Figures & data
Figure 2. Patients referred for electrochemotherapy present with different clinical stages of cutaneous metastasis. Evaluation of smaller tumours may favourably be performed using digital photography and ruler (top panel, from [Citation36]). For larger tumours, imaging such as PET/CT can be very valuable in determining response (bottom panel, from [Citation9]).
![Figure 2. Patients referred for electrochemotherapy present with different clinical stages of cutaneous metastasis. Evaluation of smaller tumours may favourably be performed using digital photography and ruler (top panel, from [Citation36]). For larger tumours, imaging such as PET/CT can be very valuable in determining response (bottom panel, from [Citation9]).](/cms/asset/b73d2438-41fb-4803-b070-d3f683dca59d/ionc_a_1454602_f0002_c.jpg)
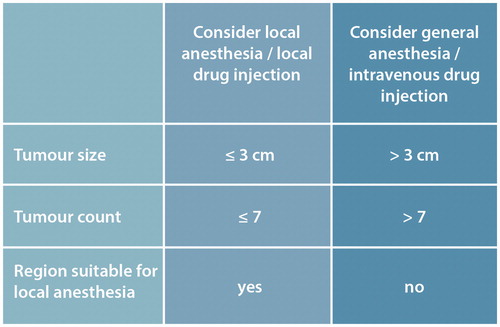
Figure 3. Intratumoural treatment using bleomycin. Volumes for smaller tumours are relatively larger, to compensate for loss to the systemic circulation when the injected volume is small.
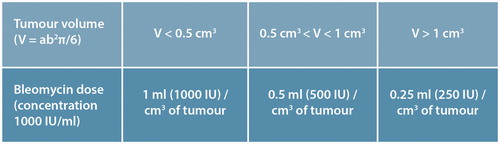
Figure 4. Different electrodes suit different clinical challenges. Top left; linear array electrode, ideal for smaller tumours. Due to the relatively lower applied voltage (due to small electrode distance), ideal for treatment in local anaesthesia. Hyperpigmentation using this electrode is very little to negligible, and this electrode is thus recommended for use in the facial region. Top right; hexagonal electrode. This electrode should only be used under general anaesthesia, and will often cause hyperpigmentation. The relatively larger area covered allows larger tumours to be treated, making this electrode a good choice for large cutaneous metastases, e.g., chest wall recurrence after breast cancer. Middle left panel; plate electrodes, may be used for exophytic tumours. Middle right panel; finger electrodes, may be used for mucosal tumours in e.g., the oral cavity. Bottom; Adjustable electrodes allow better support for the needles, and allows adjustment for tumours with heterogeneous size.
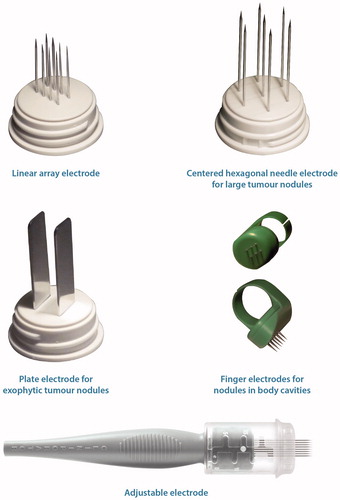
Figure 5. Carrying out treatment. Electrochemotherapy is performed under analgesia; for smaller tumours local anaesthesia (as indicated here) whereas larger tumor conglomerates necessitate general anaesthesia. The chemotherapeutic agent, bleomycin, is either injected locally (few, small tumours), or systemically for large and/or many tumours. After drug administration the electric pulses are administered through the electrodes that are inserted into the tumour tissue. The electrodes are systematically moved, and pulses applied again, in order to cover the entire tumour area. The pulsing sequence is very brief, and therefore even large tumours may be covered in the course of a single treatment because the procedure proceeds quickly.
Figure 6. Pain management plan. Most patients treated with electrochemotherapy only experience no or limited pain after treatment. A subset of patients do, however, experience pain and these patients may be predicted from their pain score before treatment [Citation33], i.e., at the pre-treatment visit. Based on patient pain score (NRS = numeric rating scale, where 0 is no pain at all, and 10 is the worst pain imaginable), the patient may be assessed at the pre-treatment visit for a pain management plan. Other factors that may forewarn higher risk of post-procedure pain are previous irradiation and large tumours [Citation33].
![Figure 6. Pain management plan. Most patients treated with electrochemotherapy only experience no or limited pain after treatment. A subset of patients do, however, experience pain and these patients may be predicted from their pain score before treatment [Citation33], i.e., at the pre-treatment visit. Based on patient pain score (NRS = numeric rating scale, where 0 is no pain at all, and 10 is the worst pain imaginable), the patient may be assessed at the pre-treatment visit for a pain management plan. Other factors that may forewarn higher risk of post-procedure pain are previous irradiation and large tumours [Citation33].](/cms/asset/a7d68f7a-b473-43e4-a9df-a9489ac651ae/ionc_a_1454602_f0006_c.jpg)