Figures & data
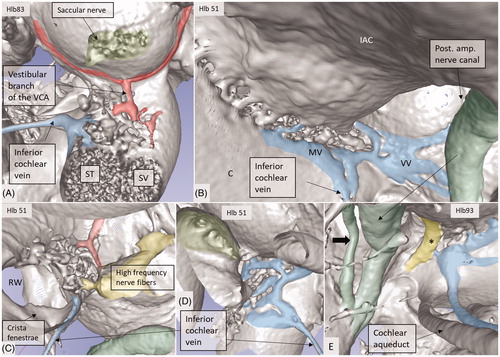
Figure 1. Micro-CT and volume rendering of a plastic corrosion cast of a left human temporal bone. The VA and CA (yellow) with their accessory canals (blue) are seen (arrows). They drain blood from the inner ear and are shown in higher magnification in B and C. *carotid artery; JB: jugular bulb; RW: round window; SS: sigmoid sinus.
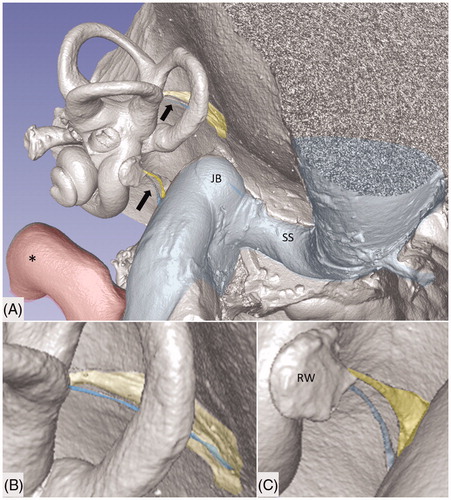
Figure 2. Principal vascular anatomy of the human inner ear by Nabeya (Citation42).
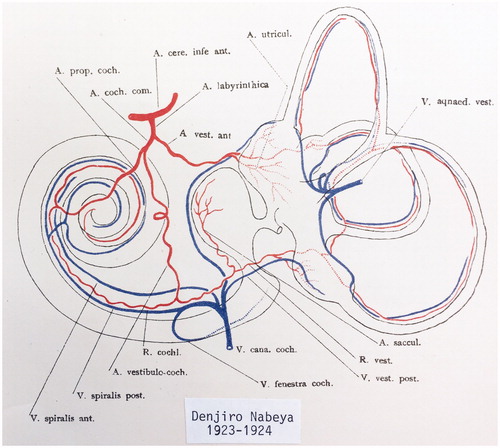
Figure 3. (A) Plastic corrosion cast of a left human cochlea. Radiating arterioles of the basal turn of the cochlea can be observed. The route for electrode insertion at the CI is shown in green at arrow. (B) Micro-CT and 3D rendering of a plastic mold from a left human temporal bone (medial view). The level of cropping is shown (interrupted line). The inferior cochlear vein channel is seen (blue), as well as the cochlear aqueduct. The vein drains blood from the cochlea and runs parallel to the cochlear aqueduct. C: cochlea; CI: cochlear implantation; IAC: internal acoustic canal.
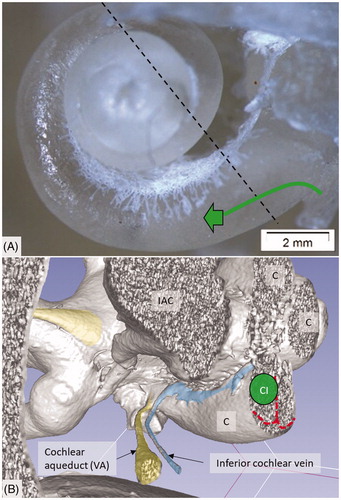
Figure 4. Micro-CT and 3D rendering with surface enhancement of the inner labyrinth in a right macerated human temporal bone. (A) The tractus spiralis arteriosus (red) supplying the SV with radiating arterioles is seen (Roman numerals represent cochlear turns). The VCA branches into the vestibular and cochlear branches which run in opposite directions. (B) The cochlear branch runs spirally and anastomoses with the CA (blue arrow) at the upper segment of the first cochlear turn. The size and anatomy vary greatly among different temporal bones. (C and D) Anastomosis shown between the cochlear branch of the CVA and the CA. Several tributaries project into the modiolus, supplying the spiral ganglion and spiral lamina.
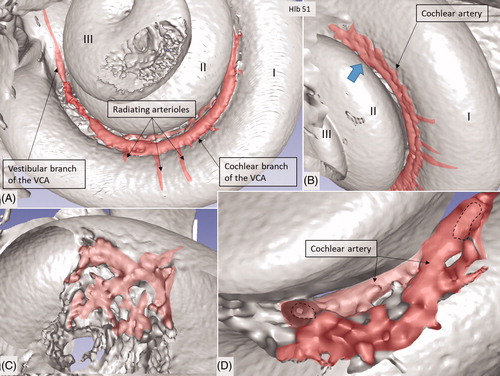
Figure 5. SR-PCI image of a left human cochlea. (A) The tractus spiralis arteriosus is seen between the first and second turn (lower inset). The draining inferior cochlear vein is identified with the merging modiolar spiral veins. (B) The soft tissues in the IAC (yellow) and the inferior cochlear vein are reproduced (blue). The entrances of the VCA and CA can be traced. Note that the VCA crosses through a structurally modified channel.
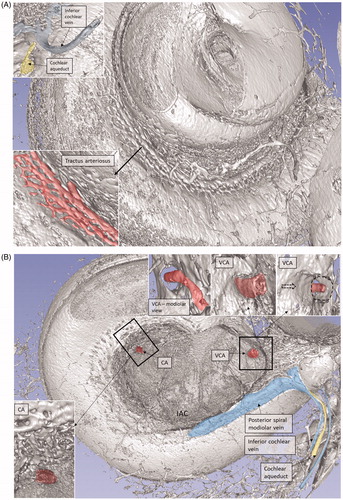
Figure 6. SR-PCI image of a right human cochlea. The VCA was segmented and is shown in higher magnification in the inset. After entry into the modiolus, it divides into several small arteries or plexus.
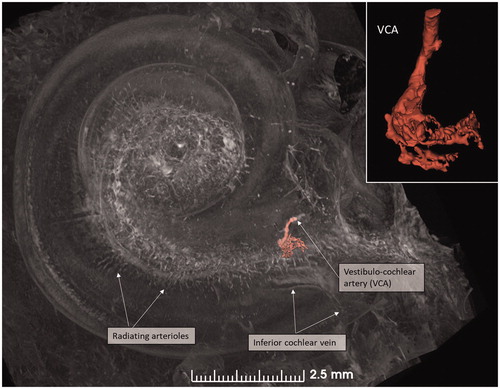
Figure 7. (A) Micro-CT of a right cochlea showing the VCA dividing into vestibular and cochlear branches running in opposite directions. The framed area is magnified in the inset. (B) The VCA is traced in the IAC using a red marker. SNC: saccular nerve canal; UNC: utricle nerve canal.
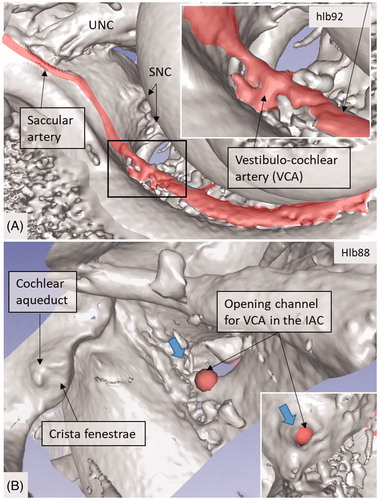
Figure 8. 3D view of a cropped human cochlea at the level of IAC. Removal of bone and surface enhancement reveal vascular structures and nerve canals. The basal turn is sectioned horizontally near the RW. The cochlear aqueduct and inferior cochlear vein are seen. A radiating arteriole is identified and can be followed to the main stem of the cochlear branch of the VCA. The VCA is smaller than usual, suggesting that the main arterial supply to the basal turn is through the CA. C: cochlea.
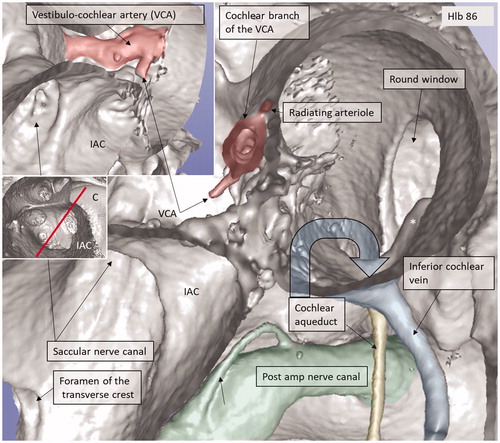
Figure 9. Micro-CT and 3D rendering of a left human temporal bone after virtual molding of the labyrinth using surface enhancement and medial cropping. The technique allows visualization of the labyrinthine cavities. Medial 3D view of a cropped human labyrinth at the level of IAC. The removal of bone reveals openings of the nerve canals in the fundus, as well as the medial surface of the vestibule (V) with common crus (CC), anterior ampulla (Ant amp), and the posterior ampulla (Post amp), together with the vestibular aqueduct (VA) and the vein of the VA. Note the impression of the facial nerve canal caused by the cochlea (red arrows). The inferior cochlear vein can be seen. The foramen of the TC (upper red circle) and the region for the entrance of the VCA (lower red circle) can be seen.
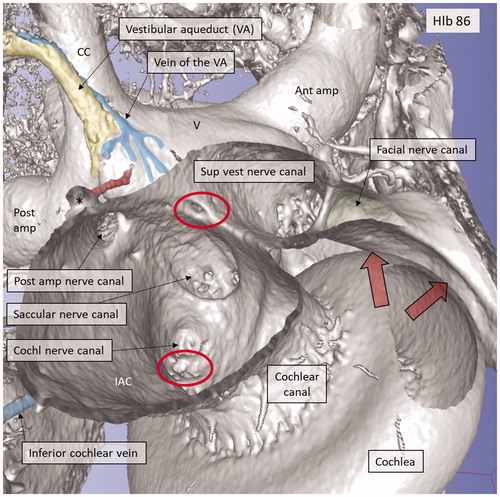
Figure 10. Micro-CT and 3D rendering of a left human temporal bone after virtual molding of the labyrinth using surface enhancement and coronal cropping. (A) The 3D view of a cropped human labyrinth at the level of IAC. The removal of bone and surface enhancement reveal both vascular structures and nerve canals. The cochlear aqueduct and the inferior cochlear vein can be seen. (B) The cochlea is sectioned horizontally near the foramen of the TC (red circle). This channel seems to house a vessel or artery which supplies both the utricle and the saccule. Framed area is shown in higher magnification in (D). (C): Lateral view of the IAC showing the channel of the TC (red). The VA and the accessory canal housing the vein of the VA are identified. CNC: cochlear nerve canal; CC: common crus; S: saccule; TC: transverse crest; U: utricle; *accessory singular nerve canal.
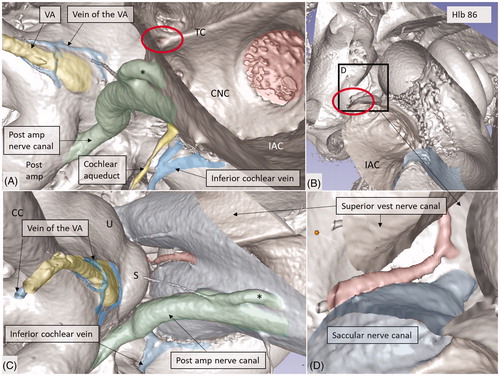
Figure 11. Micro-CT and 3D rendering show anatomic variations of the inferior cochlear vein. (A) Medial view of the basal turn and saccule after cropping. Note the close relationship between the artery and veins. ST: scala tympani; SV: scala vestibuli. (B) Inferior view of the C and IAC. Modiolar veins (MVs) and vestibular veins (VVs) coalesce and drain into the inferior cochlear vein. (C) The inferior cochlear veins run in the floor of the ST near the opening of the cochlear aqueduct and the RW. A channel housing the high-frequency nerve fibers can be seen. (D) Veins draining in the base of the C. Entrance of the saccular nerves are stained green. (E) The relationship between the inferior cochlear vein (blue) and the channel for the high-frequency nerve fibers (*) are seen.