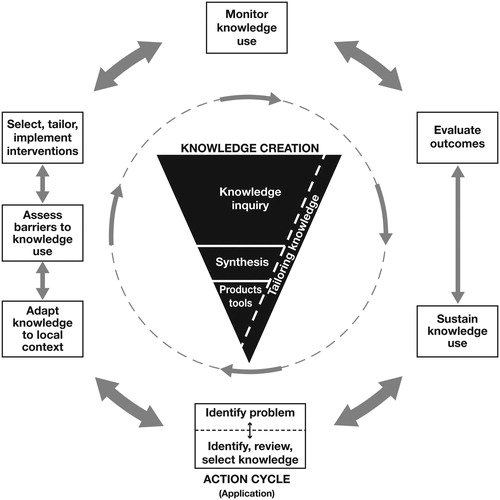
Figure 2. Frequency of challenges to provision of optimal care for patients with severe asthma. A) The types of challenges and the frequency with which providers experience themc for all respondents. B) Challenges “often” or “always” faced by respondents by practice type are shown. AMC, academic medical center; CB, community-based. ap < 0.0001 across all 4 challenges. bComparisons were made for AMC and CB practitioners for each of the 4 individual challenges using chi-square to evaluate 2 × 2 frequency tables displaying Frequency of Physician Practice Setting × Difficulty, where Difficulty was dichotomously categorized as Often/Always a Challenge (response of 2 or 3) vs. Not Often/Always a Challenge (response of 0 or 1); however, none of these associations were significant. cSurvey respondents were asked: “What challenges do you face in providing optimal care for your patients with severe, uncontrolled asthma?” Response choices were “never,” “sometimes,” “often,” or “always.” p-values are determined using a chi-squared test for the percentage of respondents who “never” or “sometimes” compared with “often” or “always” face particular challenges.
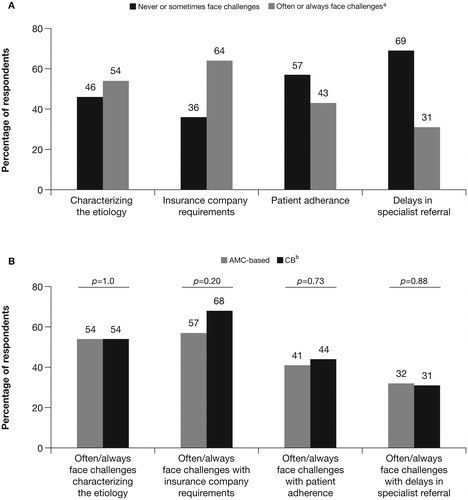
Figure 3. Factors considered in making therapy decisions. The importance of each factor in making decisions about therapya was ranked by A) all respondents and B) respondents separated by practice type.b AMC, academic medical center; CB, community-based; ED, emergency department; EOS, eosinophils; FeNO, fractional exhaled nitric oxide; IgE, immunoglobulin E; OCS, oral corticosteroids; RAST, radioallergosorbent test. aSurvey respondents were asked: “When determining therapy for patients with severe, uncontrolled asthma, please rate the degree to which you take into consideration each of the following parameters.” Response choices were 0–5 (0 = minimally important; 5 = highly important). bp-values are determined using a chi-squared test for the percentage of respondents who rate each factor with a score of 4–5 compared with 0–3 between practice types. The dichotomization for the degree of consideration for each parameter was tested via chi-square for association with practice type (CB vs. AMC), traditional measures of morbidity vs. biomarkers.
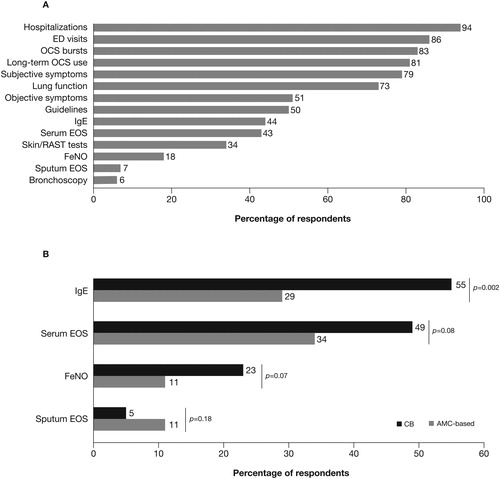
Figure 4. Characterization of resources necessary for optimal management of severe asthma.b The percentages of A) all respondents and B) respondents by practice typec who considered each resource necessary for severe asthma management are shown. AMC, academic medical center; CB, community-based. ap < 0.0001 across all 4 resources. bSurvey respondents were asked: “What resources do you believe are important for you to optimally manage your patients with severe, uncontrolled asthma?” Response choices were: “necessary and use,” “necessary but don't have,“ “might use but don't have,” and “don't need.” cp-values are determined using a chi-squared test for the percentage of respondents who rate each factor as “necessary and use” compared with “necessary/might use but don't have” (which is the result of combining the “necessary but don't have” and the “might use but don't have” response options) between practice types.
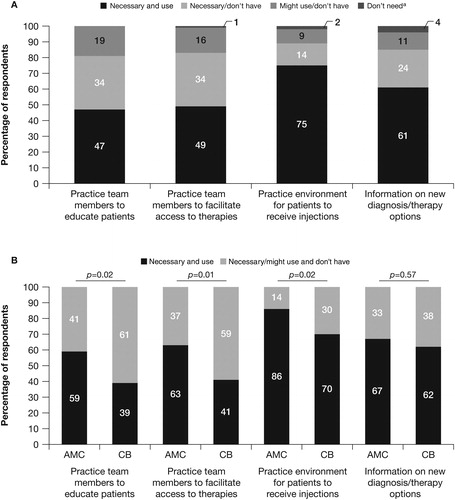
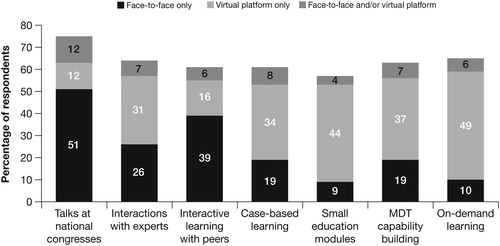
Figure 5. Value of different types of educational opportunities and formats.a,b The percentages of respondents who preferred each type of format for each educational opportunity are shown. AMC, academic medical center; CB, community-based; MDT, multidisciplinary team. aSurvey respondents were asked: “How valuable are each of the following educational opportunities/formats to assist you in effectively managing your patients with severe, uncontrolled asthma?” Response choices were “face-to-face only,” “virtual platform only,” and “face-to-face and/or virtual platform.” Responses were dichotomized into face-to-face or virtual (combining “highly valuable face-to-face” and “highly valuable virtually”) and neither/none (combining “somewhat valuable ± virtual access” and “of no value to me”), and chi-square was used to test the association with practice type (AMC or CB). No significant associations were found. This figure shows simple percentages of respondents. bBars did not total 100% because some respondents selected that these educational opportunities were “of no benefit to me.”