Figures & data
Table 1. Indications for preoperative treatment in rectal cancer according to pretreatment characteristics defined by pelvic magnetic resonance imaging.Table Footnotea,Table Footnotee
Figure 1. Proportion of patients receiving short-course radiotherapy (scRT) with a delay to surgery >3 weeks rather than immediate surgery in six health care regions in Sweden 2009–2014. The Stockholm/Gotland and Uppsala/Örebro regions participated in the Stockholm III trial (Citation47) where patients could be randomized to delayed surgery. However, the number of randomized patients was far less than the number of patients treated with a delay, and, furthermore, randomization stopped in January 2014 but a delay continued to be used. A delay was used also in other regions but one during the latter part of the time period for patients below 75 years (A). Several patients above 75 years had surgery delayed, with no real change during the time period (B).
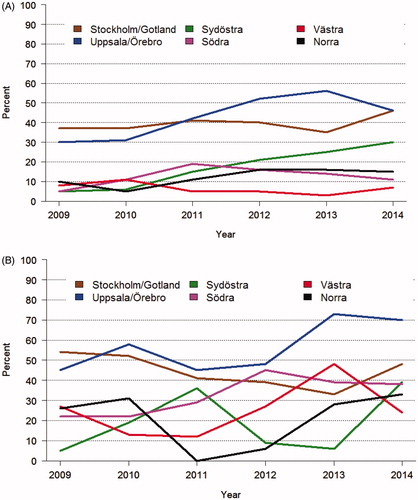
Figure 2. Time in weeks for patients treated in Sweden 1995–2014 with short-course radiotherapy (scRT) and a delay to surgery (>3 weeks). When a delay started to be used in 1999, the time when the Stockholm III trial (Citation47) started, the delay was usually 4–6 weeks. After a few years, a delay of 6–8 weeks or longer became more common, and during the last years it was above 8 weeks in the majority of the patients.
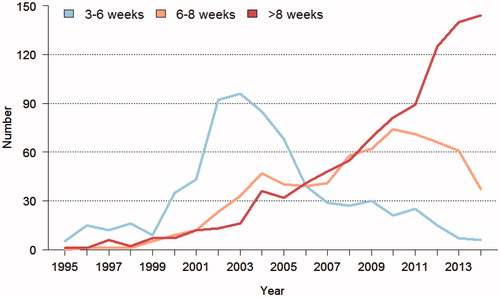
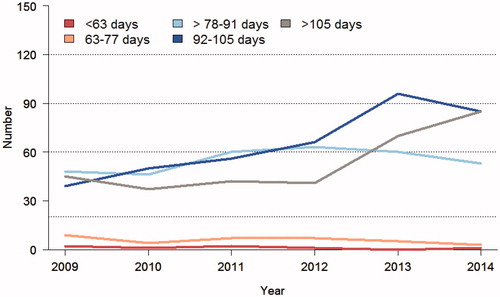
Figure 3. Time from start of chemoradiotherapy (50–50.4 Gy in 25–28 fractions during 5–5.5 weeks with capecitabine) in Sweden 2009–2014. In 2009 an equal number of patients had a delay after the last radiation fraction of 6–8 weeks (78–91 days), 8–10 weeks (92–105 days), and >10 weeks (>105 days). The number of patients with the longest delay was stable until 2012, after which time it increased and was more common than 8–10 weeks during 2014. During the entire time period, a delay of 6–8 weeks has been recommended. This is also recommended in the latest version from 2016 of the national care programme.
Bengt Glimelius, winner of the Rudbeck award 2016, at the Medical Faculty of Uppsala University for his elaborative studies of colorectal cancers the results of which have been of utmost importance for patients with this devastating disease.

