Figures & data
Table 1. Patient characteristics of 73 patients with locally advanced primary or recurrent rectal and sigmoid cancer with high risk of R1 resection treated with pulsed dose rate brachytherapy.
Table 2. Treatment characteristics for 73 patients with locally advanced primary or recurrent rectal and sigmoid cancer with high risk of R1 resection treated with external beam radiotherapy, extensive surgery and pulsed dose rate brachytherapy.
Figure 1. Postoperative interstitial pulsed dose rate brachytherapy (PDR-BT) in a patient with locally recurrent rectal cancer with high risk of R1 resection. (a) Catheters for brachytherapy sutured to the tumour bed. The catheters were later covered by a pediculated myocutaneous flap (rectus abdominis) preventing direct contact between the intestines and the high dose volume. (b) Treatment plan delivering 30 Gy (cyan contour) given with 0.6 Gy per pulse, one pulse per hour to the BT target (red contour). Dose planning was conducted with manual dose optimisation avoiding overlap of double dose volumes i.e., 60 Gy (yellow contour).
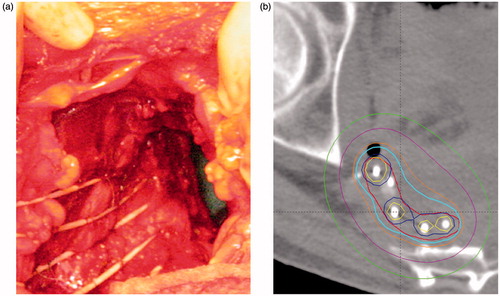
Figure 2. Clinical outcome in 73 patients with locally advanced primary or recurrent rectal and sigmoid cancer with high risk of R1 resection treated with pulsed dose rate brachytherapy (PDR-BT). (a) Local control (LC) and overall survival (OS) of the entire group. (b) Local control related to the number of catheters used for brachytherapy. (c) Local control in relation to resection margin (R-stage). (d) Freedom from Grade 3, 4 and 5 overall and specific brachytherapy-related morbidity ().
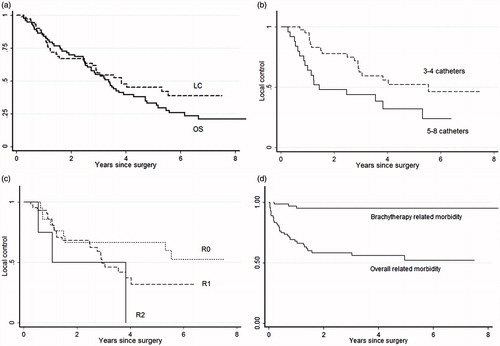
Table 3. Early (within 90 days) and late complications (>90 days) retrospectively scored according to CTCv3.0 in 73 patients with locally advanced primary or recurrent rectal and sigmoid cancer with high risk of R1 resection treated with external beam radiotherapy, extensive surgery and pulsed dose rate brachytherapy.
