Figures & data
Figure 1. Flowchart depicting the cohort study with nested case-control analysis study design. EMR: electronic medical record; GIB: gastrointestinal bleed; HES: hospital episode statistics; LGIB: lower gastrointestinal bleed; PCP: primary care practitioner; UGIB: upper gastrointestinal bleed; THIN: The Health Improvement Network.
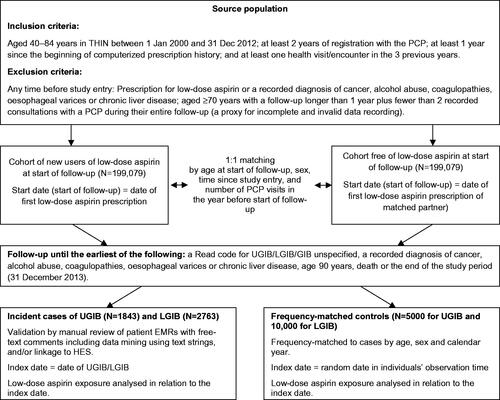
Figure 2. Odds ratio (95% CI) for the associations between morbidities and medications and the risk of UGIB (nested case-control analysis). CI: confidence interval; eGFR: estimated glomerular filtration rate; GERD: gastro-oesophageal reflux disease; H2RA: histamine H2-receptor antagonist; IBD: inflammatory bowel disease; IBS: irritable bowel syndrome; lower gastrointestinal bleed; OR: odds ratio; NSAID: non-steroidal anti-inflammatory drugs; PPI: proton pump inhibitors; PU: peptic ulcer; SSRI: selective serotonin reuptake inhibitors; relative risk; UGIB: upper gastrointestinal bleed. *Adjusted by age, sex, calendar year, number of PCP visits in the year before the index date, smoking, alcohol consumption, prior UGIB, prior LGIB, prior GIB unspecified, pancreatic disease, uncomplicated peptic ulcer, polypharmacy, use of NSAIDs, PPIs, clopidogrel and warfarin. Peptic ulcer complicated were events that presented with haematemesis and/or perforation, unlike peptic ulcer uncomplicated events.
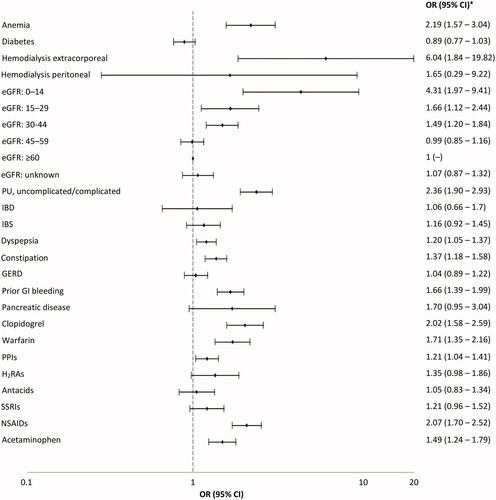
Figure 3. Odds ratio (95% CI) for the associations between morbidities and medications and the risk of LGIB (nested case-control analysis). CI: confidence interval; eGFR: estimated glomerular filtration rate; GERD: gastro-oesophageal reflux disease; H2RA: histamine H2-receptor antagonist; IBD: inflammatory bowel disease; IBS: irritable bowel syndrome; lower gastrointestinal bleed; OR: odds ratio; NSAID: non-steroidal anti-inflammatory drugs; PPI: proton pump inhibitors; PU: peptic ulcer; SSRI: selective serotonin reuptake inhibitors; relative risk; UGIB: upper gastrointestinal bleed. *Adjusted by age, sex, calendar year, number of PCP visits in the year before the index date, smoking, alcohol consumption, BMI, history of polyps, history of LGIB, history of unspecified GIB, PU diseases (complicated and uncomplicated), GERD, IBD, IBS, polypharmacy, use of NSAIDs, PPIs, clopidogrel and warfarin and low-dose aspirin. Peptic ulcer complicated were events that presented with haematemesis and/or perforation, unlike peptic ulcer uncomplicated events.
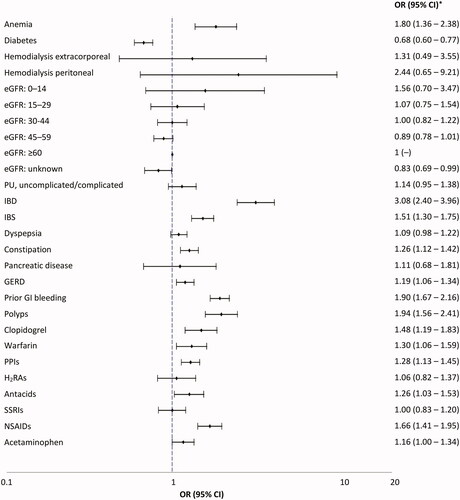
Table 1. ORs (95% CI) for the association between recency, dose and duration of low-dose aspirin and risk of UGIB.
Table 2. RRs (95% CI) for the association between recency, dose and duration of low-dose aspirin and risk of LGIB.
Figure 4. Odds ratio (95% CI) for the association between current use of low-dose aspirin (current use ≤30 days vs. non-use [no use in the 365 days before the index date]) and risk of UGIB/LGIB stratified by primary/secondary CVD prevention population. CI: confidence interval; CVD: cardiovascular; LGIB: lower gastrointestinal bleed; OR: odds ratio; UGIB: upper gastrointestinal.
![Figure 4. Odds ratio (95% CI) for the association between current use of low-dose aspirin (current use ≤30 days vs. non-use [no use in the 365 days before the index date]) and risk of UGIB/LGIB stratified by primary/secondary CVD prevention population. CI: confidence interval; CVD: cardiovascular; LGIB: lower gastrointestinal bleed; OR: odds ratio; UGIB: upper gastrointestinal.](/cms/asset/9bc8ff2b-c6f4-4448-be9e-4a2ea1cc94cf/iann_a_1591635_f0004_b.jpg)
Figure 5. Odds ratio (95% CI) for the association between current use of low-dose aspirin (vs. non-use [no use in the 365 days before the index date]) and risk of (A) UGIB, and (B) LGIB, by case-fatality and level of healthcare assistance. CI: confidence interval; LGIB: lower gastrointestinal bleed; OR: odds ratio; UGIB: upper gastrointestinal bleed.
![Figure 5. Odds ratio (95% CI) for the association between current use of low-dose aspirin (vs. non-use [no use in the 365 days before the index date]) and risk of (A) UGIB, and (B) LGIB, by case-fatality and level of healthcare assistance. CI: confidence interval; LGIB: lower gastrointestinal bleed; OR: odds ratio; UGIB: upper gastrointestinal bleed.](/cms/asset/9190c505-c133-464b-8349-14c2e43db273/iann_a_1591635_f0005_b.jpg)
Supplemental Material
Download Zip (383.2 KB)Data availability
The data supporting the results of this study are helped by the corresponding author.
