Figures & data
Figure 1. Percentage of patients with ILDs diagnosed by different clinical specialties. Data from online survey of physicians (pulmonologists, n = 243; rheumatologists, n = 203; internists, n = 40). Survey question: “What percentage of patients with the following types of ILDs are diagnosed by the following specialties?” Examples of autoimmune ILDs provided to physicians participating in the survey were RA-ILD, SSc-ILD and other CTD-ILDs. Examples of non-IPF non-autoimmune ILDs provided were iNSIP, HP and sarcoidosis-ILD. Rheumatologists were only asked this question in relation to autoimmune ILDs. Abbreviations. CTD, Connective tissue disease; HP, Hypersensitivity pneumonitis; ILD, Interstitial lung disease; iNSIP, Idiopathic non-specific interstitial pneumonia; IPF, Idiopathic pulmonary fibrosis; RA, Rheumatoid arthritis; SSc, Systemic sclerosis.
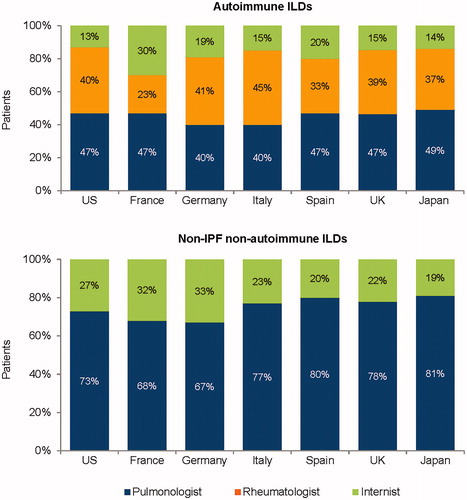
Figure 2. Patient journey in non-IPF progressive fibrosing ILDs. Data from online survey of physicians (pulmonologists, n = 243; rheumatologists, n = 203; internists, n = 40). Survey question: “Please estimate the average duration of the following for the different ILDs: time from symptom onset to diagnosis of ILD; time from diagnosis of ILD to development of ILD that is fibrotic and progressing; time from development of ILD that is fibrotic and progressing to point where fibrotic and progressing ILD is detected by physician; time from point where fibrotic and progressing ILD is detected by physician to patient death”. Rheumatologists were only asked this question in relation to RA-ILD, SSc-ILD and other CTD-ILDs. Abbreviations. CTD, Connective tissue disease; HP, Hypersensitivity pneumonitis; IIP, Idiopathic interstitial pneumonias; ILD, Interstitial lung disease; iNSIP, Idiopathic non-specific interstitial pneumonia; IPF, Idiopathic pulmonary fibrosis; RA, Rheumatoid arthritis; SSc, Systemic sclerosis.
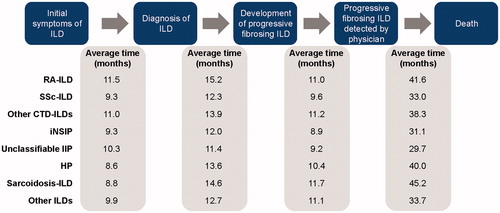
Figure 3. Frequency of pulmonary function tests in patients with ILDs. Data from online survey of physicians (pulmonologists, n = 243; rheumatologists, n = 203; internists, n = 40). Survey question: “In patients with ILD where you manage/help manage the ILD, on average how frequently do you check the status of the patients’ ILD based on pulmonary function tests (e.g. FVC, DLCO, 6-minute walk)?” Abbreviations. DLCO, Diffusing capacity of the lungs for carbon monoxide; FVC, Forced vital capacity; ILD, Interstitial lung disease.
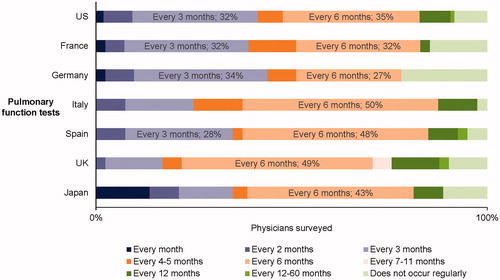
Table 1. Percentage of US patients who received treatment for non-IPF ILDs in 2016.
Figure 4. Percentage of patients with non-IPF ILDs who develop a progressive fibrosing phenotype. Data from online survey of physicians (pulmonologists, n = 243; rheumatologists, n = 203; internists, n = 40). Survey question: “For each of the ILD types listed below, among the patients you have seen in the past year, please estimate what percentage of patients had an ILD that (1) had fibrosis detected by HRCT (i.e. reticular abnormality with traction bronchiectasis with or without honeycombing) AND (2) was progressing in terms of worsening of lung function (FVC and/or DLCO) and/or respiratory symptoms and/or chest images”. Rheumatologists were only asked this question in relation to RA-ILD, SSc-ILD and other CTD-ILDs. Abbreviations. CTD, Connective tissue disease; DLCO, Diffusing capacity of the lungs for carbon monoxide; FVC, Forced vital capacity; HP, Hypersensitivity pneumonitis; HRCT, High-resolution computed tomography; IIP, Idiopathic interstitial pneumonias; ILD, Interstitial lung disease; iNSIP, Idiopathic non-specific interstitial pneumonia; IPF, Idiopathic pulmonary fibrosis; RA, Rheumatoid arthritis; SSc, Systemic sclerosis.
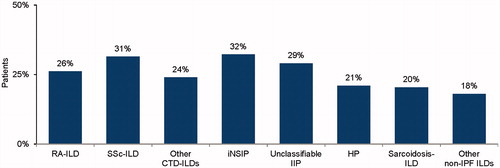
Figure 5. Percentage of patients who received treatment for non-IPF progressive fibrosing ILDs in the past year. Data from online survey of physicians (pulmonologists, n = 243; rheumatologists, n = 203; internists, n = 40). Survey question: “For all non-IPF ILD patients you manage that have fibrosis and progressive disease, what percentage received drug treatment for their ILD in the past year? Examples of treatments include corticosteroids, azathioprine, or other immunosuppressants aimed at treating the ILD”. Rheumatologists were only asked this question in relation to RA-ILD, SSc-ILD and other CTD-ILDs. Abbreviations. CTD, Connective tissue disease; HP, Hypersensitivity pneumonitis; IIP, Idiopathic interstitial pneumonias; ILD, Interstitial lung disease; iNSIP, Idiopathic non-specific interstitial pneumonia; IPF, Idiopathic pulmonary fibrosis; RA, Rheumatoid arthritis; SSc, Systemic sclerosis.
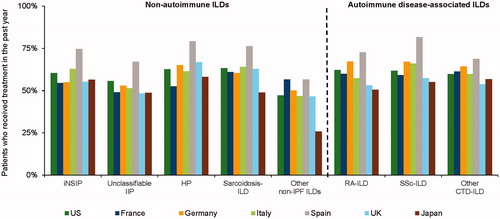
Figure 6. Reasons why patients with non-IPF progressive fibrosing ILDs did not receive treatment. Data from online survey of physicians (pulmonologists, n = 243; rheumatologists, n = 203). Survey question: “In the previous question, you indicated that some ILD patients that have fibrosis and progressive disease did not receive drug treatment for their ILD in the past year. What are the primary reasons why these patients did not take a therapy?” Abbreviations. ILD, Interstitial lung disease; IPF, Idiopathic pulmonary fibrosis.
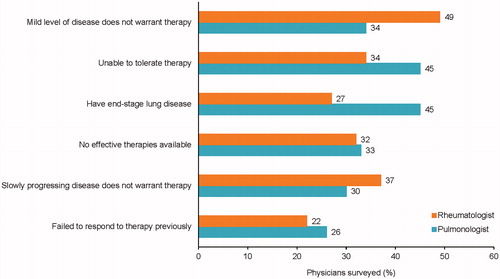
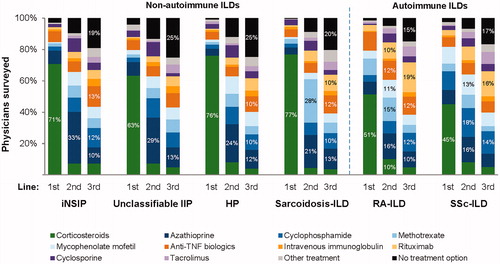
Figure 7. Agents used as first-, second- and third-line treatments for fibrotic ILDs. Data from online survey of physicians (non-autoimmune ILDs: 243 pulmonologists; autoimmune ILDs: 243 pulmonologists and 203 rheumatologists). Survey question: “For the following types of ILDs where patients also have lung fibrosis, please indicate your preferred first, second, and third line treatments for the respective ILD”. Rheumatologists were only asked this question in relation to RA-ILD and SSc-ILD. Abbreviations. HP, Hypersensitivity pneumonitis; IIP, Idiopathic interstitial pneumonias; ILD, Interstitial lung disease; iNSIP, Idiopathic non-specific interstitial pneumonia; RA, Rheumatoid arthritis; SSc, Systemic sclerosis.
Supplemental Material
Download MS Word (488.9 KB)Data availability statement
The datasets used and/or analyzed during the current study are not publicly available but are available from Boehringer Ingelheim on reasonable request.
