Figures & data
Table 1. Baseline characteristics of the REBUS population and pharmaceutical treatment at hospital discharge. Results describe number of patients (proportion) unless stated otherwise.
Table 2. D-dimer concentrations, thrombin peak concentrations, and ETP given as median (interquartile range).
Table 3. Biomarkers at early follow-up (2–3 weeks after discharge) in relation to baseline characteristics and pharmaceutical treatment at hospital discharge after index event.
Figure 2. Kaplan–Meier estimate for (upper panel) the composite endpoint of all-cause mortality, new myocardial infarction, congestive heart failure, and all-cause stroke; and (lower panel) clinically relevant bleeding events by D-dimer concentration tertiles.
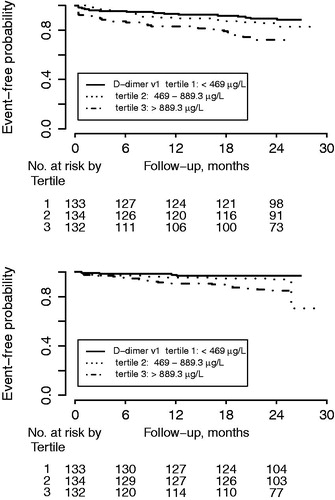
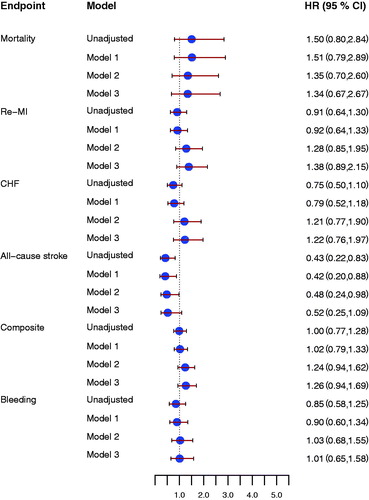
Figure 3. Forrest plot for the effect of D-dimer concentrations at early follow-up for prediction of all-cause mortality, new myocardial infarction (re-MI), congestive heart failure (CHF), all-cause stroke, the composite endpoint, and clinically relevant bleeding event (Bleeding), unadjusted and after adjustment. Model 1 included adjustment for age, sex, hypertension, diabetes, atrial fibrillation, previous congestive heart failure, NSTEMI/STEMI as index event. Model 2 included antithrombotic treatment: aspirin, ADP receptor-blocking agent, and oral anticoagulant treatment at inclusion and at the early follow-up visit. Model 3 included model 1 and model 2. All hazard ratios reflect the effect of a one standard deviation increase.
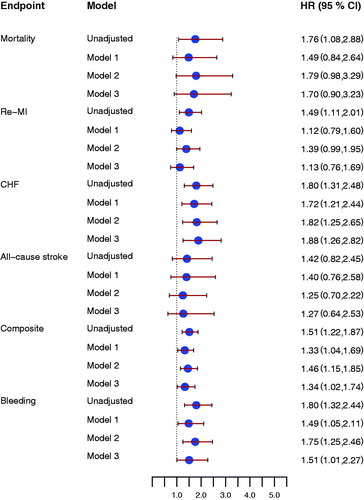
Figure 4. Forrest plot for the effect of thrombin peak at early follow-up for prediction of all-cause mortality, new myocardial infarction (re-MI), congestive heart failure (CHF), all-cause stroke, the composite endpoint, and clinically relevant bleeding event (Bleeding), unadjusted and after adjustment. Model 1 included adjustment for age, sex, hypertension, diabetes, atrial fibrillation, previous congestive heart failure, NSTEMI/STEMI as index event. Model 2 included antithrombotic treatment: aspirin, ADP-receptor blocking agent, and oral anticoagulant treatment at inclusion and at the early follow up visit. Model 3 included model 1 and model 2. All hazard ratios reflect the effect of a one standard deviation increase.
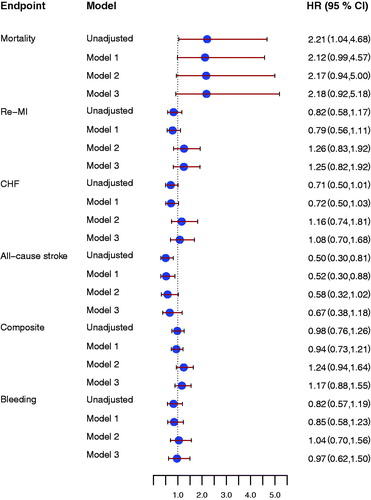
Figure 5. Forrest plot for the effect of endogenous thrombin potential (ETP) at early follow-up for prediction of all-cause mortality, new myocardial infarction (re-MI), congestive heart failure (CHF), all-cause stroke, the composite endpoint and clinically relevant bleeding event (Bleeding), unadjusted and after adjustment. Model 1 included adjustment for age, sex, hypertension, diabetes, atrial fibrillation, previous congestive heart failure, NSTEMI/STEMI as index event. Model 2 included antithrombotic treatment: aspirin, ADP receptor-blocking agent, and oral anticoagulant treatment at inclusion and at the early follow-up visit. Model 3 included model 1 and model 2. All hazard ratios reflect the effect of a one standard deviation increase.